Int J Aging. 2024;2:e2.
doi: 10.34172/ija.2024.e2
Review Article
Enhanced Recovery After Surgery Protocols and Procedures in Geriatric Surgery
Ali Sharifi 1, #  , Farid Jahanshahlou 2, #
, Farid Jahanshahlou 2, #  , Ali Gol Mohammadi Senji 3
, Ali Gol Mohammadi Senji 3  , Sina Hamzezadeh 2
, Sina Hamzezadeh 2  , Mahdi Zarei 4, 5
, Mahdi Zarei 4, 5  , Mohammad-Salar Hosseini 2, 4, 5, *
, Mohammad-Salar Hosseini 2, 4, 5, * 
Author information:
1Hepatopancreaticobiliary and Organ Transplantation Surgery Group, Department of General and Vascular Surgery, Imam Reza Hospital, Tabriz University of Medical Science, Tabriz, Iran
2Research Center for Integrative Medicine in Aging, Aging Research Institute, Tabriz University of Medical Sciences, Tabriz, Iran
3Department of General and Vascular Surgery, Imam Reza Hospital, Tabriz University of Medical Science, Tabriz, Iran
4Medical Philosophy and History Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
5Research Center for Evidence-Based Medicine, Iranian EBM Center: A JBI Center of Excellence, Tabriz University of Medical Sciences, Tabriz, Iran
#Contributed equally as the first authors.
Abstract
Objectives:
To provide an inclusive overview on the applicability of ERAS protocols in geriatric surgeries.
Design:
A review study.
Participants:
Geriatric patients.
Outcome measures:
Objective and patient-reported outcomes during pre-operative, intraoperative, and post-operative periods of surgery.
Results:
Enhanced recovery after surgery (ERAS) is recognized as a revolutionary approach to postoperative care, and its importance is particularly prominent in geriatric surgery. The unique challenges caused by age-related factors and comorbidities increase the need for an appropriate approach for increasing the recovery path in elderly surgical patients. The central role of ERAS in the care of geriatric patients as well as the reduction of post-operative complications and length of hospitalization is one of its achievements.
Conclusions:
By prioritizing optimal preparation for surgery, initial mobilization, and personalized post-operative pain management, ERAS not only addresses the distinct needs of the elderly but also contributes to a paradigm shift in surgical practices.
Keywords: Aged, Enhanced recovery after surgery, Fast-track surgery, Geriatric nursing, Geriatric surgery
Copyright and License Information
© 2024 The Author(s).
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Please cite this article as follows: Sharifi A, Jahanshahlou F, Gol Mohammadi Senji A, Hamzehzadeh S, Zarei M, Hosseini MS. Enhanced recovery after surgery protocols and procedures in geriatric surgery. Int J Aging. 2024;2: e2. doi: 10.34172/ija.2024.e2
Introduction
The term “geriatric” refers to a person in the later stages of life characterized by aging and associated physiological changes. While no agreed-upon age threshold defines someone as “aged”, common indicators include people aged 65 and older.1 As the world’s population ages, a profound shift in healthcare demographics is occurring, with an increasing number of older adults requiring surgical interventions. The aging process involves various physiological changes, including changes in organ systems, cellular functions, and metabolic processes. For example, people often experience decreased muscle mass and sarcopenia, bone density changes, frailty, immune function changes, delirium, falls, and decreased organ reserve as they age.2,3 In addition, the older people are more susceptible to chronic conditions such as cardiovascular diseases, diabetes mellitus, arthritis, neurological disorders, and increased sensitivity to surgery-related stress. These factors require a suitable approach for the entire surgical procedure. It has been observed that patients with decreased physical and mental capacity have more severe post-operation complications and a higher mortality rate.4 The term frailty reflects the nature of age-related vulnerability and deterioration.5 Frailty involves dysregulation across multiple physiological systems, including the cardiovascular, musculoskeletal, and immune systems, and may be linked to cognitive decline and poor nutritional status.6 They often experience a decline in physical function and are more susceptible to stressors such as illness, surgery, or environmental changes. Screening to determine the state of frailty is based on one of the two concepts of physical frailty and frailty index, where physical frailty is caused by multi-system biological decline, and the frailty index is defined as a combination of comorbidities and social situations used to assess risk.7
Patients should not be disqualified from the surgery for being labeled as frail. Recognizing the current problems in these types of patients could result in shorter length of stay and reduce rates of readmission.8,9
Enhanced recovery after surgery (ERAS) is an evidence-based multifaceted approach that involves each stage of the surgical journey and improves various outcomes.10 Despite recent attention, the initial concepts of ERAS were presented in the 1990s.11 This multidisciplinary strategy requires a team approach, including surgery, anesthesiology, nursing, psychiatry, nutrition, physical therapy, and geriatric specialties, in which the patient plays an active role as a member. Given that ERAS has improved the outcome of patients after surgery in studies and since older patients are exposed to more risk, the study of ERAS in older patients is doubly essential. There are doubts regarding the use of ERAS in the older population due to fears of low compliance and worse outcomes.12 However, studies point to a significant reduction in complications with ERAS implementation. Some studies reported that elderly patients as well as the younger population benefit from ERAS, and underlying diseases and frailty can explain the increased risk of post-operative complications.13,14
The general goals of using ERAS in the older population are similar to those in the younger population; however, according to their unique conditions and challenges, appropriate endpoints should be defined. Accordingly, this study aimed to provide a comprehensive overview and special considerations for the applicability of ERAS protocols in geriatric surgeries.
Geriatric Surgery: General Concerns
The older patients are a heterogeneous group with different health conditions, functional abilities, and comorbidities. Aging is associated with physiological changes, including reduced organ function, altered metabolism, and reduced storage capacity, namely, physical frailty. In addition, older patients usually have several comorbidities such as cardiovascular diseases, diabetes, and respiratory problems, which, are associated with an increase in the frailty index.15 Polypharmacy is also common in geriatric patients, leading to drug interactions and potential complications.16,17 As a result, senior patients often face a higher risk of post-operative complications.18 Personalized ERAS recognizes these unique characteristics and empowers healthcare providers to optimize outcomes, accelerate recovery, and enhance the overall quality of care for elderly patients by tailoring care to each individual.
