Int J Aging. 2024;2:e13.
doi: 10.34172/ija.2024.e13
Review Article
Liver Cancer in the Middle East and North Africa: Epidemiology, Trends, and Risk Factors
Mohammad-Salar Hosseini 1  , Manouchehr Khoshbaten 2
, Manouchehr Khoshbaten 2  , Ali-Asghar Kolahi 3
, Ali-Asghar Kolahi 3  , Saeid Safiri 1, *
, Saeid Safiri 1, * 
Author information:
1Social Determinants of Health Research Center, Department of Community Medicine, Faculty of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
2Liver and Gastrointestinal Diseases Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
3Social Determinants of Health Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Abstract
Objectives:
Considering the growing concerns about the rising incidence of this cancer in the Middle East and North Africa (MENA), this literature review presents the local epidemiology and trends of liver cancer, along with a practical estimation of its epidemiology and contributing risk factors.
Design:
Review Article.
Setting(s):
Middle East and North Africa.
Outcome measures:
MEDLINE (via PubMed), Scopus, and Web of Science databases, as well as Google Scholar, were searched up to September 2024 using representative keywords and MeSH terms. Studies reporting the epidemiology of liver and intrahepatic cholangiocarcinoma in the region or an analysis of the contributing infectious diseases, non-communicable disorders, genetic predispositions, behavioral aspects, and environmental factors were included. A qualitative synthesis was performed, and the results were presented using thematic narrative synthesis.
Results:
Liver cancer, particularly hepatocellular carcinoma (HCC), is rapidly growing in the MENA region, driven by a combination of viral hepatitis, underlying metabolic disorders, and environmental exposures. Liver cancer epidemiology varies across the region, with countries like Egypt historically burdened by hepatitis C, while Gulf states experience rising cases linked to metabolic disorders. Projections indicate a continued increase in the incidence of liver cancer due to the ongoing obesity and diabetes epidemics.
Conclusions:
Despite the success of viral hepatitis management campaigns in some countries, the region faces significant challenges in controlling the rising burden of liver cancer related to metabolic disorders. Prevention strategies should focus on lifestyle and dietary interventions, alongside the need for improved cancer registries, better data collection, and policy reforms. A multidisciplinary approach, combining public health initiatives and targeted healthcare improvements, is essential to reduce regional liver cancer incidence and improve outcomes.
Keywords: Epidemiology, Gulf region, Hepatocellular carcinoma, Liver neoplasms viral hepatitis
Copyright and License Information
© 2024 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
This study is part of a project funded by the Social Determinants of Health Research Center at Tabriz University of Medical Sciences in Tabriz, Iran (Grant Number: 69744).
Please cite this article as follows: Hosseini MS, Khoshbaten M, Kolahi AA, Safiri S. Liver cancer in the Middle East and North Africa: epidemiology, trends, and risk factors. Int J Aging. 2024;2: e13. doi: 10.34172/ija.2024.e13
Introduction
Liver cancer is a major health issue, representing nearly half of the global morbidity and mortality from cancer. Primary liver cancer includes hepatocellular carcinoma (HCC), intrahepatic cholangiocarcinoma, and rare forms such as hepatoblastoma.1 Among these types, HCC is the dominant form, responsible for around four out of every five cases of primary liver cancer.2 Intrahepatic cholangiocarcinoma, which originates from the biliary ducts in the liver, represents a smaller proportion, while hepatoblastoma is usually limited to pediatric cases.3
Following lung and colorectal cancers, liver cancer is the third cause of cancer-associated mortalities worldwide and the sixth most recorded malignancy in terms of diagnoses.4,5 According to the World Health Organization (WHO) report in 2020, 830 000 people died of liver cancer.5 The distribution of liver cancer cases is not uniform across regions; in other words, East and Southeast Asia, as well as sub-Saharan Africa, exhibit the greatest incidence rates.6 This geographic variation is primarily driven by the dominance of chronic hepatitis B virus (HBV) and hepatitis C virus (HCV) infections in these regions. However, the global epidemiological landscape is shifting, with liver cancer emerging as a growing concern in other nations, especially the Middle East and Eastern Mediterranean region, mainly due to rising rates of obesity, diabetes, and metabolic dysfunction-associated fatty liver disease (MAFLD).7-9 In light of these changing trends, this paper reviews the current and forthcoming burden of liver cancer, epidemiology trends, and contributing risk factors in the MENA region.
Methods
An extended review was conducted, retrieving all related evidence from MEDLINE (via PubMed), Web of Science, Scopus, and Google Scholar up to September 2024, using keywords and MeSH terms related to liver neoplasms, hepatocellular carcinoma, cholangiocarcinoma, intrahepatic bile duct (IBD) cancer, incidence, mortality, and Middle East and North Africa (MENA) countries, based on a preformulated research question, without any restrictions on date, language, or type of document.10 Studies performed on human subjects, reporting liver and IBD cancer in the MENA region, or providing an analysis of the contributing risk factors, including communicable and non-communicable diseases, behavioral aspects, environmental factors, genetic predispositions, and demographics, were included in the study. In addition, published studies reporting the epidemiological features or burden of liver cancer at a global, regional, or national scale, including the reports from the Global Burden of Disease (GBD) study, were reviewed. Two authors independently assessed the retrieved articles for relevance and quality, with points of disagreement resolved through discussion. The latest available data on the epidemiology and burden of liver cancer were also retrieved from the International Agency for Research on Cancer (IARC) as part of the GLOBOCAN project (GLOBOCAN 2022, version 1.1, 2024).11 A qualitative synthesis was performed, and the results were presented using thematic narrative synthesis.
Results
A total of 4395 articles were retrieved from the databases, 871 of which were removed due to the duplicity. The remaining articles were screened by title, abstract, and full text for relevance. A total of 64 studies were ultimately included in the qualitative synthesis.
Regional Overview
Liver cancer is a growing public health concern in the MENA region, as it contributes significantly to cancer-related morbidity and mortality.8 This region is characterized by a unique epidemiological profile, heavily influenced by chronic infections such as HBV and HCV, alongside emerging risk factors such as diabetes and MAFLD. The MENA region encompasses diverse socioeconomic and healthcare settings, leading to variations in disease burden across different countries.12 However, a common feature in many MENA countries is the notable prevalence of viral hepatitis, which performs a fundamental role in the burden of liver cancer in the region.13
High rates of HBV/HCV infections have affected liver cancer incidence in this region throughout the past years given that both viruses are recognized as risk factors for the development of HCC.14 The prevalence of chronic HBV infection is less than 1% in some areas, yet several MENA countries, including Sudan, show rates as high as 8%.15 Liver cancer is a serious concern in this country, which has one of the greatest numbers of HCV cases around the world, with HCC being the most prevalent form.16 While concerted efforts in recent years have reduced the prevalence of HCV in Egypt due to widespread treatment with direct-acting antivirals (DAAs), the long-term effects of chronic infections continue to contribute to elevated rates of liver cancer.17 Several other MENA countries, including Saudi Arabia and Iraq, also report high incidence rates of liver cancer due to the combination of chronic viral hepatitis and the growing trends of metabolic conditions.18
Globally, the age-standardized incidence rate (ASIR) and age-standardized mortality rate (ASMR) of liver cancer are estimated to be around 9.3 and 8.5 cases per 100 000 person years, respectively, with major variations across regions and significantly lower incidence among females.4,19 MENA countries have varying liver cancer incidence rates, with countries like Egypt reporting ASIR as high as around 20 cases, which, although higher than the global average, is comparable to other high-burden regions.13 Moreover, studies have reported an increase of 11.9% in liver cancer regional ASIR from 1990 to 2017.13
The rates of new cases of liver cancer across the MENA region are relatively diverse, reflecting differences in public health infrastructure, risk factor distribution, and healthcare access. Figure 1 presents the MENA countries with the highest ASIR and ASMR of liver and IBD cancer in 2022. Apart from the metabolic shift, lack of efficient healthcare infrastructure, economic instability, ongoing conflicts, and lack of access to early diagnostic and treatment services remain key challenges in addressing the liver cancer burden in many MENA countries. Future projections indicate that liver cancer incidence will continue to rise, particularly in countries with high rates of metabolic disorders. Figures 2 and 3 present the overall and country-wise projections for liver and IBD cancer until 2050.
