Int J Aging. 2023;1:e18.
doi: 10.34172/ija.2023.e18
Review Article
Immunological and Neurological Changes of COVID-19 in the Elderly
Ahmad Mobed 1, 2, * 
Author information:
1Neurosciences Research Center, Aging Research Institute, Tabriz University of Medical Sciences, Tabriz, Iran
2Department of Microbiology, Faculty of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Objectives:
To investigate the immunological and neurological changes of COVID-19 in the elderly.
Design:
A review study.
Participants:
People over 60 years old with neurological disorders were included in this study.
Outcome measures:
Review of immunological and neurological aspects of COVID-19 in the elderly.
Results:
The novel coronavirus, an acute respiratory syndrome caused by coronavirus 2, has caused an epidemic of the coronavirus disease 2019 (COVID-19) that has infected millions and killed many people worldwide. Moreover, studies showed that mortality is high in the elderly, especially those with comorbidities. Studies have indicated that biological changes in the immune system are a major contributor to the spread of various diseases, especially infectious diseases in the elderly. Therefore, all data and immunological outcomes should be disaggregated and analyzed by age to better understand the heterogeneity between disease incidence and aging.
Conclusions:
Indeed, understanding the pathogenesis of novel coronavirus disease (i.e., COVID-19) and subsequent vaccine development requires prospective studies on the impact of a novel coronavirus, especially on its long-term effects on aging populations in each country.
Keywords: Aging, COVID-19, Pandemic, Viral infections
Introduction
In December 2019, an outbreak of a new infectious respiratory syndrome of unknown etiology was confirmed in Wuhan, China.1,2 As a result of many experiences and studies of the outbreak of severe acute respiratory syndrome (SARS) in 2003, scientists and clinicians around the world organized to identify a new coronavirus. Finally, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was introduced as the causative agent of the disease.1,3 Although this epidemic was dramatically dominant in China, according to the information recorded first in Italy and then in other European countries, the United States of America, and Brazil, the virus spread rapidly around the world and caused significant deaths.4,5 In this regard, governments took urgent measures to prevent further spread of the disease; for example, on March 13, the United States government declared a national emergency, and on March 11, 2020, the World Health Organization (WHO) declared the coronavirus disease 2019 (COVID-19) a global pandemic.6
On March 31, 2020 similar to March 31, 2020, 33% of the population was infected although a large portion of them had no clinical symptoms, according to records filed in New York State. In heterogeneous infections such as COVID-19, host factors are key in determining disease severity and progression.7,8 Studies indicated that many factors such as obesity, smoking, gender, and age are major risk factors for severe disease of COVID-19, and underlying diseases such as type 2 diabetes and high blood pressure are considered aggravating factors.8,9 A wide range of confirmed global data indicated that age is the most important risk factor for severe COVID-19 and its adverse health effects.9 This review includes increased vulnerability in older adults when exposed to COVID-19. In addition, associations between exposure to COVID-19 in older adults and immunological and neurological factors such as psychological and social-environmental changes due to COVID-19 were examined. Furthermore, relevant pathophysiological features that underlie the psychiatric setting and may be exacerbated by SARS-CoV-2 infection were examined. In this study, biological mechanisms such as immune system alterations and inflammation were described appropriately. The focus was on the involvement of mechanisms in aging-related diseases, psychiatric disorders, stress, and infectious diseases such as COVID-19. This review described the increasing vulnerability of older adults to COVID-19 exposure. In addition, the link between exposure to COVID-19 in older adults and the immunological, neurological, psychological, environmental, and social changes caused by COVID-19 was also investigated. Moreover, the pathophysiological features underlying psychiatric attitudes that may be exacerbated by SARS-CoV-2 infection were also considered. Furthermore, biological mechanisms such as changes in the immune system and inflammation were described.
Methods
For our review, we searched PubMed, Google Scholar, and medRxiv for the following keywords: “SARS-CoV-2,” “Pandemic,” “COVID-19,” “Fragile People,” “Mild Cognitive Impairment,” “Psychology,” “Psychiatry,” “Mental Health,” “Elderly “Alzheimer’s Disease,” and “Dementia”. Recently, several new reports related to COVID-19 and its psychosocial impact on vulnerable populations, particularly older adults in general have been critically added.
Results
The Coronavirus Disease 2019 and Aging
Age and age-related diseases are completely dependent on each other, so the number and severity of diseases are directly related to aging. For example, the obtained results suggested that the age-related diseases of 60-year-olds are more and more severe than those of 50-year-olds, and men were twice more likely to die than women of the same age.10 This is because men age faster than women, and men are biologically older than women at any chronological age.10,11 Overall, studies in different countries showed that mortality from COVID-19 increases exponentially with age.12 The exact death rate varies across hundreds of studies because it depends on the test and treatment intervention, but as far as we know, mortality increases exponentially with age.13,14
In Figure 1, nationwide data on the number of hospitalizations (A), ICU admissions (B), and deaths (C) of COVID-19 patients by age group and sex were reported up to May 7, 2020 in France.
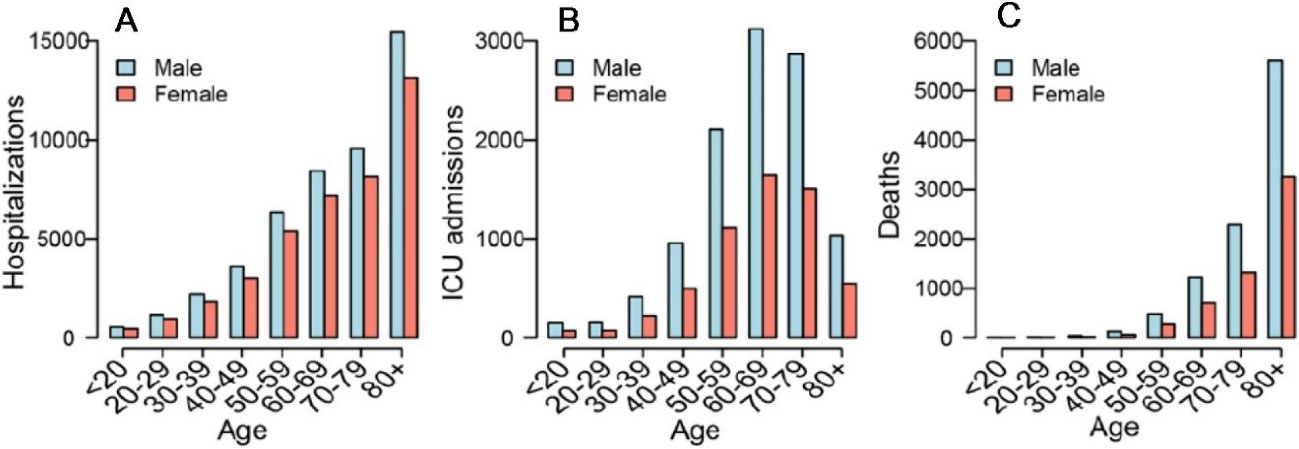
Figure 1.