Challenges and Considerations of ERAS in Geriatric Surgeries
Implementing ERAS protocols in geriatric patients is associated with specific challenges due to age-related physiological changes and the presence of multiple comorbidities. Senior patients often show weakness characterized by decreased physiological reserve and increased vulnerability to stressful factors. Malnutrition and insufficient intake of nutrients are more common in the elderly population.19,20 Adapting ERAS protocols to accommodate frailty and individual variations in flexibility could be quite challenging. Older patients usually have several comorbidities and may take multiple medications. In geriatric patients, the risk of complications related to polypharmacy such as drug interactions and side effects requires additional caution. Geriatric patients may experience delayed recovery and rehabilitation compared to their younger counterparts.21 Therefore, setting rehabilitation plans and managing expectations about recovery speed are important considerations in older patients.
Moreover, geriatric patients are at risk of post-operative delirium,22 thus ERAS interventions, including pain management strategies and medication adjustments should be designed to minimize the risk and impact of delirium.23
Another challenge is the low adherence of the aged population to ERAS protocols.24 Elderly patients often face barriers that prevent them from fully complying with ERAS elements. Although adherence to the protocol can improve the results of ERAS protocols, patients who do not achieve complete adherence can also benefit from the partial implementation.25,26
Addressing these challenges requires a multidisciplinary approach.27 As a result, customizing ERAS protocols to meet the unique needs of geriatric patients is essential to optimize outcomes and ensure a patient-centered approach to perioperative care.
Core Components of ERAS in Geriatric Surgery
The goal of implementing the ERAS protocol is to reduce the stress caused by surgery, optimize intraoperative medical care, reduce the duration of hospitalization, accelerate the return to daily life, improve pain control, reduce complications related to immobility, and improve organ functions. The core components of ERAS could be explored in three main categories (Table 1).
Table 1.
The Core Components of the Pre-operative, Intraoperative, and Post-operative for ERAS in Geriatrics
|
Pre-operative Period
|
| Preadmission counseling |
| Multidisciplinary approach |
| Physical educational |
| Nutritional considerations |
| Psychological improvement |
| Smoking/alcohol/medication cessation |
| Comorbidity and polypharmacy management |
| Proper surgery fasting |
| Thromboprophylaxis |
| Antibiotic prophylaxis |
| Bowel preparation |
|
Intraoperative Period
|
| Less invasive surgical technique |
| Pain management and multimodal analgesia |
| Vital signs and body temperature monitoring |
| Blood glucose control |
| Fluid management |
| Aspiration prevention |
| Avoiding unnecessary drainage placement |
|
Post-operative Period
|
| Early oral feeding |
| Fluid balance and nutritional status |
| Pain management |
| Early ambulation |
| Polypharmacy management |
| Monitoring thrombotic and infectious complications |
| Delirium prevention and management |
| Avoiding nasogastric decompression |
| Early discharge and transition to care settings |
| Proper follow-up |
Note. ERAS: Enhanced recovery after surgery.
Pre-operative Period
Prehabilitation refers to the period after the diagnosis and establishment of surgical indications until before admission to the hospital and surgery.28 This includes physical, educational, nutritional, psychological, and clinical activities, the purpose of which is to improve functional capacity and the ability to adapt to stress to reduce morbidity and mortality.29 Since functional disability strongly predicts surgical outcomes, physical activity improves muscle function and cardiorespiratory capacity.30 These exercises can range from strength training and aerobics to specific exercises to areas being operated. Optimizing nutrition can improve the patient’s immune status and reduce chronic inflammation in older people.31 For patients who cannot get enough calories with oral supplements, enteral nutrition through a feeding tube should be considered if their digestive system is functioning properly. This is particularly significant in patients with cancer. Furthermore, erythropoietin and iron supplements should be considered in elderly anemic patients, especially patients with coronary artery disease, to reduce the risk of needing blood transfusion and its complications.32
Quitting smoking, alcohol, and drugs is also effective in patients’ outcomes as it has been observed that quitting smoking and alcohol for 6 to 8 weeks before elective surgery is associated with a reduction in half of the post-operative complications.33 This significant reduction could be attributed to their impact on boosting the immune status, reducing the possibility of surgical site infection, and improving wound healing and pain control. It should also be noted that quitting alcohol in older people also helps reduce the risk of delirium. Recent studies have demonstrated that pre-operative counseling sessions could reduce the discomfort and fear of the patients by providing an enhanced view of the information regarding the surgery and its potential complications.34 In addition, patients can express their preferences as active members of the therapeutic team. This is important for older patients since they can be informed of possible complications and functional disorders after surgery.
To prepare for gastrointestinal procedures, ERAS recommends avoiding routine mechanical bowel preparation as much as possible since it could affect the electrolyte balance, resulting in heart complications, surgical site infections, tissue changes in the colorectal mucosa, and digestive problems such as abdominal pain and bloating, which require greater attention regarding the vulnerability of older patients.35,36 Moreover, this process is poorly tolerated by patients and, in some cases, requires hospitalization before surgery and can be time-consuming and costly.