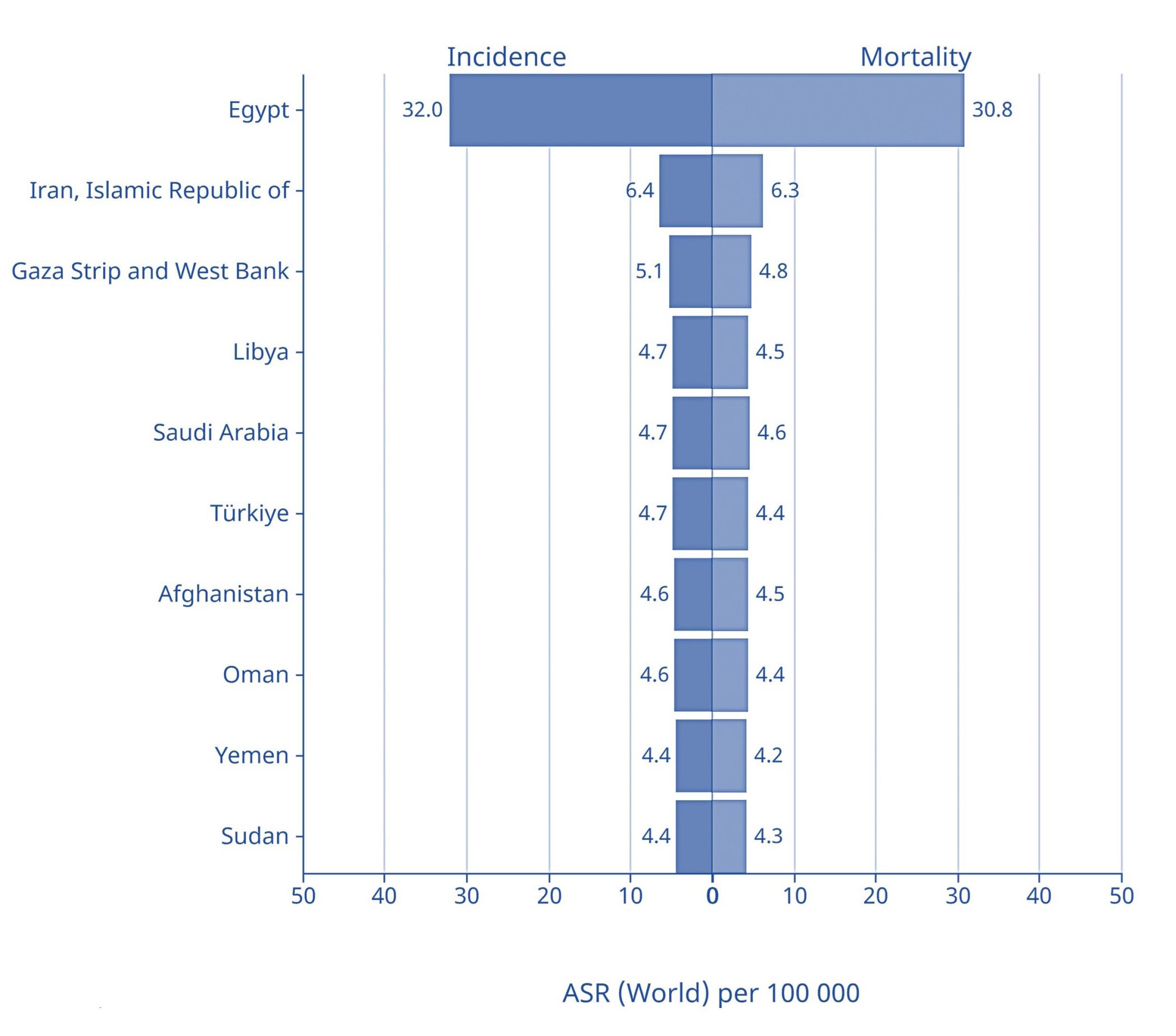
Figure 1.
Countries with the Highest Age-standardized Incidence and Mortality Rates of Liver and Intrahepatic Bile Duct Cancer in 2022 in the Middle East and North Africa
.
Countries with the Highest Age-standardized Incidence and Mortality Rates of Liver and Intrahepatic Bile Duct Cancer in 2022 in the Middle East and North Africa
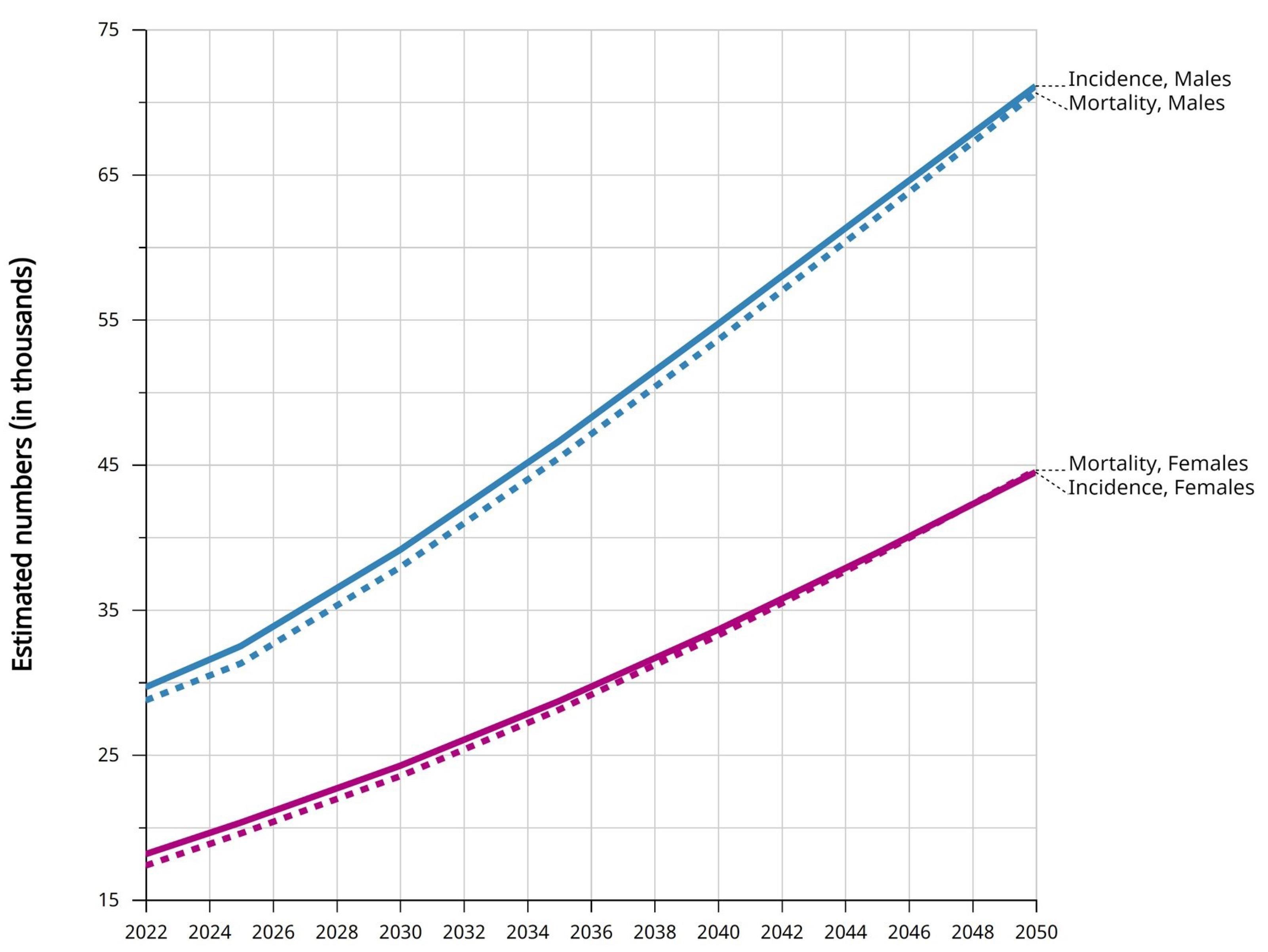
Figure 2.
Trends and Projections for Liver and Intrahepatic Bile Duct Cancer Incidence and Mortality from 2022 to 2050 in the Middle East and North Africa
.