COVID-19 Hospitalizations and Deaths in France. Note. Growing number of overall ward and ICU hospitalizations, ICU admissions, and deaths from COVID-19 in France. (A) Hospitalizations, (B) ICU Admissions, and (C) Deaths by age group and sex in France. ICU: Intensive care unit. Source Salje et al15
.
COVID-19 Hospitalizations and Deaths in France. Note. Growing number of overall ward and ICU hospitalizations, ICU admissions, and deaths from COVID-19 in France. (A) Hospitalizations, (B) ICU Admissions, and (C) Deaths by age group and sex in France. ICU: Intensive care unit. Source Salje et al15
Longer hospital stays led to more nosocomial infections, putting patients at a potential risk of further complications.16 In general, elderly patients with COVID-19 have distinctive features. The atypical clinical presentation without fever and the most common features of delirium or neurological symptoms may delay diagnosis and increase the risk of mortality. The mortality rate in elderly patients with COVID-19 is thought to be extremely high.17,18 Several factors contribute to this mortality excess, including comorbidities, atypical symptoms, and exclusion from ICU care.18,19 Although age alone is often cited as a significant factor in excluding the elderly from acute care, there is evidence that infirmity is more likely than age to predict risk for poor prognosis in this category.19
Elderly Immune Response to the Coronavirus Disease 2019
Aging brings about several important alterations in the adaptive and innate domains of immunity. This process, known as immunosenescence, significantly weakens the immune defenses against infections, negatively affecting the health and well-being of a significant portion of older adults. On the other hand, aging is a biological process related to disease and death. This process is reflected in molecular properties such as epigenetic changes and telomere attrition.20,21 Although the biological basis for the susceptibility of long-term care facility residents to patients with severe COVID-19 is unclear, age alone is an extremely strong clinical factor that has a significant effect on the immune system.22,23 Immunosenescence is the age-related decline in immune function that may be an important factor leading to severe disease. Antibody levels and quality as well as cellular responses to pathogens decline with age, which may contribute to the increased infection rate of COVID-19 infection in the elderly.24,25 These factors also strengthen the suboptimal immune responses perceived in response to vaccines such as influenza and shingles vaccines.26,27 Additionally, many residents suffer from multiple comorbidities, making them more likely to have serious consequences after infection.27,28 In response to viral replication, macrophages and hyper-functional monocytes infiltrate the lung, causing hyper-inflammation and hyper-secretion of cytokines such as interferon-γ inducible protein-10, interleukin (IL)-2, IL-6, IL-7, IL-1ra, monocyte chemoattractant protein-1, tumor necrosis factor-α, ferritin, C-reactive protein, macrophage inflammatory protein 1-α, granulocyte-colony stimulating factor, and procalcitonin.29-31
Age is now recognized as a major risk factor for COVID-19 complications. COVID-19 complications in the elderly are known and extensively studied due to the dysregulation of immune function, vaccination response, and inflammation, and it has been speculated that immunosenescence is a critical factor in the outcome of SARS-CoV-2 infection.32 On the other hand, the relative impact of immune system dysregulation on virulence during COVID-19 in the elderly (or indeed anyone) is still poorly understood.33,34 Some important immunological variations in old adults are summarized in Table 1.
Table 1.
Some Important Immunological Variation in Old Adult
|
Immunological Factor
|
Variations
|
Ref
|
| Thymic involution |
Thymic output↓, Adiposity in thymus↑, Thymic epithelial cells↓, IL-7 production↓ |
35
|
| T lymphocytes |
Native T cell pool↓, Memory T cell↑, TCR diversity↓, CD8↑, CD4↓ |
35,36
|
| B lymphocytes |
Native B cell pool↓, Memory B cells↑, IgM, IgD serum level↓, IgG, IgA serum level↑ |
36
|
| Hematological biomarkers |
LDH↑, ALT↓, AST↑ |
|
| Inflamm-aging |
Inflammatory mediators↑, IL-6↑, CRP↑, Tissue dysfunction↑ |
37
|
| Cytokine |
(IFN)-γ↓, TH1 ↓, IL-4 and IL-10↑, CD45RO + /CD8 + T cells ↓ |
38
|
| Overall changes |
Telomerase activity↓, Tomur incidence↑, Infection susceptibility↑, Auto immune/inflammatory reaction↑, Immune response to vaccination↓ |
37
|
Note. IL: Interleukin; TNF: Tumor necrosis factor; CRP: C-reactive protein; LDH: Lactate dehydrogenase; ALT: Alanine aminotransferase; AST: Aspartate aminotransferase; IFN-γ: Interferon-gamma.
In sum, for severe COVID-19, five key points of attention in the immune response may be affected by the aging immune system: (A) Increased underlying inflammation (inflammation) at the SARS-CoV-2 vaccination site may expose older adults to a previously inflammatory local environment. (B) Aging-associated innate immune cell dysfunction may impair primary immune response. (C) Late and/or impaired adaptive responses are due to reduced clonal diversity, preexisting weak or ineffectual immunity, and deprived T-cell priming. (D) The decline in T-cell function and antibody response may be due to the immune aging process, and (E) The potential for reduced memory reactivity and potentially long-term effects on the immune system may promote immunodeficiency phenotypes.