Regarding pre-operative fasting, recent studies have indicated that instead of the traditional fasting schemes with fasting for 8-12 hours and no drinking for 4-6 hours, patients could only undergo a six-hour fasting and a two-hour limitation for clear liquids before the surgery, which would ultimately result in reduced hunger and thirst and higher post-surgical satisfaction.37 Operating patients influenced by insulin after carbohydrate load has been associated with a decrease in glucagon secretion, cancellation of cortisol secretion, and, as a result, less catabolic in the post-operative period.38,39
Considering that surgical site infection is the most common complication after surgery, the use of prophylactic antibiotics plays an essential role in reducing hospitalization time, treatment costs, complications, and mortality.40
Intraoperative Period
Different measures can improve the surgical outcomes of geriatric patients during the intraoperative period. If possible, it is essential to use a minimally invasive surgical technique to reduce the duration of hospitalization and post-operative complications. It should be noted that the recovery process is slower in geriatric patients. Implementing multimodal analgesia by combining different classes of analgesics with different mechanisms of action results in minimal reliance on opioids and reduces the risk of drug-related complications such as respiratory depression and constipation.41 Moreover, the use of regional anesthetic techniques such as epidurals or peripheral nerve blocks helps manage pain and minimize the need for opioids effectively.42 This technique is beneficial for minimizing post-operative pain and facilitating early movement. It is recommended to avoid using drainage when possible due to its effect on reducing fluid loss, reducing the risk of infection, and faster recovery of the surgical site. It also adversely affects the patients’ satisfaction, earlier mobilization, and length of hospitalization.43
Recent studies have documented that perioperative blood sugar control and maintaining blood sugar in the normal range are important factors in preventing surgical site infection.44,45 Using heating devices to prevent mild hypothermia and regulatory vasoconstriction plays a role in reducing wound infection.46 It also helps reduce catabolism and blood loss, thus reducing the risk of cardiovascular complications and the need for blood transfusion. Considering the greater vulnerability of geriatric patients to cardiac and renal accidents, intraoperative fluid therapy, maintaining hydration, and euvolemia, according to the patient’s cardiac conditions, are of greater importance. Additionally, paying attention to aspiration and its complications is another issue that should be considered.
Post-operative Period
ERAS contributes to a holistic approach to post-operative complications and symptoms. Pain management is one of the most critical points of the post-operative period.47 Proper pain management is associated with faster patient mobilization and increased satisfaction.48 Multimodal analgesia strategies to control pain and, at the same time, minimize the use of opioids and their consequent side effects are essential in this regard. Meanwhile, attention should be paid to polypharmacy and drug interactions in geriatric patients. Patient-controlled analgesia systems allow elderly patients to self-administer pain medication within predetermined safety limits, leading to the empowerment of patients.49
An early oral diet is critical post-operative care since it preserves the health and function of the digestive system, maintains nutritional status, maintains proper control of fluids and electrolyte balance, and increases insulin sensitivity and proper control of blood glucose.50 In general, it helps the patient recover faster and more comfortably; however, the decision in this case should be based on the patient’s condition. Monitoring fluid balance and nutritional status after surgery according to individual needs is another challenge for geriatric patients.
Early mobilization is another vital issue after surgery. Early mobilization improves digestive, musculoskeletal, and cardiorespiratory function, reduces the chances of thrombotic complications, and generally accelerates returning to everyday life and discharge.51 However, according to the physical condition of each older adult, this case may require special supervision and perhaps more effort by health workers.52
Avoiding nasogastric decompression and early removal of urinary catheters, among other things, improves patient satisfaction and mental status, prevents possible complications such as infection, and helps in early mobilization and early discharge, which should be decided according to each individual’s conditions.53
Moreover, collaboration with patients and caregivers should ensure a safe and coordinated transition to home or another care setting. Post-operative care, medications, side effects, and the importance of adherence to rehabilitation programs are issues that must be entirely taught to patients and caregivers. Additionally, the communication method to contact in case of concern and to monitor the patient’s progress follow-up appointments should be considered remotely if possible.54,55
Benefits of ERAS Protocol in Geriatric Surgery
Recent studies have unveiled the potential benefits of implementing ERAS protocols in geriatric surgeries and their positive impact on surgical outcomes, the reduction of post-surgery complications, and reduction in the re-hospitalization of the patients.56,57 Although the rate of complications and re-hospitalization has been reported to be higher than that in young people in some studies, in the studies conducted, this rate was lower in older people compared to traditional protocols.58
Faster recovery speed, shorter intensive care unit (ICU) length of stay, and shorter length of hospitalization have been observed among geriatric patients following the ERAS protocols.59,60 However, it should be noted that in the case of geriatric patients, simply filling out the discharge criteria is insufficient, and proper post-discharge care should also be provided.55,61,62 The lack of provision of this care can increase the length of hospitalization. Additionally, in case of insufficient care, the possibility of complications and re-hospitalization also significantly increased.63,64
ERAS has also been more successful in controlling the patients’ pain, which can be attributed to the use of multimodal analgesic methods such as non-opioid anesthesia and analgesia, regional anesthesia, and limiting the use of opioids, considering the susceptibility of older patients to its side effects such as respiratory depression, aspiration, cognitive disorders, and constipation.65,66 In the case of post-operative ileus, using less invasive surgical techniques such as laparoscopy, reducing the use of opioids, maintaining the electrolyte balance, starting nutrition earlier, and early mobilization were found helpful.
ERAS plays a fundamental role in reducing the rate of prevalent geriatric surgery complications, including delirium, life-threatening thrombotic events such as deep vein thrombosis, pulmonary embolism, and hemodynamic instability.67,68 In addition, ERAS advocates multifaceted approaches to pain management, often including the limited use of opioids, in addition to early action to minimize their associated risks such as increased thrombotic potential. Adequate hydration, proper nutritional support, and integral components of ERAS help maintain optimal blood viscosity and prevent thrombotic complications.69,70 ERAS has also been more cost-effective than traditional methods by improving pre- and post-operative care, including reducing the need for ICU, reducing the length of hospitalization, reducing the need for expensive drugs such as opioids, and decreasing post-operative complications. Today, with the increase in the elderly population and the increase in the level of care expectations, economic considerations also seem more significant than before.71
Overall, studies showed that ERAS protocols provide safe and cost-effective modifications to geriatric surgeries, and as with the younger population, implementing these protocols is associated with reduced surgical stress and morbidity. Figure 1 summarizes the benefits and barriers of ERAS protocols in geriatric surgery.