Trends and Projections for Liver and Intrahepatic Bile Duct Cancer Incidence and Mortality from 2022 to 2050 in the Middle East and North Africa
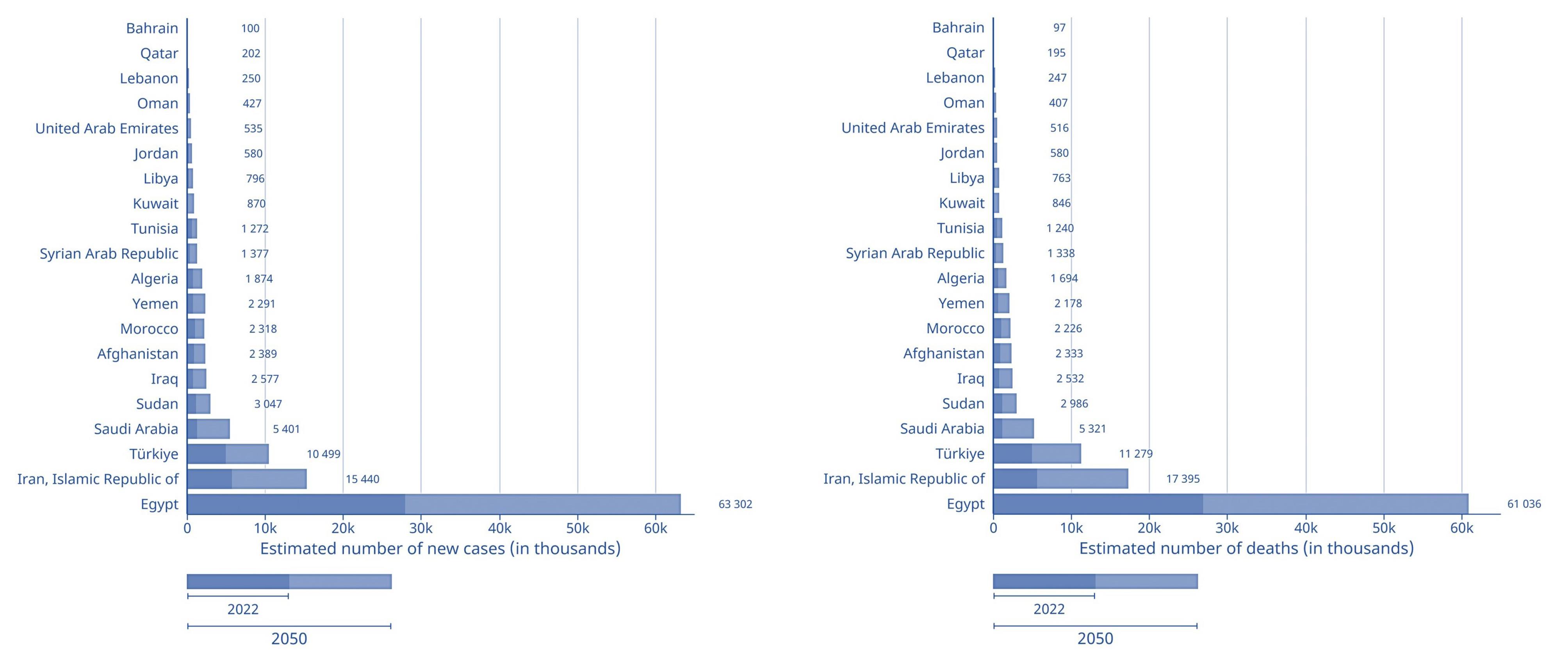
Figure 3.
The Country-wise Estimation of Liver and Intrahepatic Bile Duct Cancer Incidence and Mortality from 2022 to 2050 in the Middle East and North Africa
.
The Country-wise Estimation of Liver and Intrahepatic Bile Duct Cancer Incidence and Mortality from 2022 to 2050 in the Middle East and North Africa
Hotspot Countries
Egypt
Liver cancer is regarded as a concerning public health challenge in Egypt as it has one of the highest incidence rates worldwide. The longstanding high prevalence of HCV infection largely affects country’s liver cancer burden, though other factors, such as HBV, MAFLD, and metabolic disorders, are also becoming significant contributors.20 Over the past few decades, Egypt has experienced substantial shifts in liver cancer epidemiology due to public health interventions, demographic changes, and lifestyle modifications.
Egypt is constantly among the nations with the highest liver cancer rates worldwide. Some studies have even reported ASIR and ASMR as high as 32.2 and 31.8 cases per 100 000 people per year in this country, significantly higher than the worldwide average of 9.3 per 100 000.21,22 Liver is the most prevalent cancer site among Egyptian men and ranks second among women, accounting for nearly 33% of the country’s cancer-related mortalities.23
The distinct epidemiological context of the country, where the frequency of chronic HCV infection has historically been among the highest ones in history, is the primary cause of the heightened incidence of liver cancer in Egypt.16,24 For much of the 20th century, Egypt faced an HCV epidemic, which was potentially exacerbated by unsafe medical practices during 1960-1970s mass schistosomiasis treatment campaigns.25 These campaigns, which involved the use of inadequately sterilized needles, might have facilitated widespread transmission of HCV, ultimately leading to millions of chronic infections.
Liver cancer is not evenly distributed across the Egyptian population; in other words, men are significantly more prone to develop liver cancer, with a roughly 4:1 male-to-female ratio.22 This disparity is partly due to the prevalence of chronic viral hepatitis and cirrhosis in men, as well as greater exposure to environmental and occupational risk factors. Geographically, liver cancer is more prevalent in rural areas, although urbanization is associated with rising cases of MAFLD and metabolic liver disease. Historically, rural populations, particularly in the Nile Delta region, had higher rates of HCV infection due to the schistosomiasis treatment campaigns that were concentrated in these areas.26,27
Recent studies have revealed HCV infection as a prominent cause of HCC and liver cirrhosis among Egyptians, followed by cirrhosis of unknown etiology, HBV infection, and HBV-HCV co-infection.28,29 Over the last two decades, Egypt has made significant efforts to reduce the prevalence of HCV, which has begun to affect liver cancer trends in the country. In 2014, Egypt launched a nationwide initiative to eradicate HCV using DAAs, which have proven highly effective.30 By 2020, over 4 million Egyptians had been treated, and HCV prevalence was reduced from 14.7% to approximately 4.5%.25,31 This large-scale effort was supported by mass screening programs aimed at detecting HCV in the general population, where around 50 million Egyptians (around 79.5% of the target population) were screened in the initial months.32 Despite this progress, the HCV epidemic continues to impact liver cancer rates, and due to the long latency period between chronic HCV infection and HCC development, many individuals who contracted the virus before widespread antiviral treatment became available are now presenting with liver cancer. This has created a lag effect in which the incidence of liver cancer remains high, even as HCV prevalence declines.33 Generally, a plateau in liver cancer rates, with a subsequent decline, may be the scenario in the upcoming decades as the long-term effects of HCV control programs take hold.
Iran
The incidence of liver cancer is not significantly higher in Iran in comparison to global averages, with an ASIR of 6.4 cases per 100000 people, respectively.11,34,35 Although the ASIR among males does not significantly differ from the global rates, the ASIR among females is significantly higher compared to other countries. More recent studies have highlighted a five-fold increase in the ASIR of liver cancer in the last three decades.36 Liver cancer mortality rate also tends to increase, regardless of gender and province. Liver cancer alone accounts for more than 2% of all cancers diagnosed in Iran but falls among the top five cancer-related causes of death.37,38 However, although reports have indicated Iran as a region with a low risk of liver cancer, 40% of the cases are possibly underreported due to limited access to cancer registry systems and late-stage diagnosis, as liver cancer is often asymptomatic in its early stages.39
About three out of every four liver cancer mortalities are due to HBV/HCV infections.39 HBV has been the most significant underlying cause of liver cancer in Iran, but the landscape is gradually shifting. Following the nationwide HBV vaccination program initiated in 1993, Iran has significantly reduced HBV prevalence, particularly among younger generations.40 As a result, liver cancer cases related to HBV are expected to decline in the future. HCV, while less prevalent than HBV, is also a contributor to liver cancer in Iran, particularly among high-risk individuals, including intravenous drug users.41 National efforts to improve diagnosis and treatment of HCV have been less comprehensive compared to HBV, but recent initiatives aim to address this gap. As more HCV-infected individuals are identified and treated with DAAs, the HCV-related liver cancer burden may also decrease.40
Metabolic disorders are a prominent cause of liver cancer in Iran. The rising prevalence of diabetes and obesity in Iran, both with a prevalence of over 20%, have significantly contributed to this cause.42 Recent studies have reported an overall prevalence of 33% for non-alcoholic fatty liver disease (NAFLD) in Iran, rising to around 37% among adults.43 A rising incidence of MAFLD is influencing the overall trend of liver cancer in Iran. The alarming increase in obesity, type 2 diabetes, and sedentary lifestyles in Iran has resulted in an increased NAFLD-related liver cancer, turning it into a risk factor for primary liver cancer in Iran.44 The aging population is expected to further contribute to an increasing liver cancer burden in Iran in the coming years, as older adults are more prone to develop chronic liver diseases and cirrhosis.45,46 Additionally, as metabolic risk factors continue to rise, younger populations may face higher risks of liver disease, shifting the epidemiological profile of this cancer over time.