The Coronavirus Disease 2019 Clinical Manifestation in Older Adults
About 50% of patients over 60 years of age suffer from the classic triad of symptoms associated with SARS-CoV-2, including fever, cough, and shortness of breath.39,40 Although fever and cough are the most common symptoms among the elderly, young people with healthy immune systems may also have the triad of symptoms.40 Hypothermia in some patients can have many causes, including thermoregulatory disturbances, low basal body temperature, and certain medications in older people.41 In addition, phlegm production and shortness of breath are more common in older people than in other age groups. Elderly patients are less likely to exhibit typical COVID-19 symptoms and more likely to exhibit unusual SARS-CoV-2 symptoms such as confusion, falls, and significant gastrointestinal symptoms.41,42
Accordingly, a retrospective study on 141 people aged 50 years and older with SARS-CoV-2 infection confirmed that the most common clinical presentation of COVID-19 disease in older adults includes typical symptoms, especially cough (61.4%), fever (79.5%), and shortness of breath (31.8%) at the age of 65-79 as well as shortness of breath (25.5%), fever (75.0%), cough (43.8%), and fatigue (25.5%) for people aged 80 years and older.39 Indeed, with advanced age, the inconsistency in clinical demonstration of COVID-19 is greater due to a higher incidence of atypical symptoms and signs such as gastrointestinal disturbances (e.g., nausea, diarrhea, and vomiting), hypotension, delirium, and falls.43
Common Diseases Related to the Coronavirus Disease 2019 in the Elderly
Comorbidities are the main challenge in the control and treatment of COVID-19 in the elderly. The novel coronavirus primarily causes pulmonary infections and increases the strain on the heart.44,45 At the same time, high blood sugar levels make the control of infections difficult (see Figure 2). The coexisting multisystem disease features create a complex disease in the elderly that is more difficult to treat.44,46 Additionally, elderly patients are prone to multisystem organ failure that develops other systemic complications such as renal failure, gastrointestinal bleeding, delirium, disseminated intravascular coagulation, and deep vein thrombosis.46 Frequent infectious diseases have led to an increase in the death rate among the elderly and are the main challenges in implementing appropriate preventive measures and future strategies to protect the elderly. These include worsening conditions, weakened immune function, reduced organ function, and increased susceptibility to multiple underlying diseases. Illness and the lack of attention to personal health make older people vulnerable to a variety of illnesses.47,48 In addition, immunodeficiency decreases receptor expression, and severe pathophysiological reactions in the elderly can lead to functional impairment. Despite many ailments, mental health is one of the most important pillars of public health for older people. Regular telephone counseling, contact with family members, the provision of appropriate and timely information on the epidemic, continued supply of generic drugs, addressing psychological needs, and instilling respect are essential. On the other hand, respect and dignity are considered highly valuable in maintaining the mental health of older adults.48
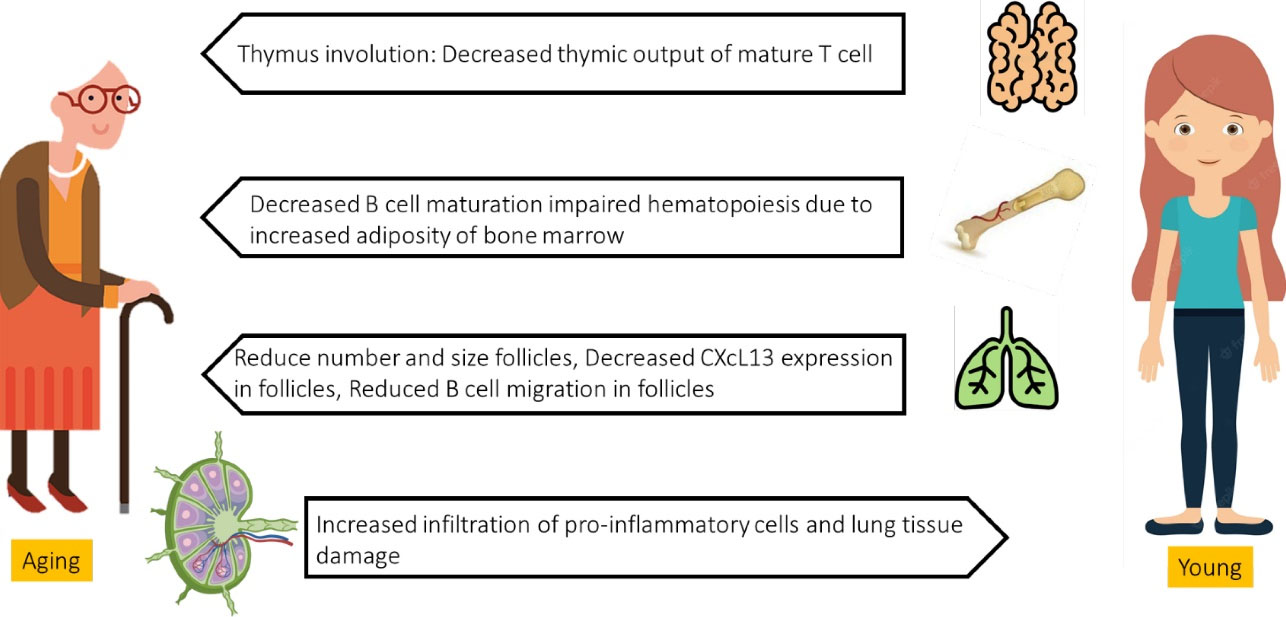
Figure 2.
Immune System in Aging. Note. The degeneration of the main lymphoid organs reduces the assembly of naive T and B cells, resulting in decreased migration to secondary lymphoid organs and locates of antigen exposure. In addition, the lungs and extrapulmonary organs are vulnerable to the buildup of pro-inflammatory cells and mediators, adapted from Bajaj et al3
.
Immune System in Aging. Note. The degeneration of the main lymphoid organs reduces the assembly of naive T and B cells, resulting in decreased migration to secondary lymphoid organs and locates of antigen exposure. In addition, the lungs and extrapulmonary organs are vulnerable to the buildup of pro-inflammatory cells and mediators, adapted from Bajaj et al3
The COVID-19, risk factors and challenges are illustrated in Figure 3.