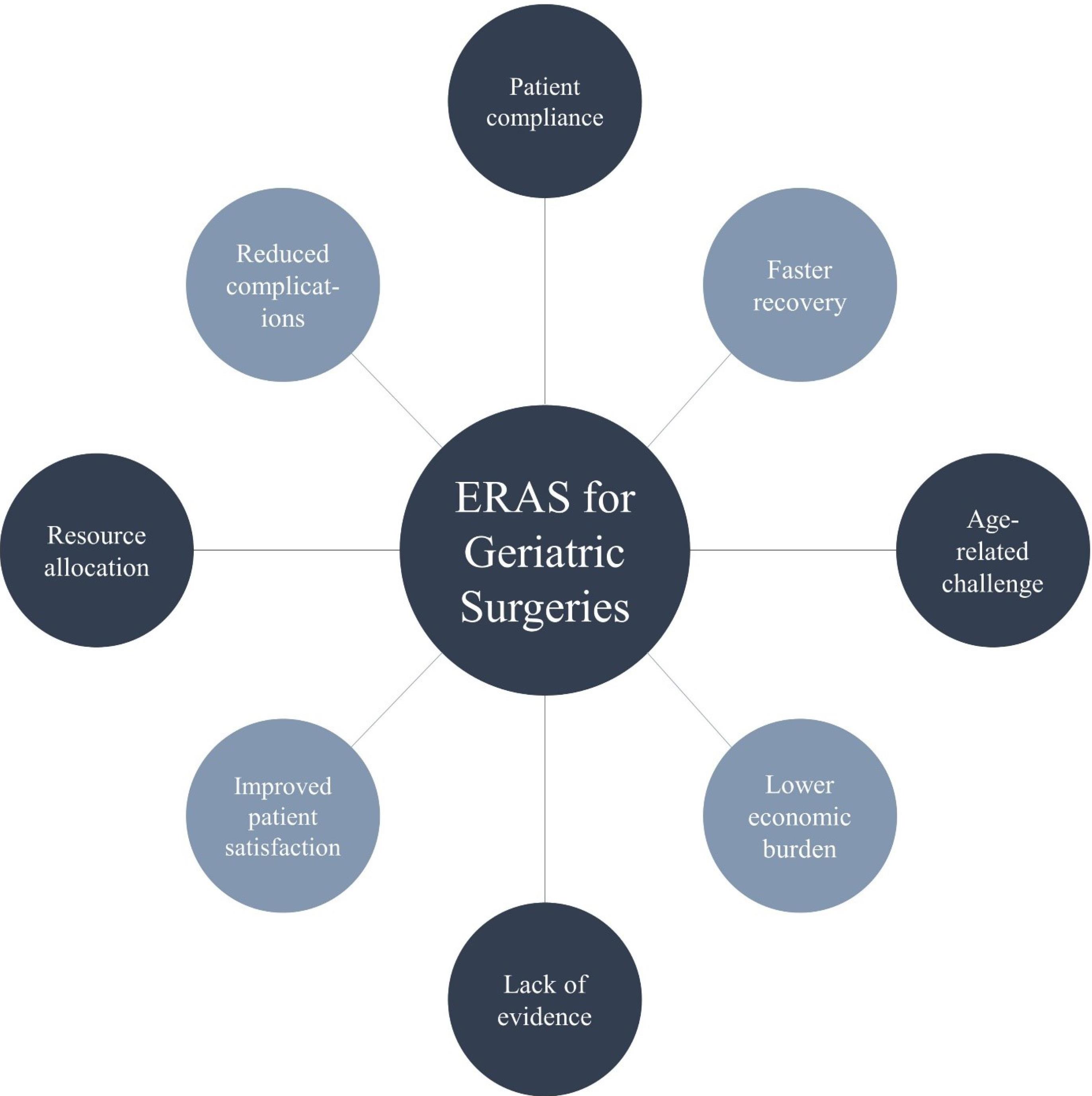
Figure 1.
Benefits and Barriers of Implementing ERAS Protocols in Geriatric Surgery. Note. ERAS: Enhanced recovery after surgery. The benefits are presented in gray and the barriers are presented in dark circles
.
Benefits and Barriers of Implementing ERAS Protocols in Geriatric Surgery. Note. ERAS: Enhanced recovery after surgery. The benefits are presented in gray and the barriers are presented in dark circles
Future Directions and Innovations
Integrating telehealth for pre-operative assessments, risk assessment discussion of surgical procedures, and discussion of patient preferences and expectations effectively increases access and convenience for older patients.72,73 Furthermore, post-operative tele-follow-ups can increase continuity of care and reduce unnecessary hospital visits. Such services include virtual appointments to assess recovery progress, manage medications, address concerns, and conduct even remote rehabilitation and remote monitoring of chronic conditions.74 The progress achieved in artificial intelligence algorithms can help predict surgical results, identify patients at higher risk for complications, and adjust post-operative care programs based on individual patient characteristics.75
Conclusions
Implementing ERAS protocols in the older population is a critical paradigm for optimizing peri-operative care. The challenges presented by age-related complexities, comorbidities, and diverse functional reserves emphasize the importance of designing ERAS protocols to meet the unique needs of elderly surgical patients. Emphasizing early mobilization, multimodal pain management, and individualized nutritional support, ERAS seeks to improve post-operative recovery and addresses specific vulnerabilities associated with aging. Implications for the future of geriatric surgery are refining and personalizing ERAS approaches, integrating technological advances, and adopting a multidisciplinary model that accounts for the diverse health profiles in the geriatric population. Recognizing the need to adapt ERAS principles to the complexities of geriatric care paves the way for improved outcomes, reduced complications, and a more patient-centered approach to surgery in geriatric patients.
Acknowledgements
We would like to appreciate the support of the Clinical Research Development Unit, Imam Reza General Hospital (Tabriz, Iran) in conducting this research.
Author contributions
Conceptualization: Ali Sharifi, Mohammad-Salar Hosseini.
Data curation: Ali Sharifi, Farid Jahanshahlou, Ali Gol Mohammadi Senji, Mahdi Zarei.