Saudi Arabia
The annual number of new liver cancer cases in Saudi Arabia is lower compared to some other parts of the Middle East, but it has been rising steadily.47 According to the updated data from Saudi cancer registries, ASIR and ASMR of liver cancer in Saudi Arabia are approximately 4.5 and 4.2 per 100 000 person-years, with an overall male-to-female ratio of 2.5.47,48 Liver cancer represents about 3% to 5% of all cancers diagnosed in Saudi Arabia.48,49
The incidence of liver cancer has risen in Saudi Arabia in line with several important public health trends. HBV was the primary driver of liver cancer, and the country’s early experience with viral hepatitis infections was due to the high endemicity of HBV before the introduction of comprehensive vaccination programs.50 Since 1989, Saudi Arabia has implemented nationwide neonatal HBV vaccination programs, which has, in turn, translated into a decreasing trend in HBV-related liver cancer cases over time.51 Although the number of liver cancer cases in Saudi Arabia is not considered among the global hotspots, most detected cases are late-stage and with poor prognosis.52
Turkey
Turkey has a relatively moderate incidence of liver cancer compared to global hotspots, with a liver cancer ASIR of approximately 4.5 to 7.6 per 100 000 people annually.53,54 This places Turkey in the middle range globally but higher than many Western European nations. Representing less than 3% of all cancers diagnosed in Turkey, most patients are diagnosed at advanced stages, accounting for around 4.3% of cancer-related mortality in Turkey, with a 5-year age-standardized survival rate of 15.9%.54 Recent studies have reported an overall median survival of 16 months, which does not significantly differ from the other regions.55
Risk Factors and Underlying Conditions
Various underlying conditions, such as chronic viral infections, and several risk factors, including metabolic disorders, environmental exposures, and lifestyle factors, affect the regional liver cancer burden. In general, metabolic risks (including high body mass index and high fasting plasma glucose) and behavioral risks (including smoking, tobacco, high alcohol consumption, and drug use) are the most important factors contributing to liver cancer mortality in MENA region, respectively, with an ever-increasing trend in the region (Figure 4). Meanwhile, environmental and occupational risks show a decreasing trend throughout the last three decades. Overall, the key risk factors for liver cancer and underlying conditions are presented in Figure 5.
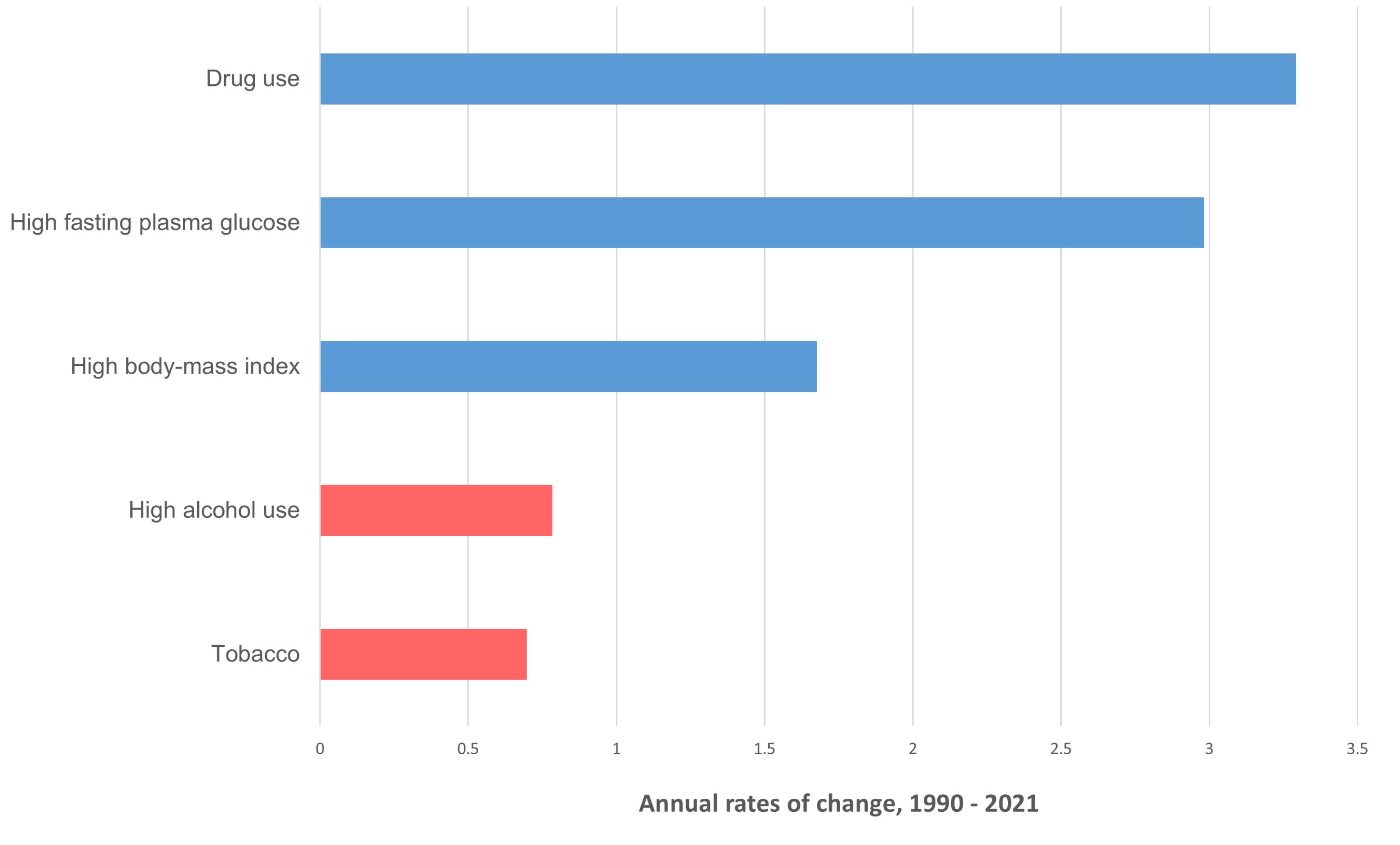
Figure 4.
Annualized Rates of Change for the Top 5 Contributing Risk Factors for Liver Cancer in the Middle East and North Africa Region from 1990 to 2021
.
Annualized Rates of Change for the Top 5 Contributing Risk Factors for Liver Cancer in the Middle East and North Africa Region from 1990 to 2021
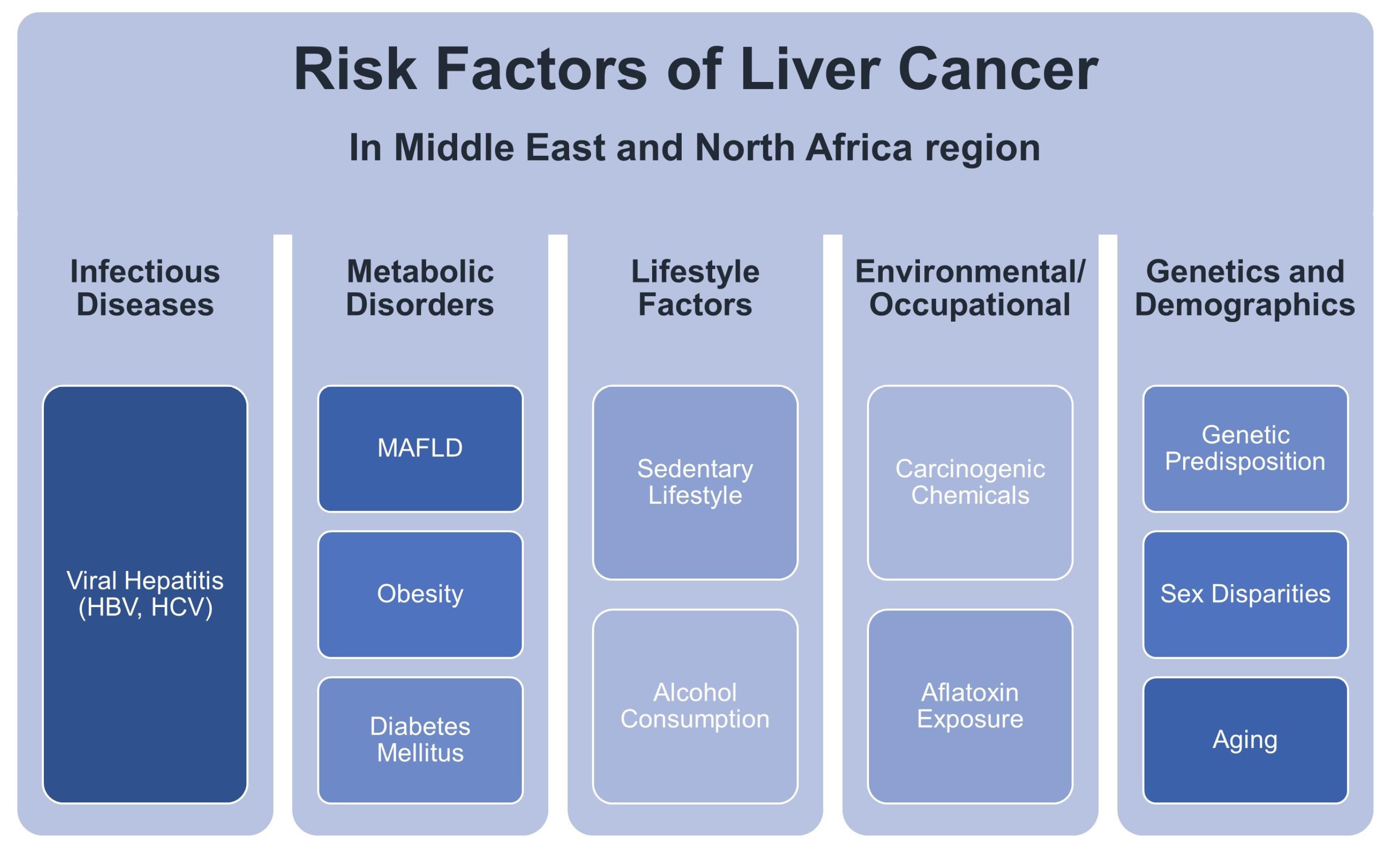
Figure 5.