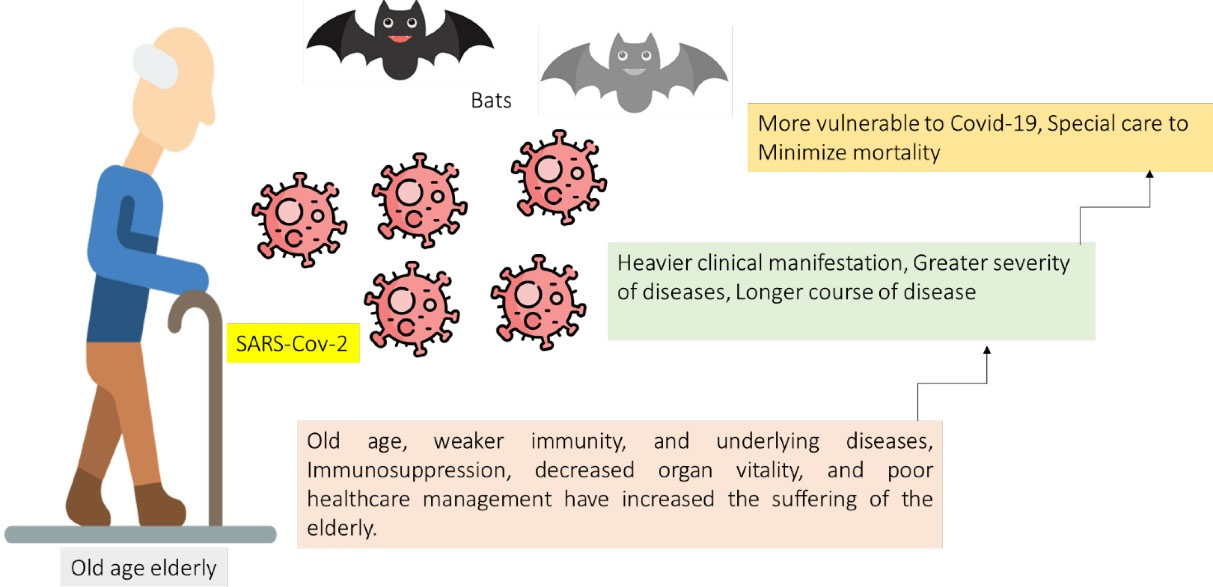
Figure 3.
COVID-19 Risk Factors and Challenges. Note. A good diet, adequate nutrition, allergies, and COVID-19 vaccination are protective factors against COVID-19 infection and development and increases anti-inflammatory cytokines; further, a decrease in ACE2 expression could contribute to the protective effects of these factors. Moreover, the induction of antibody responses and T-cell activation by COVID-19 immunizations can also help prevent infection, progression, and poor clinical outcomes, adapted from Niu et al39 and Guo et al.40 COVID-19: Coronavirus disease 2019
.
COVID-19 Risk Factors and Challenges. Note. A good diet, adequate nutrition, allergies, and COVID-19 vaccination are protective factors against COVID-19 infection and development and increases anti-inflammatory cytokines; further, a decrease in ACE2 expression could contribute to the protective effects of these factors. Moreover, the induction of antibody responses and T-cell activation by COVID-19 immunizations can also help prevent infection, progression, and poor clinical outcomes, adapted from Niu et al39 and Guo et al.40 COVID-19: Coronavirus disease 2019
As illustrated in Figure 3, in addition to increased viral susceptibility/virulence or infection rate, immune response dysregulation and hyper-inflammation significantly increased COVID-19 pathophysiology, resulting in increased disease severity.30,49 Preventive interventions should focus on the unique health as well as nutritional, psychological, and spiritual well-being needs of older people. Physical isolation, social distancing, and proper hand and respiratory hygiene must be supported by the provision of personal protective equipment, environmental disinfection, and nutritious meals.30,49
Additionally, mechanisms and risk factors associated with the exacerbation of COVID-19 in older adults are illustrated in Figure 4.
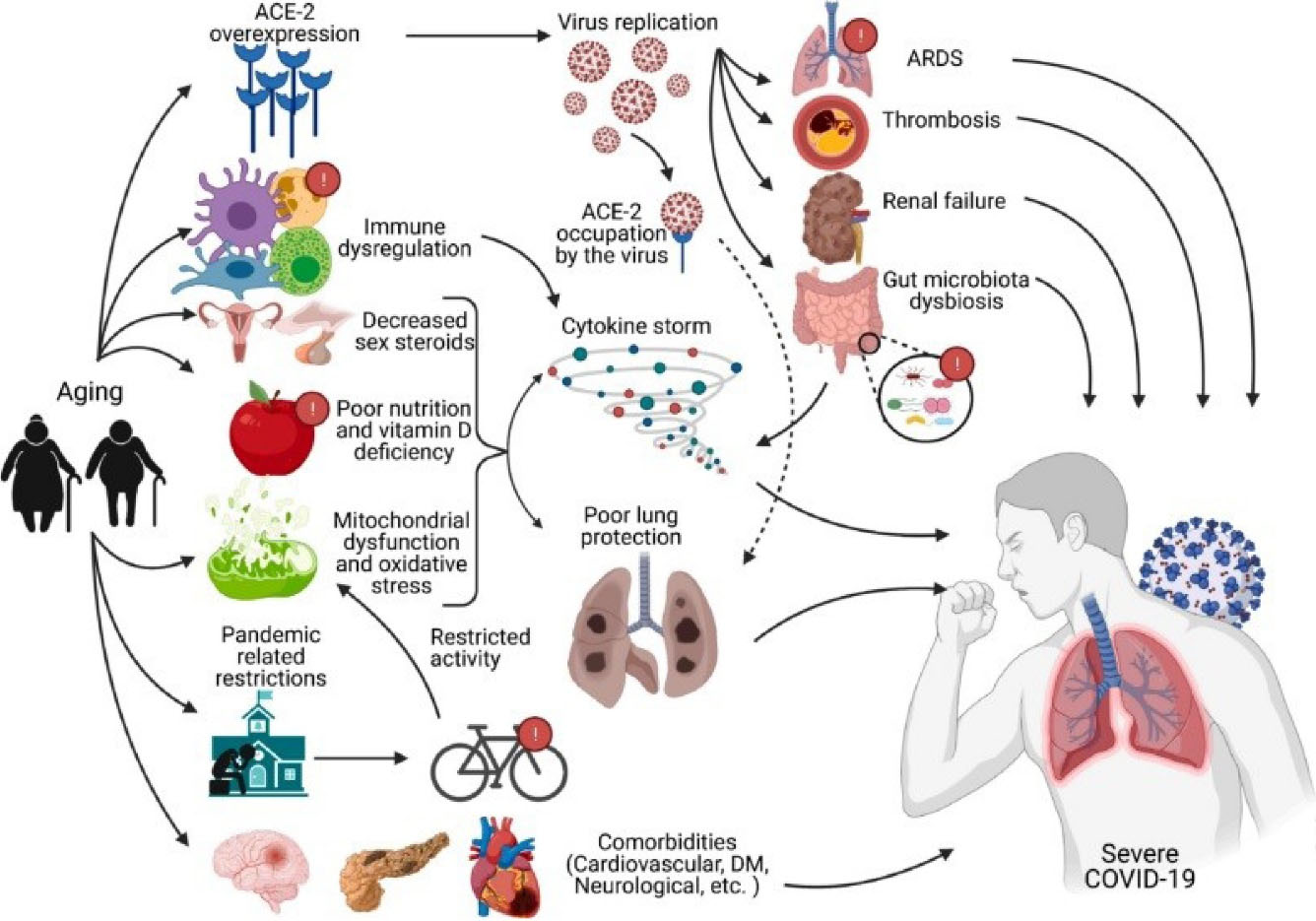
Figure 4.