Investigation: Ali Sharifi, Farid Jahanshahlou, Ali Gol Mohammadi Senji, Mahdi Zarei.
Visualization: Sina Hamzehzadeh, Mohammad-Salar Hosseini.
Writing–original draft: Farid Jahanshahlou, Ali Gol Mohammadi Senji, Sina Hamzehzadeh.
Writing–review & editing: Ali Sharifi, Mahdi Zarei, Mohammad-Salar Hosseini.
Funding
None.
Data availability statement
This article contains all data produced or analyzed during this investigation.
Ethical approval
Not applicable.
Consent for publication
Not applicable.
Conflict of interests
The authors declare no conflict of interests.
References
- Araj-Khodaei M, Sanaie S, Nejadghaderi SA, Sullman MJ, Samei-Sis S, Taheri-Targhi S. Profile of Tabriz Older People Health Survey (TOPS-2019): a representative community-based cross-sectional study. Sci Rep 2022; 12(1):17879. doi: 10.1038/s41598-022-22710-2 [Crossref] [ Google Scholar]
- Agresta F, Bergamini C, Podda M, Campanile FC, Anania G, Volpato S, et al. How to define an elderly and frail patient? In: Agresta F, Podda M, Campanile FC, Bergamini C, Anania G, eds. Emergency Laparoscopic Surgery in the Elderly and Frail Patient. Cham: Springer; 2021. p. 3-18. 10.1007/978-3-030-79990-8_1.
- Akbarzadeh MA, Hosseini MS. Is COVID-19 really a geriatric syndrome?. Ageing Res Rev 2022; 79:101657. doi: 10.1016/j.arr.2022.101657 [Crossref] [ Google Scholar]
- Artiles-Armas M, Roque-Castellano C, Conde-Martel A, Marchena-Gómez J. The comprehensive complication index is related to frailty in elderly surgical patients. J Surg Res 2019; 244:218-24. doi: 10.1016/j.jss.2019.06.011 [Crossref] [ Google Scholar]
- Rohrmann S. Epidemiology of frailty in older people. In: Veronese N, ed. Frailty and Cardiovascular Diseases: Research into an Elderly Population. Cham: Springer; 2020. p. 21-7. 10.1007/978-3-030-33330-0_3.
- Xia F, Zhang J, Meng S, Qiu H, Guo F. Association of frailty with the risk of mortality and resource utilization in elderly patients in intensive care units: a meta-analysis. Front Med (Lausanne) 2021; 8:637446. doi: 10.3389/fmed.2021.637446 [Crossref] [ Google Scholar]
- Fried LP, Cohen AA, Xue QL, Walston J, Bandeen-Roche K, Varadhan R. The physical frailty syndrome as a transition from homeostatic symphony to cacophony. Nat Aging 2021; 1(1):36-46. doi: 10.1038/s43587-020-00017-z [Crossref] [ Google Scholar]
- Engelhardt KE, Reuter Q, Liu J, Bean JF, Barnum J, Shapiro MB. Frailty screening and a frailty pathway decrease length of stay, loss of independence, and 30-day readmission rates in frail geriatric trauma and emergency general surgery patients. J Trauma Acute Care Surg 2018; 85(1):167-73. doi: 10.1097/ta.0000000000001931 [Crossref] [ Google Scholar]
- Wang YC, Liang CK, Chou MH, Chiu CF, Lin HC, Hsu YH. The effectiveness of frailty intervention for older patients with frailty during hospitalization. J Nutr Health Aging 2023; 27(6):413-20. doi: 10.1007/s12603-023-1924-y [Crossref] [ Google Scholar]
- Melnyk M, Casey RG, Black P, Koupparis AJ. Enhanced recovery after surgery (ERAS) protocols: time to change practice?. Can Urol Assoc J 2011; 5(5):342-8. doi: 10.5489/cuaj.11002 [Crossref] [ Google Scholar]
- Bardram L, Funch-Jensen P, Jensen P, Crawford ME, Kehlet H. Recovery after laparoscopic colonic surgery with epidural analgesia, and early oral nutrition and mobilisation. Lancet 1995; 345(8952):763-4. doi: 10.1016/s0140-6736(95)90643-6 [Crossref] [ Google Scholar]
- Kehlet H. Enhanced Recovery After Surgery (ERAS): good for now, but what about the future?. Can J Anaesth 2015; 62(2):99-104. doi: 10.1007/s12630-014-0261-3 [Crossref] [ Google Scholar]
- Ljungqvist O, Hubner M. Enhanced recovery after surgery-ERAS-principles, practice and feasibility in the elderly. Aging Clin Exp Res 2018; 30(3):249-52. doi: 10.1007/s40520-018-0905-1 [Crossref] [ Google Scholar]
- Jasper E, Dhesi J, Partridge J. Delivering perioperative care for older patients undergoing cancer surgery. In: Hagberg C, Gottumukkala V, Riedel B, Nates J, Buggy D, eds. Perioperative Care of the Cancer Patient. New Delhi: Elsevier; 2023. p. 409-16. 10.1016/b978-0-323-69584-8.00036-0.