Summary Diagram Representing the Key Risk Factors for Liver and Intrahepatic Bile Duct Cancer in the Middle East and North Africa. Abbreviations: HBV, hepatitis B virus. HCV, hepatitis C virus; MAFLD, metabolic dysfunction-associated fatty liver disease
.
Summary Diagram Representing the Key Risk Factors for Liver and Intrahepatic Bile Duct Cancer in the Middle East and North Africa. Abbreviations: HBV, hepatitis B virus. HCV, hepatitis C virus; MAFLD, metabolic dysfunction-associated fatty liver disease
Viral Hepatitis
Globally, chronic HBV infection is the principal cause of liver cancer, and it continues to be a significant risk factor among MENA nations.56 HBV is endemic in several areas of the region, especially North Africa. Long-term HBV infection leads to chronic liver disease, cirrhosis, and elevated risk of HCC, particularly among those infected at birth or in early childhood.57 WHO recommends universal HBV vaccination, and most MENA countries have implemented vaccination programs.58 For instance, Egypt, Iran, and Saudi Arabia have significantly reduced the prevalence of HBV among younger populations through vaccination. However, many individuals born before these programs remain chronically infected.
Recent estimates suggest that around 2% to 7% of the residents of the MENA are chronically infected with HBV, varying between and within countries.59 Around 15% to 40% of individuals with chronic HBV develop liver failure or HCC.60 Furthermore, co-infection with hepatitis D virus (HDV), which is common in certain countries like Iran and Egypt, raises the incidence of HCC and aggravates liver damage.61
Another important risk factor for liver cancer is HCV infection, which is especially prevalent in nations with a history of high prevalence of HCV such as Egypt, Iraq, and Morocco. Primarily transmitted through unsafe medical procedures, such as blood transfusions and the use of non-sterile medical equipment, HCV easily progresses to cirrhosis. Recent advancements in antiviral therapies, such as DAAs, have dramatically improved the prognosis for individuals with chronic HCV infection, significantly reducing the risk of liver cancer through infection clearance.62 However, many people in the MENA region still lack access to these therapies due to cost, healthcare infrastructure limitations, and diagnostic challenges.
Non-communicable Diseases
Cirrhosis, MAFLD, and diabetes mellitus are emerging health concerns and significant risk factors for liver cancer. Previously known as NAFLD, MAFLD is observed in individuals with metabolic dysfunction, irrespective of alcohol consumption.63 Urbanization, sedentary lifestyles, and dietary changes have contributed to an increase in obesity and metabolic disorders across the region, particularly in wealthier Gulf states.64 Estimates suggest that NAFLD is present in around 32% of the adult population in the MENA region, with an exceptionally high burden among middle-aged and elderly individuals.65 Public health strategies focused on addressing the root causes of metabolic syndrome, including obesity prevention and the promotion of healthier diets and physical activity, are critical for controlling the upcoming regional burden of metabolic-related liver cancer.66
Alcohol Consumption
While alcohol consumption is generally low in the MENA region due to religious and cultural factors, alcohol-related liver disease is still a concern in certain populations.67 In some MENA countries, alcohol-related liver disease is an emerging risk factor; still, its contribution to the overall liver cancer burden is relatively modest compared to viral hepatitis and metabolic liver disease.
Aflatoxin Exposure
In certain MENA nations, aflatoxins, carcinogenic substances produced by specific fungi that contaminate the food supply, especially grains, have been connected to a heightened risk of liver cancer.68 Aflatoxin exposure, especially in chronic HBV-infected population, significantly increases the risk of HCC. Countries with poor food storage practices and higher consumption of contaminated crops face a higher risk of aflatoxin-induced liver cancer.69 While aflatoxin contamination is a well-documented risk factor in Sub-Saharan Africa and Southeast Asia, it has also been identified as a concern in some parts.70 Improved agricultural practices, food safety regulations, and public awareness are critical for reducing aflatoxin exposure and the associated risk of liver cancer.
Environmental and Occupational Exposures
Environmental factors, including exposure to industrial chemicals and pollutants, may also be risk factors for liver cancer in the region, particularly in countries with rapid industrialization and inadequate environmental protections. For example, exposure to vinyl chloride and arsenic, known as carcinogens, has been linked to liver cancer.21 Water scarcity in the region has also increased reliance on treated water, increasing exposure to carcinogenic disinfection byproducts, such as trihalomethanes and haloacetic acids.71 Occupational exposures in industries such as agriculture, construction, and petrochemicals may also contribute to the liver cancer burden, although data on these exposures in the MENA region remain limited.
Genetic and Demographic Factors
As with global trends, men are more likely to develop liver cancer, a disparity that is partly explained by higher HBV/HCV infection rates, alcohol consumption, and exposure to other contributing factors in men. In addition, liver cancer is primarily a disease of older adults, with more than 80% of the cases diagnosed after the age of 70.72 As life expectancy increases in many MENA countries, the aging population is expected to contribute to the increasing incidence of liver cancer. Genetic predisposition to liver cancer has also been suggested in certain populations, though more studies are mandatory to clarify the role of genetics.
Discussion
Liver cancer is a critical health issue in the region, with declining rates of viral hepatitis-related cases in some countries but a rising epidemic of MAFLD. While public health interventions targeting HBV and HCV have had a positive impact, particularly in countries like Egypt, the growing burden of obesity, diabetes, and metabolic syndrome presents a new challenge for the region. Future projections indicate that liver cancer incidence will continue to rise, particularly in countries with high rates of metabolic disorders. Public health interventions, especially vaccination against HBV and broad access to DAA therapies for HCV, have played a crucial role in altering liver cancer trends in the region. HBV vaccination programs, implemented in most MENA countries in the 1990s, have dramatically reduced the prevalence of HBV among younger populations, which is expected to lower HBV-related liver cancer rates in the coming decades. Egypt’s large-scale HCV treatment campaign, initiated in 2014, seems highly effective in reducing the country’s once significantly high HCV prevalence. As large proportions of the population are successfully treated, the burden of HCV-related liver cancer is expected to decline. Meanwhile, given the long latency period between infection and cancer development, the full impact of these interventions on liver cancer rates may not be seen for several upcoming years.