Mechanisms and Risk Factors Associated with Exacerbation of COVID-19 in Older Adults. Note. In older adults, COVID-19 is associated with immunodeficiency, ACE-2 overexpression, decreased sex steroid secretion, mitochondrial dysfunction, oxidative stress, poor diet, vitamin D deficiency, comorbidities, and reduced physical activity, leading to a pandemic. It is exacerbated by related restrictions. These effects result in increased viral replication, cytokine storm, and reduced lung protection against viruses. Complications of COVID-19 such as ARDS, thrombosis, and renal failure are also common in older people and ultimately lead to severe COVID-19, with permission from Farshbafnadi et al.50 COVID-19: Coronavirus disease 2019; Ace-2: angiotensin-converting enzyme 2; ARDS: Acute respiratory distress syndrome
.
Mechanisms and Risk Factors Associated with Exacerbation of COVID-19 in Older Adults. Note. In older adults, COVID-19 is associated with immunodeficiency, ACE-2 overexpression, decreased sex steroid secretion, mitochondrial dysfunction, oxidative stress, poor diet, vitamin D deficiency, comorbidities, and reduced physical activity, leading to a pandemic. It is exacerbated by related restrictions. These effects result in increased viral replication, cytokine storm, and reduced lung protection against viruses. Complications of COVID-19 such as ARDS, thrombosis, and renal failure are also common in older people and ultimately lead to severe COVID-19, with permission from Farshbafnadi et al.50 COVID-19: Coronavirus disease 2019; Ace-2: angiotensin-converting enzyme 2; ARDS: Acute respiratory distress syndrome
Discussion
In many countries, isolation was considered an essential solution. However, some studies have found that social isolation in the elderly is a “serious public health concern” due to the increased risk of cardiovascular disease, autoimmune disease, neurocognitive disorders, and mental health problems.51
Older age is one of the predictors of poor prognosis, so elderly patients with COVID-19 are at increased risk of severe and fatal complications.52 Due to worsening health conditions and comorbidities, elderly patients with COVID-19 are more likely to be hospitalized for longer periods and are more likely to require additional medical resources, so improving patient care is critical.52,53 Remdesivir is currently the only available antiviral drug that is effective against moderate to severe SARS-CoV-2, and its mechanism of action involves the inhibition of the viral RNA-dependent polymerase. Elevated aminotransferase and/or serum creatinine is one of the main side effects of remdesivir.54 This requires special attention as hepatic and renal dysfunction with remdesivir can be severe54; therefore, caution should be exercised when administering remdesivir to elderly patients with reduced visceral function.55 Furthermore, elderly patients with COVID-19 are at high risk of exacerbations requiring treatment with remdesivir. However, the safety of remdesivir, especially in elderly patients, is unknown in clinical practice.55 There are currently no other effective antiviral drugs available for the treatment of moderate to severe novel coronavirus disease (i.e., COVID-19).56 The knowledge of remdesivir safety is therefore essential for older patients, and extra research is needed to evaluate the safety of remdesivir in elderly patients with COVID-19, particularly those who are being treated in hospitals.57 Well-timed antiviral therapy primary in the disease course is strongly recommended for patients with COVID-19, especially older patients and those with underlying medical conditions.57,58 Researchers retrospectively reviewed clinical data from 280 COVID-19 cases, recommending the timely initiation of antiviral therapy to slow disease progression and improve prognosis in older patients. So far, Oseltamivir, which may reduce mortality in influenza patients, and ganciclovir, which is primarily used to treat cytomegalovirus, have been widely used in SARS-CoV-2 patients.58,59 However, the efficacy of neuraminidase inhibitors is now questionable and is no longer recommended.59 Remdesivir (GS-5734) is a monophosphoramidate prodrug of an adenosine analog that affects viral RNA polymerase and reduces viral RNA production.60 Remdesivir showed significant therapeutic efficacy in a Middle East respiratory syndrome coronavirus mouse model.60 This finding suggested that a patient treated with Nirmatrelvir/ritonavir was more likely to have a negative test within 10 days of his/her first positive test.61,62 This benefit of Nirmatrelvir/ritonavir persisted after adjusting for relevant confounding factors such as COVID-19 immunization status and also in specific subgroups such as immunosuppressed and elderly patients.61,62
Conclusions and Recommendations
The main results of this study indicated that people who die from COVID-19 have high levels of comorbidities at all ages, but a minority of healthy adults without underlying medical conditions die. due to common non-respiratory complications. Hence, it was recommended that respiratory disease should be combined with strategies to prevent and reduce the impact of non-respiratory complications; furthermore, hospitalized patients who died from COVID-19 worldwide had a variety of complications regardless of age. However, the occurrence of some deaths in young adult patients without underlying medical conditions suggests that COVID-19 can also affect healthy people. Finally, further research is needed to identify the contribution of aging to other serious viral diseases and to elucidate the mechanisms underlying age-related onset potential. During quarantine due to COVID-19, the level of physical activity among older people around the world decreased. In the current pandemic scenario, fitness strategies with age-appropriate exercise should be promoted to maintain and improve the health of this population. Studies suggest that older age may reduce the mental health impact of COVID-19. Despite popular perceptions and conflicting evidence about vulnerability, the ability of older adults to adapt to adversity varies according to cultural, social, economic, and other personal factors. Overall, the impacts and long-term effects of COVID-19 are expected to vary across countries and older populations and have yet to be evaluated in prospective longitudinal studies.
Acknowledgments
The author would like to express their gratitude to the Department of Microbiology, Faculty of Medicine and Aging Research Institute, Tabriz University of Medical Sciences, Tabriz, Iran.