- Safiri S, Motlagh Asghari K, Sullman MJ. The global burden of diseases and injuries among older adults. Int J Aging 2023; 1(1):e16. doi: 10.34172/ija.2023.e16 [Crossref] [ Google Scholar]
- Lertkovit S, Siriussawakul A, Suraarunsumrit P, Lertpipopmetha W, Manomaiwong N, Wivatdechakul W. Polypharmacy in older adults undergoing major surgery: prevalence, association with postoperative cognitive dysfunction and potential associated anesthetic agents. Front Med (Lausanne) 2022; 9:811954. doi: 10.3389/fmed.2022.811954 [Crossref] [ Google Scholar]
- Nagai S, Inagaki R, Michikawa T, Kawabata S, Ito K, Hachiya K. Efficacy of surgical treatment on polypharmacy of elderly patients with lumbar spinal canal stenosis: retrospective exploratory research. BMC Geriatr 2023; 23(1):169. doi: 10.1186/s12877-023-03853-x [Crossref] [ Google Scholar]
- Arends BC, Blussé van Oud-Alblas HJ, Vernooij LM, Verwijmeren L, Biesma DH, Knibbe CAJ. The association of polypharmacy with functional decline in elderly patients undergoing cardiac surgery. Br J Clin Pharmacol 2022; 88(5):2372-9. doi: 10.1111/bcp.15174 [Crossref] [ Google Scholar]
- Norman K, Haß U, Pirlich M. Malnutrition in older adults-recent advances and remaining challenges. Nutrients 2021; 13(8):2764. doi: 10.3390/nu13082764 [Crossref] [ Google Scholar]
- Dent E, Wright ORL, Woo J, Hoogendijk EO. Malnutrition in older adults. Lancet 2023; 401(10380):951-66. doi: 10.1016/s0140-6736(22)02612-5 [Crossref] [ Google Scholar]
- Tillou A, Kelley-Quon L, Burruss S, Morley E, Cryer H, Cohen M. Long-term postinjury functional recovery: outcomes of geriatric consultation. JAMA Surg 2014; 149(1):83-9. doi: 10.1001/jamasurg.2013.4244 [Crossref] [ Google Scholar]
- Schenning KJ, Deiner SG. Postoperative delirium in the geriatric patient. Anesthesiol Clin 2015; 33(3):505-16. doi: 10.1016/j.anclin.2015.05.007 [Crossref] [ Google Scholar]
- Wang C, Tan B, Qian Q. The impact of perioperative enhanced recovery nursing model on postoperative delirium and rehabilitation quality in elderly patients with femoral neck fractures. BMC Musculoskelet Disord 2023; 24(1):947. doi: 10.1186/s12891-023-07068-4 [Crossref] [ Google Scholar]
- Fagard K, Wolthuis A, D’Hoore A, Verhaegen M, Tournoy J, Flamaing J. A systematic review of the intervention components, adherence and outcomes of enhanced recovery programmes in older patients undergoing elective colorectal surgery. BMC Geriatr 2019; 19(1):157. doi: 10.1186/s12877-019-1158-3 [Crossref] [ Google Scholar]
- Pisarska M, Pędziwiatr M, Małczak P, Major P, Ochenduszko S, Zub-Pokrowiecka A. Do we really need the full compliance with ERAS protocol in laparoscopic colorectal surgery? A prospective cohort study. Int J Surg 2016; 36(Pt A):377-82. doi: 10.1016/j.ijsu.2016.11.088 [Crossref] [ Google Scholar]
- Wang D, Liu Z, Zhou J, Yang J, Chen X, Chang C. Barriers to implementation of enhanced recovery after surgery (ERAS) by a multidisciplinary team in China: a multicentre qualitative study. BMJ Open 2022; 12(3):e053687. doi: 10.1136/bmjopen-2021-053687 [Crossref] [ Google Scholar]
- Millan M. Enhanced recovery after surgery in elderly and high-risk patients. Ann Laparosc Endosc Surg 2020; 5:39. doi: 10.21037/ales.2020.02.05 [Crossref] [ Google Scholar]
- Gillis C, Ljungqvist O, Carli F. Prehabilitation, enhanced recovery after surgery, or both? A narrative review. Br J Anaesth 2022; 128(3):434-48. doi: 10.1016/j.bja.2021.12.007 [Crossref] [ Google Scholar]
- Koh FH, Loh CH, Tan WJ, Ho LML, Yen D, Chua JMW. Structured presurgery prehabilitation for aged patients undergoing elective surgery significantly improves surgical outcomes and reduces cost: a nonrandomized sequential comparative prospective cohort study. Nutr Clin Pract 2022; 37(3):645-53. doi: 10.1002/ncp.10787 [Crossref] [ Google Scholar]
- Fernández-Costa D, Gómez-Salgado J, Castillejo Del Río A, Borrallo-Riego Á, Guerra-Martín MD. Effects of prehabilitation on functional capacity in aged patients undergoing cardiothoracic surgeries: a systematic review. Healthcare (Basel) 2021; 9(11):1602. doi: 10.3390/healthcare9111602 [Crossref] [ Google Scholar]
- Martínez-Ortega AJ, Piñar-Gutiérrez A, Serrano-Aguayo P, González-Navarro I, Remón-Ruíz PJ, Pereira-Cunill JL. Perioperative nutritional support: a review of current literature. Nutrients 2022; 14(8):1601. doi: 10.3390/nu14081601 [Crossref] [ Google Scholar]
- Seong JY, Shin DY, Byun JM, Koh Y, Hong J, Kim I. Serum Erythropoietin level in anemia of elderly with unclear etiology. Sci Rep 2023; 13(1):15902. doi: 10.1038/s41598-023-42806-7 [Crossref] [ Google Scholar]
- Iqbal U, Green JB, Patel S, Tong Y, Zebrower M, Kaye AD. Preoperative patient preparation in enhanced recovery pathways. J Anaesthesiol Clin Pharmacol 2019; 35(Suppl 1):S14-23. doi: 10.4103/joacp.JOACP_54_18 [Crossref] [ Google Scholar]
- Akkamahadevi P, Subramanian VV. The efficacy of different methods of pre-operative counselling on perioperative anxiety in patients undergoing regional anaesthesia. Indian J Anaesth 2016; 60(1):58-60. doi: 10.4103/0019-5049.174812 [Crossref] [ Google Scholar]