The limited availability of antiviral treatments, challenges in healthcare infrastructure, and inconsistent access to screening programs have hindered progress in controlling HBV and HCV, leading to ongoing high rates of viral hepatitis-related liver cancer. Countries with lower healthcare investments, such as Yemen and Sudan, probably will continue facing barriers in reducing liver cancer incidence due to under-resourced public health systems. The population aging across the MENA region is another key factor influencing future liver cancer trends. As life expectancy increases, particularly in wealthier nations, the incidence of age-related diseases, including liver cancer, is expected to rise. Older adults are more likely to develop liver cancer, and as the population structure shifts, this demographic change could contribute to a significant increase in cancer cases. Healthcare systems across the MENA region must adapt to these changing epidemiological trends. Moreover, considering the evolving landscape of liver cancer treatment and the incorporation of novel immunotherapy and targeted therapy modalities in clinical practice guidelines, providing stable access to innovative anticancer therapies is more important than ever.73-75
Prevention strategies for liver cancer in the MENA region should focus on both controlling viral hepatitis and addressing the rising burden of MAFLD. Lifestyle and dietary modifications are key interventions for reducing liver cancer risk. Additionally, establishing comprehensive regional cancer registries and improving data collection is essential to accurately track trends, identify at-risk populations, and lead public health strategies. Advocacy for public health initiatives and policy changes, including vaccination programs, diabetes management, and environmental health regulations, is essential to control the growing liver cancer burden in the region. Moreover, the significant heterogeneity in the epidemiology of liver cancer in the regions necessitates more population-based studies at national and subnational levels.
Conclusions
Liver cancer poses a significant and growing public health challenge in the MENA region, driven by a multipart interplay of underlying factors such as chronic viral hepatitis, metabolic disorders, environmental exposures, and demographic shifts. While public health interventions, such as HBV vaccination programs and HCV treatment campaigns, have successfully lowered viral hepatitis-related liver cancer in some countries, the mounting burden of metabolic disorders is contributing to a surge in MAFLD-related liver cancer. Prevention efforts must now evolve to address both viral and metabolic risk factors, with an emphasis on lifestyle and dietary interventions, improved healthcare access, and targeted public health strategies. Early detection and surveillance programs are critical given the increasing contribution of non-viral causes of liver cancer. Looking ahead, addressing the growing concern of liver cancer in the MENA region will require a coordinated approach, integrating public health initiatives, policy reforms, and community-based interventions. Without urgent action, the region faces a growing cancer burden that will strain healthcare systems and result in significant loss of life.
Acknowledgements
We would like to express our gratitude to the Social Determinants of Health Research Center at Tabriz University of Medical Sciences in Tabriz, Iran.
Author contributions
Conceptualization: Saeid Safiri.
Funding acquisition: Saeid Safiri.
Investigation: Mohammad-Salar Hosseini.
Methodology: Saeid Safiri.
Project administration: Saeid Safiri.
Software: Mohammad-Salar Hosseini.
Supervision: Saeid Safiri.
Validation: Saeid Safiri.
Visualization: Mohammad-Salar Hosseini.
Writing–original draft: Mohammad-Salar Hosseini, Manouchehr Khoshbaten, Ali-Asghar Kolahi, Saeid Safiri.
Writing–review & editing: Mohammad-Salar Hosseini, Ali-Asghar Kolahi, Saeid Safiri.
Data availability statement
All data generated or analyzed during this study are included in this published article.
Ethical approval
This part of the project was approved by the Ethics Committee of Tabriz University of Medical Sciences, Tabriz, Iran, and is included in a Master of Public Health thesis (IR.TBZMED.REC.1402.267).
Consent for publication
Not applicable.
Conflict of interests
The authors declare no conflict of interests.
References
- Chidambaranathan-Reghupaty S, Fisher PB, Sarkar D. Hepatocellular carcinoma (HCC): epidemiology, etiology and molecular classification. Adv Cancer Res 2021; 149:1-61. doi: 10.1016/bs.acr.2020.10.001 [Crossref] [ Google Scholar]
- Chon YE, Park SY, Hong HP, Son D, Lee J, Yoon E. Hepatocellular carcinoma incidence is decreasing in Korea but increasing in the very elderly. Clin Mol Hepatol 2023; 29(1):120-34. doi: 10.3350/cmh.2021.0395 [Crossref] [ Google Scholar]
- Massarweh NN, El-Serag HB. Epidemiology of hepatocellular carcinoma and intrahepatic cholangiocarcinoma. Cancer Control 2017; 24(3):1073274817729245. doi: 10.1177/1073274817729245 [Crossref] [ Google Scholar]
- Li Q, Cao M, Lei L, Yang F, Li H, Yan X. Burden of liver cancer: From epidemiology to prevention. Chin J Cancer Res 2022; 34(6):554-66. doi: 10.21147/j.issn.1000-9604.2022.06.02 [Crossref] [ Google Scholar]
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021; 71(3):209-49. doi: 10.3322/caac.21660 [Crossref] [ Google Scholar]
- Singal AG, Lampertico P, Nahon P. Epidemiology and surveillance for hepatocellular carcinoma: new trends. J Hepatol 2020; 72(2):250-61. doi: 10.1016/j.jhep.2019.08.025 [Crossref] [ Google Scholar]
- Toh MR, Wong EYT, Wong SH, Ng AWT, Loo LH, Chow PK. Global epidemiology and genetics of hepatocellular carcinoma. Gastroenterology 2023; 164(5):766-82. doi: 10.1053/j.gastro.2023.01.033 [Crossref] [ Google Scholar]
- Poustchi H, Sepanlou S, Esmaili S, Mehrabi N, Ansarymoghadam A. Hepatocellular carcinoma in the world and the middle East. Middle East J Dig Dis 2010; 2(1):31-41. [ Google Scholar]
- Safiri S, Nejadghaderi SA, Karamzad N, Kaufman JS, Carson-Chahhoud K, Bragazzi NL. Global, regional and national burden of cancers attributable to high fasting plasma glucose in 204 countries and territories, 1990-2019. Front Endocrinol (Lausanne) 2022; 13:879890. doi: 10.3389/fendo.2022.879890 [Crossref] [ Google Scholar]
- Hosseini MS, Jahanshahlou F, Akbarzadeh MA, Zarei M, Vaez-Gharamaleki Y. Formulating research questions for evidence-based studies. J Med Surg Public Health 2024; 2:100046. doi: 10.1016/j.glmedi.2023.100046 [Crossref] [ Google Scholar]
- International Agency for Research on Cancer (IARC). Global Cancer Observatory. Vol 2024. IARC; 2024.
- Nejadghaderi SA, Grieger JA, Karamzad N, Kolahi AA, Sullman MJ, Safiri S. Burden of diseases attributable to excess body weight in the Middle East and North Africa region, 1990-2019. Sci Rep 2023; 13(1):20338. doi: 10.1038/s41598-023-46702-y [Crossref] [ Google Scholar]
- Sharafi H, Alavian SM. The rising threat of hepatocellular carcinoma in the Middle East and North Africa region: results from Global Burden of Disease Study 2017. Clin Liver Dis (Hoboken) 2019; 14(6):219-23. doi: 10.1002/cld.890 [Crossref] [ Google Scholar]
- Shen C, Jiang X, Li M, Luo Y. Hepatitis virus and hepatocellular carcinoma: recent advances. Cancers (Basel) 2023; 15(2):533. doi: 10.3390/cancers15020533 [Crossref] [ Google Scholar]
- Habibzadeh F. Viral hepatitis in the Middle East. Lancet 2014; 384:1-2. [ Google Scholar]
- Ezzat R, Eltabbakh M, El Kassas M. Unique situation of hepatocellular carcinoma in Egypt: a review of epidemiology and control measures. World J Gastrointest Oncol 2021; 13(12):1919-38. doi: 10.4251/wjgo.v13.i12.1919 [Crossref] [ Google Scholar]
- Estes C, Abdel-Kareem M, Abdel-Razek W, Abdel-Sameea E, Abuzeid M, Gomaa A. Economic burden of hepatitis C in Egypt: the future impact of highly effective therapies. Aliment Pharmacol Ther 2015; 42(6):696-706. doi: 10.1111/apt.13316 [Crossref] [ Google Scholar]
- Alavian SM, Haghbin H. Relative importance of hepatitis B and C viruses in hepatocellular carcinoma in EMRO countries and the Middle East: a systematic review. Hepat Mon 2016; 16(3):e35106. doi: 10.5812/hepatmon.35106 [Crossref] [ Google Scholar]
- Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2024; 74(3):229-63. doi: 10.3322/caac.21834 [Crossref] [ Google Scholar]
- Lehman EM, Wilson ML. Epidemiology of hepatitis viruses among hepatocellular carcinoma cases and healthy people in Egypt: a systematic review and meta-analysis. Int J Cancer 2009; 124(3):690-7. doi: 10.1002/ijc.23937 [Crossref] [ Google Scholar]
- Lampimukhi M, Qassim T, Venu R, Pakhala N, Mylavarapu S, Perera T. A review of incidence and related risk factors in the development of hepatocellular carcinoma. Cureus 2023; 15(11):e49429. doi: 10.7759/cureus.49429 [Crossref] [ Google Scholar]
- Goodarzi E, Ghorat F, Mosavi Jarrahi A, Adineh HA, Sohrabivafa M, Khazaei Z. Global incidence and mortality of liver cancers and its relationship with the human development index (HDI): an ecology study in 2018. World Cancer Research Journal 2019; 6:e1255. doi: 10.32113/wcrj_20194_1255 [Crossref] [ Google Scholar]
- Ngoma TA, Ngoma M. Global burden of cancer. In: Kickbusch I, Ganten D, Moeti M, eds. Handbook of Global Health. Cham: Springer; 2021. p. 459-94. 10.1007/978-3-030-45009-0_26.