Funding
This study was supported by the Department of Microbiology, School of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran, and Aging Research Institute, Faculty of Medicine, Tabriz University of Medical Sciences, Iran.
Data availability statement
Not applicable.
Ethical approval
Not applicable.
Consent for publication
Not applicable.
Conflict of interests
The author declares that he has no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Sharma A, Tiwari S, Deb MK, Marty JL. Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2): a global pandemic and treatment strategies. Int J Antimicrob Agents 2020; 56(2):106054. doi: 10.1016/j.ijantimicag.2020.106054 [Crossref] [ Google Scholar]
- Law S, Leung AW, Xu C. Severe acute respiratory syndrome (SARS) and coronavirus disease-2019 (COVID-19): from causes to preventions in Hong Kong. Int J Infect Dis 2020; 94:156-63. doi: 10.1016/j.ijid.2020.03.059 [Crossref] [ Google Scholar]
- Bajaj V, Gadi N, Spihlman AP, Wu SC, Choi CH, Moulton VR. Aging, immunity, and COVID-19: how age influences the host immune response to coronavirus infections?. Front Physiol 2020; 11:571416. doi: 10.3389/fphys.2020.571416 [Crossref] [ Google Scholar]
- Khan I, Haleem A, Javaid M. Analysing COVID-19 pandemic through cases, deaths, and recoveries. J Oral Biol Craniofac Res 2020; 10(4):450-69. doi: 10.1016/j.jobcr.2020.08.003 [Crossref] [ Google Scholar]
- Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 2020; 323(18):1775-6. doi: 10.1001/jama.2020.4683 [Crossref] [ Google Scholar]
- Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020; 579(7798):270-3. doi: 10.1038/s41586-020-2012-7 [Crossref] [ Google Scholar]
- Minaee S, Kafieh R, Sonka M, Yazdani S, Jamalipour Soufi G. Deep-COVID: predicting COVID-19 from chest X-ray images using deep transfer learning. Med Image Anal 2020; 65:101794. doi: 10.1016/j.media.2020.101794 [Crossref] [ Google Scholar]
- Garibaldi BT, Fiksel J, Muschelli J, Robinson ML, Rouhizadeh M, Perin J. Patient trajectories among persons hospitalized for COVID-19: a cohort study. Ann Intern Med 2021; 174(1):33-41. doi: 10.7326/m20-3905 [Crossref] [ Google Scholar]
- Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med 2020; 180(7):934-43. doi: 10.1001/jamainternmed.2020.0994 [Crossref] [ Google Scholar]
- Blagosklonny MV. Why men age faster but reproduce longer than women: mTOR and evolutionary perspectives. Aging (Albany NY) 2010; 2(5):265-73. doi: 10.18632/aging.100149 [Crossref] [ Google Scholar]
- Jin JM, Bai P, He W, Wu F, Liu XF, Han DM. Gender differences in patients with COVID-19: focus on severity and mortality. Front Public Health 2020; 8:152. doi: 10.3389/fpubh.2020.00152 [Crossref] [ Google Scholar]
- Palaiodimos L, Kokkinidis DG, Li W, Karamanis D, Ognibene J, Arora S. Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York. Metabolism 2020; 108:154262. doi: 10.1016/j.metabol.2020.154262 [Crossref] [ Google Scholar]
- Zhavoronkov A. Geroprotective and senoremediative strategies to reduce the comorbidity, infection rates, severity, and lethality in gerophilic and gerolavic infections. Aging (Albany NY) 2020; 12(8):6492-510. doi: 10.18632/aging.102988 [Crossref] [ Google Scholar]
- Lu Q, Shi Y. Coronavirus disease (COVID-19) and neonate: what neonatologist need to know. J Med Virol 2020; 92(6):564-7. doi: 10.1002/jmv.25740 [Crossref] [ Google Scholar]
- Salje H, Tran Kiem C, Lefrancq N, Courtejoie N, Bosetti P, Paireau J. Estimating the burden of SARS-CoV-2 in France. Science 2020; 369(6500):208-11. doi: 10.1126/science.abc3517 [Crossref] [ Google Scholar]
- Thümmler L, Lindemann M, Horn PA, Lenz V, Konik M, Gäckler A. Early treatment with monoclonal antibodies or convalescent plasma reduces mortality in non-vaccinated COVID-19 high-risk patients. Viruses 2022; 15(1):119. doi: 10.3390/v15010119 [Crossref] [ Google Scholar]
- Perrotta F, Corbi G, Mazzeo G, Boccia M, Aronne L, D’Agnano V. COVID-19 and the elderly: insights into pathogenesis and clinical decision-making. Aging Clin Exp Res 2020; 32(8):1599-608. doi: 10.1007/s40520-020-01631-y [Crossref] [ Google Scholar]
- Guo YR, Cao QD, Hong ZS, Tan YY, Chen SD, Jin HJ. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res 2020; 7(1):11. doi: 10.1186/s40779-020-00240-0 [Crossref] [ Google Scholar]
- Mostaza JM, García-Iglesias F, González-Alegre T, Blanco F, Varas M, Hernández-Blanco C. Clinical course and prognostic factors of COVID-19 infection in an elderly hospitalized population. Arch Gerontol Geriatr 2020; 91:104204. doi: 10.1016/j.archger.2020.104204 [Crossref] [ Google Scholar]
- Kumar A, Dowling WE, Román RG, Chaudhari A, Gurry C, Le TT. Status report on COVID-19 vaccines development. Curr Infect Dis Rep 2021; 23(6):9. doi: 10.1007/s11908-021-00752-3 [Crossref] [ Google Scholar]
- Scartoni FR, de Oliveira Sant’Ana L, Murillo-Rodriguez E, Yamamoto T, Imperatori C, Budde H. Physical exercise and immune system in the elderly: implications and importance in COVID-19 pandemic period. Front Psychol 2020; 11:593903. doi: 10.3389/fpsyg.2020.593903 [Crossref] [ Google Scholar]
- Ciabattini A, Nardini C, Santoro F, Garagnani P, Franceschi C, Medaglini D. Vaccination in the elderly: the challenge of immune changes with aging. Semin Immunol 2018; 40:83-94. doi: 10.1016/j.smim.2018.10.010 [Crossref] [ Google Scholar]
- Pereira B, Xu XN, Akbar AN. Targeting inflammation and immunosenescence to improve vaccine responses in the elderly. Front Immunol 2020; 11:583019. doi: 10.3389/fimmu.2020.583019 [Crossref] [ Google Scholar]