- Ju YU, Min BW. A review of bowel preparation before colorectal surgery. Ann Coloproctol 2021; 37(2):75-84. doi: 10.3393/ac.2020.04.01 [Crossref] [ Google Scholar]
- Yue Y, Chen X, Wang H, Cheng M, Zheng B. Mechanical bowel preparation combined with oral antibiotics reduces infectious complications and anastomotic leak in elective colorectal surgery: a pooled-analysis with trial sequential analysis. Int J Colorectal Dis 2023; 38(1):5. doi: 10.1007/s00384-022-04302-8 [Crossref] [ Google Scholar]
- He Y, Wang R, Wang F, Chen L, Shang T, Zheng L. The clinical effect and safety of new preoperative fasting time guidelines for elective surgery: a systematic review and meta-analysis. Gland Surg 2022; 11(3):563-75. doi: 10.21037/gs-22-49 [Crossref] [ Google Scholar]
- Duggan EW, Carlson K, Umpierrez GE. Perioperative hyperglycemia management: an update. Anesthesiology 2017; 126(3):547-60. doi: 10.1097/aln.0000000000001515 [Crossref] [ Google Scholar]
- Janssen J. New insights into the role of insulin and hypothalamic-pituitary-adrenal (HPA) axis in the metabolic syndrome. Int J Mol Sci 2022; 23(15):8178. doi: 10.3390/ijms23158178 [Crossref] [ Google Scholar]
- Habteweld HA, Yimam M, Tsige AW, Wondmkun YT, Endalifer BL, Ayenew KD. Surgical site infection and antimicrobial prophylaxis prescribing profile, and its determinants among hospitalized patients in Northeast Ethiopia: a hospital based cross-sectional study. Sci Rep 2023; 13(1):14689. doi: 10.1038/s41598-023-41834-7 [Crossref] [ Google Scholar]
- Schwenk ES, Mariano ER. Designing the ideal perioperative pain management plan starts with multimodal analgesia. Korean J Anesthesiol 2018; 71(5):345-52. doi: 10.4097/kja.d.18.00217 [Crossref] [ Google Scholar]
- Mancel L, Van Loon K, Lopez AM. Role of regional anesthesia in Enhanced Recovery After Surgery (ERAS) protocols. Curr Opin Anaesthesiol 2021; 34(5):616-25. doi: 10.1097/aco.0000000000001048 [Crossref] [ Google Scholar]
- Miyazaki T, Nagayasu T. No drain policy for “ultimate” enhanced recovery after surgery. J Thorac Dis 2019; 11(Suppl 15):S1900-2. doi: 10.21037/jtd.2019.08.46 [Crossref] [ Google Scholar]
- Lai J, Li Q, He Y, Zou S, Bai X, Rastogi S. Glycemic control regimens in the prevention of surgical site infections: a meta-analysis of randomized clinical trials. Front Surg 2022; 9:855409. doi: 10.3389/fsurg.2022.855409 [Crossref] [ Google Scholar]
- Ata A, Lee J, Bestle SL, Desemone J, Stain SC. Postoperative hyperglycemia and surgical site infection in general surgery patients. Arch Surg 2010; 145(9):858-64. doi: 10.1001/archsurg.2010.179 [Crossref] [ Google Scholar]
- Bu N, Zhao E, Gao Y, Zhao S, Bo W, Kong Z. Association between perioperative hypothermia and surgical site infection: a meta-analysis. Medicine (Baltimore) 2019; 98(6):e14392. doi: 10.1097/md.0000000000014392 [Crossref] [ Google Scholar]
- Nasir F, Hyder Z, Kasraianfard A, Sharifi A, Chavoshi Khamneh A, Zarghami SY. Enhanced recovery after hepatopancreaticobiliary surgery: a single-center case control study. Ann Hepatobiliary Pancreat Surg 2021; 25(1):97-101. doi: 10.14701/ahbps.2021.25.1.97 [Crossref] [ Google Scholar]
- Cheung CK, Adeola JO, Beutler SS, Urman RD. Postoperative pain management in enhanced recovery pathways. J Pain Res 2022; 15:123-35. doi: 10.2147/jpr.s231774 [Crossref] [ Google Scholar]
- Motamed C. Clinical update on patient-controlled analgesia for acute postoperative pain. Pharmacy (Basel) 2022; 10(1):22. doi: 10.3390/pharmacy10010022 [Crossref] [ Google Scholar]
- Hao T, Liu Q, Lv X, Qiu J, Zhang HR, Jiang HP. Efficacy and safety of early oral feeding in postoperative patients with upper gastrointestinal tumor: a systematic review and meta-analysis. World J Gastrointest Surg 2021; 13(7):717-33. doi: 10.4240/wjgs.v13.i7.717 [Crossref] [ Google Scholar]
- Wang P, Wang Q, Kong C, Teng Z, Li Z, Zhang S. Enhanced recovery after surgery (ERAS) program for elderly patients with short-level lumbar fusion. J Orthop Surg Res 2020; 15(1):299. doi: 10.1186/s13018-020-01814-3 [Crossref] [ Google Scholar]
- Surkan MJ, Gibson W. Interventions to mobilize elderly patients and reduce length of hospital stay. Can J Cardiol 2018; 34(7):881-8. doi: 10.1016/j.cjca.2018.04.033 [Crossref] [ Google Scholar]
- Millan M, Renau-Escrig AI. Minimizing the impact of colorectal surgery in the older patient: the role of enhanced recovery programs in older patients. Eur J Surg Oncol 2020; 46(3):338-43. doi: 10.1016/j.ejso.2019.12.018 [Crossref] [ Google Scholar]
- Rauwerdink A, Jansen M, de Borgie C, Bemelman WA, Daams F, Schijven MP. Improving enhanced recovery after surgery (ERAS): ERAS APPtimize study protocol, a randomized controlled trial investigating the effect of a patient-centred mobile application on patient participation in colorectal surgery. BMC Surg 2019; 19(1):125. doi: 10.1186/s12893-019-0588-3 [Crossref] [ Google Scholar]