- Mohamoud YA, Mumtaz GR, Riome S, Miller D, Abu-Raddad LJ. The epidemiology of hepatitis C virus in Egypt: a systematic review and data synthesis. BMC Infect Dis 2013; 13:288. doi: 10.1186/1471-2334-13-288 [Crossref] [ Google Scholar]
- Hassanin A, Kamel S, Waked I, Fort M. Egypt’s ambitious strategy to eliminate hepatitis C virus: a case study. Glob Health Sci Pract 2021; 9(1):187-200. doi: 10.9745/ghsp-d-20-00234 [Crossref] [ Google Scholar]
- Habib M, Mohamed MK, Abdel-Aziz F, Magder LS, Abdel-Hamid M, Gamil F. Hepatitis C virus infection in a community in the Nile Delta: risk factors for seropositivity. Hepatology 2001; 33(1):248-53. doi: 10.1053/jhep.2001.20797 [Crossref] [ Google Scholar]
- Darwish MA, Faris R, Darwish N, Shouman A, Gadallah M, El-Sharkawy MS. Hepatitis c and cirrhotic liver disease in the Nile Delta of Egypt: a community-based study. Am J Trop Med Hyg 2001; 64(3-4):147-53. doi: 10.4269/ajtmh.2001.64.147 [Crossref] [ Google Scholar]
- Yang JD, Mohamed EA, Aziz AO, Shousha HI, Hashem MB, Nabeel MM. Characteristics, management, and outcomes of patients with hepatocellular carcinoma in Africa: a multicountry observational study from the Africa Liver Cancer Consortium. Lancet Gastroenterol Hepatol 2017; 2(2):103-11. doi: 10.1016/s2468-1253(16)30161-3 [Crossref] [ Google Scholar]
- Huang DQ, Terrault NA, Tacke F, Gluud LL, Arrese M, Bugianesi E. Global epidemiology of cirrhosis - aetiology, trends and predictions. Nat Rev Gastroenterol Hepatol 2023; 20(6):388-98. doi: 10.1038/s41575-023-00759-2 [Crossref] [ Google Scholar]
- Omran D, Alboraie M, Zayed RA, Wifi MN, Naguib M, Eltabbakh M. Towards hepatitis C virus elimination: Egyptian experience, achievements and limitations. World J Gastroenterol 2018; 24(38):4330-40. doi: 10.3748/wjg.v24.i38.4330 [Crossref] [ Google Scholar]
- Abdelrahman H, Abdelmoktader A, Hammad AA, Bassyouni R. Changing in the prevalence of hepatitis C virus infection in Fayoum governorate, Egypt. Fayoum Univ Med J 2020; 7(1):25-35. doi: 10.21608/fumj.2020.174342 [Crossref] [ Google Scholar]
- Waked I, Esmat G, Elsharkawy A, El-Serafy M, Abdel-Razek W, Ghalab R. Screening and treatment program to eliminate hepatitis C in Egypt. N Engl J Med 2020; 382(12):1166-74. doi: 10.1056/NEJMsr1912628 [Crossref] [ Google Scholar]
- Lazarus JV, Picchio CA, Colombo M. Hepatocellular carcinoma prevention in the era of hepatitis C elimination. Int J Mol Sci 2023; 24(18):14404. doi: 10.3390/ijms241814404 [Crossref] [ Google Scholar]
- Mirzaei M, Ghoncheh M, Pournamdar Z, Soheilipour F, Salehiniya H. Incidence and trend of liver cancer in Iran. J Coll Physicians Surg Pak 2016; 26(4):306-9. [ Google Scholar]
- Farahmand M, Almasi-Hashiani A, Fallahzadeh M. Epidemiology of cancer of liver and intrahepatic bile ducts based on Fars province cancer registry’s data, (2001-8). Zahedan J Res Med Sci 2013; 15(2):e93119. [ Google Scholar]
- Ebrahimi P, Karami M, Delavari S, Shojaie L, Hosseini-Berneti SH, Bayani F. Investigating the mortality trend of gastrointestinal cancers in Babol, North Iran (2013-2021). BMC Gastroenterol 2024; 24(1):100. doi: 10.1186/s12876-024-03189-9 [Crossref] [ Google Scholar]
- Khanali J, Kolahi AA. National and subnational cancer incidence for 22 cancer groups, 2000 to 2016: a study based on cancer registration data of Iran. J Cancer Epidemiol 2021; 2021:6676666. doi: 10.1155/2021/6676666 [Crossref] [ Google Scholar]
- Rumgay H, Arnold M, Ferlay J, Lesi O, Cabasag CJ, Vignat J. Global burden of primary liver cancer in 2020 and predictions to 2040. J Hepatol 2022; 77(6):1598-606. doi: 10.1016/j.jhep.2022.08.021 [Crossref] [ Google Scholar]
- Rezaei N, Farzad Far F, Khademiureh S, Sheidaei A, Gohari K, Delavari F. Liver cancer mortality at national and provincial levels in Iran between 1990 and 2015: a meta regression analysis. Hepat Mon 2018; 18(1):e62009. doi: 10.5812/hepatmon.62009 [Crossref] [ Google Scholar]
- Behzadifar M, Azari S, Shirkhani S, Gholamrezaei S, Shahabi S, Doshmangir L. Hepatitis B vaccination in Iran: historical policies and programs. J Prev Med Hyg 2022; 63(4):E618-24. doi: 10.15167/2421-4248/jpmh2022.63.4.2731 [Crossref] [ Google Scholar]
- Malekinejad M, Navadeh S, Lotfizadeh A, Rahimi-Movaghar A, Amin-Esmaeili M, Noroozi A. High hepatitis C virus prevalence among drug users in Iran: systematic review and meta-analysis of epidemiological evidence (2001-2012). Int J Infect Dis 2015; 40:116-30. doi: 10.1016/j.ijid.2015.09.022 [Crossref] [ Google Scholar]
- Hassanipour S, Amini-Salehi E, Joukar F, Khosousi MJ, Pourtaghi F, Ansar MM. The prevalence of non-alcoholic fatty liver disease in Iranian children and adult population: a systematic review and meta-analysis. Iran J Public Health 2023; 52(8):1600-12. doi: 10.18502/ijph.v52i8.13399 [Crossref] [ Google Scholar]
- Tabaeian SP, Rezapour A, Azari S, Martini M, Saran M, Behzadifar M. Prevalence of non-alcoholic fatty liver disease in Iran: a systematic review and meta-analysis. J Clin Exp Hepatol 2024; 14(1):101209. doi: 10.1016/j.jceh.2023.06.009 [Crossref] [ Google Scholar]
- Golabi P, Paik JM, AlQahtani S, Younossi Y, Tuncer G, Younossi ZM. Burden of non-alcoholic fatty liver disease in Asia, the Middle East and North Africa: data from Global Burden of Disease 2009-2019. J Hepatol 2021; 75(4):795-809. doi: 10.1016/j.jhep.2021.05.022 [Crossref] [ Google Scholar]
- Georgieva M, Xenodochidis C, Krasteva N. Old age as a risk factor for liver diseases: modern therapeutic approaches. Exp Gerontol 2023; 184:112334. doi: 10.1016/j.exger.2023.112334 [Crossref] [ Google Scholar]
- Wu XN, Xue F, Zhang N, Zhang W, Hou JJ, Lv Y. Global burden of liver cirrhosis and other chronic liver diseases caused by specific etiologies from 1990 to 2019. BMC Public Health 2024; 24(1):363. doi: 10.1186/s12889-024-17948-6 [Crossref] [ Google Scholar]
- Alghamdi IG, Alghamdi MS. The incidence rate of liver cancer in Saudi Arabia: an observational descriptive epidemiological analysis of data from the Saudi Cancer Registry (2004-2014). Cancer Manag Res 2020; 12:1101-11. doi: 10.2147/cmar.s232600 [Crossref] [ Google Scholar]
- Alqahtani SA, Sanai FM, Alolayan A, Abaalkhail F, Alsuhaibani H, Hassanain M. Saudi Association for the Study of Liver diseases and Transplantation practice guidelines on the diagnosis and management of hepatocellular carcinoma. Saudi J Gastroenterol 2020; 26(Suppl 1):S1-40. doi: 10.4103/sjg.SJG_477_20 [Crossref] [ Google Scholar]
- Albarrak J, Al-Shamsi H. Current status of management of hepatocellular carcinoma in the Gulf region: challenges and recommendations. Cancers (Basel) 2023; 15(7):2001. doi: 10.3390/cancers15072001 [Crossref] [ Google Scholar]
- Sanai F, Alkhatry M, Alzanbagi A, Kumar S. Hepatitis B virus infection in Saudi Arabia and the UAE: public health challenges and their remedial measures. J Infect Public Health 2023; 16(9):1410-7. doi: 10.1016/j.jiph.2023.07.008 [Crossref] [ Google Scholar]
- Abdo AA, Sanai FM, Al-Faleh FZ. Epidemiology of viral hepatitis in Saudi Arabia: are we off the hook?. Saudi J Gastroenterol 2012; 18(6):349-57. doi: 10.4103/1319-3767.103425 [Crossref] [ Google Scholar]
- Althubiti M, Alfayez M. Insights on hepatocellular carcinoma in Saudi Arabia. In: Carr BI, ed. Liver Cancer in the Middle East. Cham: Springer; 2021. p. 247-57. 10.1007/978-3-030-78737-0_16.