- Krutikov M, Palmer T, Tut G, Fuller C, Shrotri M, Williams H. Incidence of SARS-CoV-2 infection according to baseline antibody status in staff and residents of 100 long-term care facilities (VIVALDI): a prospective cohort study. Lancet Healthy Longev 2021; 2(6):e362-e70. doi: 10.1016/s2666-7568(21)00093-3 [Crossref] [ Google Scholar]
- Jergović M, Coplen CP, Uhrlaub JL, Nikolich-Žugich J. Immune response to COVID-19 in older adults. J Heart Lung Transplant 2021; 40(10):1082-9. doi: 10.1016/j.healun.2021.04.017 [Crossref] [ Google Scholar]
- McElhaney JE, Verschoor CP, Andrew MK, Haynes L, Kuchel GA, Pawelec G. The immune response to influenza in older humans: beyond immune senescence. Immun Ageing 2020; 17:10. doi: 10.1186/s12979-020-00181-1 [Crossref] [ Google Scholar]
- Damiot A, Pinto AJ, Turner JE, Gualano B. Immunological implications of physical inactivity among older adults during the COVID-19 pandemic. Gerontology 2020; 66(5):431-8. doi: 10.1159/000509216 [Crossref] [ Google Scholar]
- Chua JV, Chen WH. Herpes zoster vaccine for the elderly: boosting immunity. Aging health 2010; 6(2):169-76. doi: 10.2217/ahe.10.5 [Crossref] [ Google Scholar]
- Korakas E, Ikonomidis I, Kousathana F, Balampanis K, Kountouri A, Raptis A. Obesity and COVID-19: immune and metabolic derangement as a possible link to adverse clinical outcomes. Am J Physiol Endocrinol Metab 2020; 319(1):E105-E9. doi: 10.1152/ajpendo.00198.2020 [Crossref] [ Google Scholar]
- Akhmerov A, Marbán E. COVID-19 and the heart. Circ Res 2020; 126(10):1443-55. doi: 10.1161/circresaha.120.317055 [Crossref] [ Google Scholar]
- McGonagle D, Sharif K, O’Regan A, Bridgewood C. The role of cytokines including interleukin-6 in COVID-19 induced pneumonia and macrophage activation syndrome-like disease. Autoimmun Rev 2020; 19(6):102537. doi: 10.1016/j.autrev.2020.102537 [Crossref] [ Google Scholar]
- Chen Y, Klein SL, Garibaldi BT, Li H, Wu C, Osevala NM. Aging in COVID-19: vulnerability, immunity and intervention. Ageing Res Rev 2021; 65:101205. doi: 10.1016/j.arr.2020.101205 [Crossref] [ Google Scholar]
- Connors J, Taramangalam B, Cusimano G, Bell MR, Matt SM, Runner K. Aging alters antiviral signaling pathways resulting in functional impairment in innate immunity in response to pattern recognition receptor agonists. Geroscience 2022; 44(5):2555-72. doi: 10.1007/s11357-022-00612-5 [Crossref] [ Google Scholar]
- Teo SP. Review of COVID-19 vaccines and their evidence in older adults. Ann Geriatr Med Res 2021; 25(1):4-9. doi: 10.4235/agmr.21.0011 [Crossref] [ Google Scholar]
- Rivera-Torres J, Girón N, San José E. COVID-19: a comprehensive review on cardiovascular alterations, immunity, and therapeutics in older adults. J Clin Med 2023; 12(2):448. doi: 10.3390/jcm12020488 [Crossref] [ Google Scholar]
- Watanabe BT, Beretta OC, da Silva EF, Assy JG, Fernandes EV, Gouvêa-e-Silva LF. [Evaluation of the biochemical, hematological and immunological profile in patients with a recent diagnosis of HIV in Santarém Reference Center, Pará, Brasil]. Rev Med (Sao Paulo) 2022; 101(3):e-189140. doi: 10.11606/issn.1679-9836.v101i3e-189140 [Crossref] [ Google Scholar]
- Schneider-Crease IA, Feder JA, Baniel A, McCann C, Haile AA, Abebe B. Urinary neopterin reflects immunological variation associated with age, helminth parasitism, and the microbiome in a wild primate. Sci Rep 2022; 12(1):21307. doi: 10.1038/s41598-022-25298-9 [Crossref] [ Google Scholar]
- Rink L, Cakman I, Kirchner H. Altered cytokine production in the elderly. Mech Ageing Dev 1998; 102(2-3):199-209. doi: 10.1016/s0047-6374(97)00153-x [Crossref] [ Google Scholar]
- Niu S, Tian S, Lou J, Kang X, Zhang L, Lian H. Clinical characteristics of older patients infected with COVID-19: a descriptive study. Arch Gerontol Geriatr 2020; 89:104058. doi: 10.1016/j.archger.2020.104058 [Crossref] [ Google Scholar]
- Guo T, Shen Q, Guo W, He W, Li J, Zhang Y. Clinical characteristics of elderly patients with COVID-19 in Hunan province, China: a multicenter, retrospective study. Gerontology 2020; 66(5):467-75. doi: 10.1159/000508734 [Crossref] [ Google Scholar]
- Mulinari Turin de Oliveira N, Fernandes da Silva Figueiredo I, Cristine Malaquias da Silva L, Sauruk da Silva K, Regis Bueno L, Barbosa da Luz B. Tissue proteases and immune responses: influencing factors of COVID-19 severity and mortality. Pathogens 2020; 9(10):817. doi: 10.3390/pathogens9100817 [Crossref] [ Google Scholar]
- Chen T, Dai Z, Mo P, Li X, Ma Z, Song S. Clinical characteristics and outcomes of older patients with coronavirus disease 2019 (COVID-19) in Wuhan, China: a single-centered, retrospective study. J Gerontol A Biol Sci Med Sci 2020; 75(9):1788-95. doi: 10.1093/gerona/glaa089 [Crossref] [ Google Scholar]
- Martín-Sánchez FJ, Del Toro E, Cardassay E, Valls Carbó A, Cuesta F, Vigara M. Clinical presentation and outcome across age categories among patients with COVID-19 admitted to a Spanish Emergency Department. Eur Geriatr Med 2020; 11(5):829-41. doi: 10.1007/s41999-020-00359-2 [Crossref] [ Google Scholar]
- Hashim MJ, Alsuwaidi AR, Khan G. Population risk factors for COVID-19 mortality in 93 countries. J Epidemiol Glob Health 2020; 10(3):204-8. doi: 10.2991/jegh.k.200721.001 [Crossref] [ Google Scholar]
- Sobotka T, Brzozowska Z, Muttarak R, Zeman K, di Lego V. Age, gender and COVID-19 infections. medRxiv [Preprint]. May 26, 2020. Available from: https://www.medrxiv.org/content/10.1101/2020.05.24.20111765v1.