- Takchi R, Williams GA, Brauer D, Stoentcheva T, Wolf C, Van Anne B. Extending enhanced recovery after surgery protocols to the post-discharge setting: a phone call intervention to support patients after expedited discharge after pancreaticoduodenectomy. Am Surg 2020; 86(1):42-8. [ Google Scholar]
- Pędziwiatr M, Mavrikis J, Witowski J, Adamos A, Major P, Nowakowski M. Current status of enhanced recovery after surgery (ERAS) protocol in gastrointestinal surgery. Med Oncol 2018; 35(6):95. doi: 10.1007/s12032-018-1153-0 [Crossref] [ Google Scholar]
- Meillat H, Braticevic C, Zemmour C, Brun C, Cécile M, Faucher M. Real-world implementation of a geriatric-specific ERAS protocol in patients undergoing colonic cancer surgery. Eur J Surg Oncol 2021; 47(5):1012-8. doi: 10.1016/j.ejso.2020.11.128 [Crossref] [ Google Scholar]
- Ayaz T, Sahin SB, Sahin OZ, Bilir O, Rakıcı H. Factors affecting mortality in elderly patients hospitalized for nonmalignant reasons. J Aging Res 2014; 2014:584315. doi: 10.1155/2014/584315 [Crossref] [ Google Scholar]
- Brinson Z, Tang VL, Finlayson E. Postoperative functional outcomes in older adults. Curr Surg Rep 2016; 4(6):21. doi: 10.1007/s40137-016-0140-7 [Crossref] [ Google Scholar]
- Li J, Zhao F, Gao J, Dong W, Yu X, Zhu C. Enhanced recovery after surgery (ERAS) protocol in geriatric patients underwent unicompartmental knee arthroplasty: a retrospective cohort study. Medicine (Baltimore) 2023; 102(6):e32941. doi: 10.1097/md.0000000000032941 [Crossref] [ Google Scholar]
- Ljungqvist O, de Boer HD. Enhanced recovery after surgery and elderly patients: advances. Anesthesiol Clin 2023; 41(3):647-55. doi: 10.1016/j.anclin.2023.02.010 [Crossref] [ Google Scholar]
- Jiang W, Mao Q, Xie Y, Ying H, Xu H, Ge H. Enhanced recovery after surgery (ERAS) program in elderly patients undergoing laparoscopic hepatectomy: a retrospective cohort study. Transl Cancer Res 2020; 9(8):4563-72. doi: 10.21037/tcr-19-2884 [Crossref] [ Google Scholar]
- Bagnall NM, Malietzis G, Kennedy RH, Athanasiou T, Faiz O, Darzi A. A systematic review of enhanced recovery care after colorectal surgery in elderly patients. Colorectal Dis 2014; 16(12):947-56. doi: 10.1111/codi.12718 [Crossref] [ Google Scholar]
- Zhou B, Ji H, Liu Y, Chen Z, Zhang N, Cao X. ERAS reduces postoperative hospital stay and complications after bariatric surgery: a retrospective cohort study. Medicine (Baltimore) 2021; 100(47):e27831. doi: 10.1097/md.0000000000027831 [Crossref] [ Google Scholar]
- Chau DL, Walker V, Pai L, Cho LM. Opiates and elderly: use and side effects. Clin Interv Aging 2008; 3(2):273-8. doi: 10.2147/cia.s1847 [Crossref] [ Google Scholar]
- Gazelka HM, Leal JC, Lapid MI, Rummans TA. Opioids in older adults: indications, prescribing, complications, and alternative therapies for primary care. Mayo Clin Proc 2020; 95(4):793-800. doi: 10.1016/j.mayocp.2020.02.002 [Crossref] [ Google Scholar]
- Zhu R, Yang F, Li C, Zhu H, Lin L, Zhao X. Effect of enhanced recovery after surgery on the prognosis of patients with hip fractures: a systematic review and meta-analysis. J Trauma Nurs 2023; 30(5):271-81. doi: 10.1097/jtn.0000000000000741 [Crossref] [ Google Scholar]
- Liu Z, Zhang J, He K, Zhang Y, Zhang Y. Optimized clinical practice for superaged patients with hip fracture: significance of damage control and enhanced recovery program. Burns Trauma 2019; 7:21. doi: 10.1186/s41038-019-0159-y [Crossref] [ Google Scholar]
- Naghedi-Baghdar H, Nazari SM, Taghipour A, Nematy M, Shokri S, Mehri MR. Effect of diet on blood viscosity in healthy humans: a systematic review. Electron Physician 2018; 10(3):6563-70. doi: 10.19082/6563 [Crossref] [ Google Scholar]
- Lei J, Huang K, Dai Y, Yin G. Evaluating outcomes of patient-centered enhanced recovery after surgery (ERAS) in percutaneous nephrolithotomy for staghorn stones: an initial experience. Front Surg 2023; 10:1138814. doi: 10.3389/fsurg.2023.1138814 [Crossref] [ Google Scholar]
- Tang B, Li Z, Hu S, Xiong J. Economic implications of health care burden for elderly population. Inquiry 2022; 59:469580221121511. doi: 10.1177/00469580221121511 [Crossref] [ Google Scholar]
- Hosseini MS, Jahanshahlou F, Gol Mohammadi Senji A. The necessity of integrating telehealth into surgical oncology practice. Int J Surg Open 2023; 56:100643. doi: 10.1016/j.ijso.2023.100643 [Crossref] [ Google Scholar]
- Eamer G, Al-Amoodi MJ, Holroyd-Leduc J, Rolfson DB, Warkentin LM, Khadaroo RG. Review of risk assessment tools to predict morbidity and mortality in elderly surgical patients. Am J Surg 2018; 216(3):585-94. doi: 10.1016/j.amjsurg.2018.04.006 [Crossref] [ Google Scholar]
- Cremades M, Ferret G, Parés D, Navinés J, Espin F, Pardo F. Telemedicine to follow patients in a general surgery department A randomized controlled trial. Am J Surg 2020; 219(6):882-7. doi: 10.1016/j.amjsurg.2020.03.023 [Crossref] [ Google Scholar]
- Leinert C, Fotteler M, Kocar TD, Dallmeier D, Kestler HA, Wolf D. Supporting SURgery with GEriatric Co-Management and AI (SURGE-Ahead): a study protocol for the development of a digital geriatrician. PLoS One 2023; 18(6):e0287230. doi: 10.1371/journal.pone.0287230 [Crossref] [ Google Scholar]