- Mohammadian M, Allah Bakeshei K, Mohammadian-Hafshejani A. International epidemiology of liver cancer: geographical distribution, secular trends and predicting the future. J Prev Med Hyg 2020; 61(2):E259-89. doi: 10.15167/2421-4248/jpmh2020.61.2.1244 [Crossref] [ Google Scholar]
- Eser S, Örün H, Hamavioğlu E, Lofti F. Cancer incidence, mortality and survival in Türkiye as of 2020. Basic Clin Cancer Res 2023; 14(1):1-13. doi: 10.18502/bccr.v14i1.14383 [Crossref] [ Google Scholar]
- Ekinci O, Baran B, Ormeci AC, Soyer OM, Gokturk S, Evirgen S. Current state and clinical outcome in Turkish patients with hepatocellular carcinoma. World J Hepatol 2018; 10(1):51-61. doi: 10.4254/wjh.v10.i1.51 [Crossref] [ Google Scholar]
- Abdelhamed W, El-Kassas M. Hepatitis B virus as a risk factor for hepatocellular carcinoma: there is still much work to do. Liver Res 2024; 8(2):83-90. doi: 10.1016/j.livres.2024.05.004 [Crossref] [ Google Scholar]
- Rizzo GEM, Cabibbo G, Craxì A. Hepatitis B virus-associated hepatocellular carcinoma. Viruses 2022; 14(5):986. doi: 10.3390/v14050986 [Crossref] [ Google Scholar]
- Al-Busafi SA, Alwassief A. Global perspectives on the hepatitis B vaccination: challenges, achievements, and the road to elimination by 2030. Vaccines (Basel) 2024; 12(3):288. doi: 10.3390/vaccines12030288 [Crossref] [ Google Scholar]
- MacLachlan JH, Cowie BC. Hepatitis B virus epidemiology. Cold Spring Harb Perspect Med 2015; 5(5):a021410. doi: 10.1101/cshperspect.a021410 [Crossref] [ Google Scholar]
- Varghese N, Majeed A, Nyalakonda S, Boortalary T, Halegoua-DeMarzio D, Hann HW. Review of related factors for persistent risk of hepatitis B virus-associated hepatocellular carcinoma. Cancers (Basel) 2024; 16(4):777. doi: 10.3390/cancers16040777 [Crossref] [ Google Scholar]
- Kamal H, Fornes R, Simin J, Stål P, Duberg AS, Brusselaers N. Risk of hepatocellular carcinoma in hepatitis B and D virus co-infected patients: a systematic review and meta-analysis of longitudinal studies. J Viral Hepat 2021; 28(10):1431-42. doi: 10.1111/jvh.13577 [Crossref] [ Google Scholar]
- Luna-Cuadros MA, Chen HW, Hanif H, Ali MJ, Khan MM, Lau DT. Risk of hepatocellular carcinoma after hepatitis C virus cure. World J Gastroenterol 2022; 28(1):96-107. doi: 10.3748/wjg.v28.i1.96 [Crossref] [ Google Scholar]
- Kaya E, Zedginidze A, Bechmann L, Canbay A. Metabolic dysfunction-associated fatty liver disease (MAFLD) and non-alcoholic fatty liver disease (NAFLD): distinct fatty liver entities with different clinical outcomes?. Hepatobiliary Surg Nutr 2022; 11(2):299-301. doi: 10.21037/hbsn-21-548 [Crossref] [ Google Scholar]
- Alnohair S. Obesity in gulf countries. Int J Health Sci (Qassim) 2014; 8(1):79-83. doi: 10.12816/0006074 [Crossref] [ Google Scholar]
- Teng ML, Ng CH, Huang DQ, Chan KE, Tan DJ, Lim WH. Global incidence and prevalence of nonalcoholic fatty liver disease. Clin Mol Hepatol 2023; 29(Suppl):S32-42. doi: 10.3350/cmh.2022.0365 [Crossref] [ Google Scholar]
- Kim HL, Chung J, Kim KJ, Kim HJ, Seo WW, Jeon KH. Lifestyle modification in the management of metabolic syndrome: statement from Korean Society of CardioMetabolic Syndrome (KSCMS). Korean Circ J 2022; 52(2):93-109. doi: 10.4070/kcj.2021.0328 [Crossref] [ Google Scholar]
- Safiri S, Nejadghaderi SA, Noori M, Sullman MJ, Collins GS, Kaufman JS. Burden of diseases and injuries attributable to alcohol consumption in the Middle East and North Africa region, 1990-2019. Sci Rep 2022; 12(1):19301. doi: 10.1038/s41598-022-22901-x [Crossref] [ Google Scholar]
- Saad-Hussein A, Taha MM, Beshir S, Shahy EM, Shaheen W, Elhamshary M. Carcinogenic effects of aflatoxin B1 among wheat handlers. Int J Occup Environ Health 2014; 20(3):215-9. doi: 10.1179/2049396714y.0000000069 [Crossref] [ Google Scholar]
- Liu Y, Wu F. Global burden of aflatoxin-induced hepatocellular carcinoma: a risk assessment. Environ Health Perspect 2010; 118(6):818-24. doi: 10.1289/ehp.0901388 [Crossref] [ Google Scholar]
- Benkerroum N. Aflatoxins: producing-molds, structure, health issues and incidence in Southeast Asian and sub-Saharan African countries. Int J Environ Res Public Health 2020; 17(4):1215. doi: 10.3390/ijerph17041215 [Crossref] [ Google Scholar]
- Aslani H, Hosseini MS, Mohammadi S, Naghavi-Behzad M. Drinking water disinfection by-products and their carcinogenicity; a review of an unseen crisis. Int J Cancer Manag 2019; 12(5):e88930. doi: 10.5812/ijcm.88930 [Crossref] [ Google Scholar]
- Macias RI, Monte MJ, Serrano MA, González-Santiago JM, Martín-Arribas I, Simão AL. Impact of aging on primary liver cancer: epidemiology, pathogenesis and therapeutics. Aging (Albany NY) 2021; 13(19):23416-34. doi: 10.18632/aging.203620 [Crossref] [ Google Scholar]
- Vaez-Gharamaleki Y, Hosseini MS. Improved access to the innovative anticancer therapies in resource-limited countries: call for global action. Int J Surg 2024; 110(7):4477-8. doi: 10.1097/js9.0000000000001413 [Crossref] [ Google Scholar]
- Kinsey E, Lee HM. Management of hepatocellular carcinoma in 2024: the multidisciplinary paradigm in an evolving treatment landscape. Cancers (Basel) 2024; 16(3):666. doi: 10.3390/cancers16030666 [Crossref] [ Google Scholar]
- Kudo M. The Society for Immunotherapy of Cancer clinical practice guideline on immunotherapy for hepatocellular carcinoma. Hepatobiliary Surg Nutr 2023; 12(2):256-60. doi: 10.21037/hbsn-23-122 [Crossref] [ Google Scholar]