- Batsis JA, Daniel K, Eckstrom E, Goldlist K, Kusz H, Lane D. Promoting healthy aging during COVID-19. J Am Geriatr Soc 2021; 69(3):572-80. doi: 10.1111/jgs.17035 [Crossref] [ Google Scholar]
- Ahrenfeldt LJ, Otavova M, Christensen K, Lindahl-Jacobsen R. Sex and age differences in COVID-19 mortality in Europe. Wien Klin Wochenschr 2021; 133(7-8):393-8. doi: 10.1007/s00508-020-01793-9 [Crossref] [ Google Scholar]
- Zheng Y, Liu X, Le W, Xie L, Li H, Wen W. A human circulating immune cell landscape in aging and COVID-19. Protein Cell 2020; 11(10):740-70. doi: 10.1007/s13238-020-00762-2 [Crossref] [ Google Scholar]
- Bianchetti A, Bellelli G, Guerini F, Marengoni A, Padovani A, Rozzini R. Improving the care of older patients during the COVID-19 pandemic. Aging Clin Exp Res 2020; 32(9):1883-8. doi: 10.1007/s40520-020-01641-w [Crossref] [ Google Scholar]
- Farshbafnadi M, Kamali Zonouzi S, Sabahi M, Dolatshahi M, Aarabi MH. Aging & COVID-19 susceptibility, disease severity, and clinical outcomes: the role of entangled risk factors. Exp Gerontol 2021; 154:111507. doi: 10.1016/j.exger.2021.111507 [Crossref] [ Google Scholar]
- Santini ZI, Jose PE, York Cornwell E, Koyanagi A, Nielsen L, Hinrichsen C. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health 2020; 5(1):e62-e70. doi: 10.1016/s2468-2667(19)30230-0 [Crossref] [ Google Scholar]
- Tiseo G, Barbieri C, Galfo V, Occhineri S, Matucci T, Almerigogna F. Efficacy and safety of nirmatrelvir/ritonavir, molnupiravir, and remdesivir in a real-world cohort of outpatients with COVID-19 at high risk of progression: the PISA Outpatient Clinic Experience. Infect Dis Ther 2023; 12(1):257-71. doi: 10.1007/s40121-022-00729-2 [Crossref] [ Google Scholar]
- Napoli C, Tritto I, Benincasa G, Mansueto G, Ambrosio G. Cardiovascular involvement during COVID-19 and clinical implications in elderly patients A review. Ann Med Surg (Lond) 2020; 57:236-43. doi: 10.1016/j.amsu.2020.07.054 [Crossref] [ Google Scholar]
- Hickman MR, Saunders DL, Bigger CA, Kane CD, Iversen PL. The development of broad-spectrum antiviral medical countermeasures to treat viral hemorrhagic fevers caused by natural or weaponized virus infections. PLoS Negl Trop Dis 2022; 16(3):e0010220. doi: 10.1371/journal.pntd.0010220 [Crossref] [ Google Scholar]
- Li P, Liu Y, Cheng Z, Yu X, Li Y. COVID-19-associated liver injury: clinical characteristics, pathophysiological mechanisms and treatment management. Biomed Pharmacother 2022; 154:113568. doi: 10.1016/j.biopha.2022.113568 [Crossref] [ Google Scholar]
- Ng TI, Correia I, Seagal J, DeGoey DA, Schrimpf MR, Hardee DJ. Antiviral drug discovery for the treatment of COVID-19 infections. Viruses 2022; 14(5):961. doi: 10.3390/v14050961 [Crossref] [ Google Scholar]
- Custodero C, Veronese N, Topinkova E, Michalkova H, Polidori MC, Cella A. The role of multidimensional prognostic index to identify hospitalized older adults with COVID-19 who can benefit from remdesivir treatment: an observational, prospective, multicenter study. Drugs Aging 2023; 40(7):643-51. doi: 10.1007/s40266-023-01036-2 [Crossref] [ Google Scholar]
- Ramos-Rincon JM, López-Carmona MD, Cobos-Palacios L, López-Sampalo A, Rubio-Rivas M, Martín-Escalante MD. Remdesivir in very old patients ( ≥ 80 Years) hospitalized with COVID-19: real world data from the SEMI-COVID-19 registry. J Clin Med 2022; 11(13):3769. doi: 10.3390/jcm11133769 [Crossref] [ Google Scholar]
- Lai CC, Wei JCC. Is inhaled zanamivir non-inferior to oral oseltamivir in the treatment of outpatients with influenza?. Clin Infect Dis 2022; 75(6):1112-3. doi: 10.1093/cid/ciac335 [Crossref] [ Google Scholar]
- Ader F, Bouscambert-Duchamp M, Hites M, Peiffer-Smadja N, Poissy J, Belhadi D. Remdesivir plus standard of care versus standard of care alone for the treatment of patients admitted to hospital with COVID-19 (DisCoVeRy): a phase 3, randomised, controlled, open-label trial. Lancet Infect Dis 2022; 22(2):209-21. doi: 10.1016/s1473-3099(21)00485-0 [Crossref] [ Google Scholar]
- Brown AJ, Won JJ, Graham RL, Dinnon KH, 3rd 3rd, Sims AC, Feng JY. Broad spectrum antiviral remdesivir inhibits human endemic and zoonotic deltacoronaviruses with a highly divergent RNA dependent RNA polymerase. Antiviral Res 2019; 169:104541. doi: 10.1016/j.antiviral.2019.104541 [Crossref] [ Google Scholar]
- Sheahan TP, Sims AC, Leist SR, Schäfer A, Won J, Brown AJ. Comparative therapeutic efficacy of remdesivir and combination lopinavir, ritonavir, and interferon beta against MERS-CoV. Nat Commun 2020; 11(1):222. doi: 10.1038/s41467-019-13940-6 [Crossref] [ Google Scholar]