Int J Aging. 2024;2:e5.
doi: 10.34172/ija.2024.e5
Original Article
The Relationship Between Air Pollution Components and Hospitalizations Due to Acute Pulmonary Embolism
Ali Soleimany 1  , Saeed Ghanbari Kaljahi 2, Reza Hajizadeh 1, *
, Saeed Ghanbari Kaljahi 2, Reza Hajizadeh 1, * 
Author information:
1Department of Cardiology, School of Medicine, Urmia University of Medical Sciences, Urmia, Iran
2Student Research Committee, School of Medicine, Urmia University of Medical Sciences, Urmia, Iran
Abstract
Objectives:
This study was conducted to examine the relationship between air pollution and pulmonary embolism in patients hospitalized in Urmia city. This cross-sectional study was conducted in West Azerbaijan province, Iran. According to the daily report from the meteorology center of West Azarbaijan province, the data on the concentrations of air pollutants, including PM10, NO2, O3, CO, and PM2.5 were extracted. Moreover, the files of patients without underlying risk factors hospitalized due to pulmonary embolism were extracted. Finally, admissions from 2 days before until 2 days after the polluted days were compared to hospitalizations on clean air days of the same month.
Design:
A cross-sectional study.
Setting(s):
Urmia, the capital city of the West Azerbaijan province in northwestern Iran.
Participants:
A total of 1275 patients without underlying risk factors hospitalized due to pulmonary embolism were included.
Outcome measures:
Admissions from 2 days before until 2 days after the polluted days were compared to hospitalizations on clean air days of the same month.
Results:
Out of 1779 patients admitted due to pulmonary embolism, 1275 patients met our inclusion and exclusion criteria. Based on the results, 403 patients (31.6%) were hospitalized in clean and healthy air (air quality index [AQI] of 0-50 and 50-100), 816 patients (64.1%) were hospitalized in unhealthy air (AQI: 150-101), and 56 patients (4.4%) were hospitalized in days with polluted air (AQI:151-200). According to Pearson’s correlation coefficient, there was a significant relationship between carbon monoxide (r=0.09, P=0.0001), sulfur dioxide (r=0.11, P=0.001), PM10 (r=0.28, P=0.001), and PM2.5 (r=0.45, P=0.0001) concentrations and the frequency of hospitalizations due to pulmonary embolism.
Conclusions:
There is a positive and significant relationship between air pollutants and the number of hospitalizations due to pulmonary embolism. Hence, preventive measures should be taken into account regarding the air pollution at the provincial and national levels.
Keywords: Pulmonary embolism, Carbon monoxide, Sulfur dioxide, Nitrogen dioxide
Copyright and License Information
© 2024 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
None.
Please cite this article as follows: Soleimany A, Ghanbari Kaljahi S, Hajizadeh R. The relationship between air pollution components and hospitalizations due to acute pulmonary embolism. Int J Aging. 2024;2: e5. doi: 10.34172/ija.2024.e5
Introduction
Cardiovascular diseases (CVDs) are among the main causes of death and disability in most countries, including Iran.1 However, CVDs are among preventable non-communicable diseases.2,3 Pulmonary embolism causes cardiovascular death. It causes disability and emotional problems.
Deep vein thrombosis (DVT) is a condition in which a blood clot or thrombus forms in a deep vein (usually a lower limb). Symptoms of DVT are pain, tenderness, and swelling in the affected area, which should be diagnosed and treated immediately. DVT can also be life-threatening.
DVT can dislodge and migrate to the lungs, causing pulmonary embolism which could initiate cardiopulmonary collapse and death. On the other hand, it could result in chronic complications such as post-thrombotic syndrome and chronic thrombotic pulmonary hypertension.4
In the United States, it is estimated that there are 100 000 to 180 000 deaths due to pulmonary embolism annually, and it is also stated that pulmonary embolism is the most common preventable cause of death in hospitalized patients.5
In the United Kingdom in 2012, 2300 deaths from pulmonary embolism were reported, accounting for about 0.4% of deaths.6 In a study conducted in Canada, almost half of patients with pulmonary embolism after one year of diagnosis had exercise limitations, reduced walking distance, or shortness of breath, resulting in reduced quality of life.
According to the report of the World Health Organization, about 7 million people die every year due to diseases attributed to air pollution. There are more than 180 types of air pollutants, which exist in different forms such as solid particles, liquid droplets, or gas. These pollutants are divided into two main groups, primary and secondary subtypes.
Primary pollutants are those that originate directly from pollution sources, including carbon monoxide, sulfur dioxide, nitrogen oxides, hydrocarbons, and suspended particles with a diameter of less than 10 μm (PM10). Secondary pollutants are produced as a result of the interaction between different factors such as the environment (sunlight and humidity), including ozone pollutants, aldehydes, sulfuric acid, and peroxyacetyl nitrate. Air pollution in cities usually includes both primary and secondary pollutants.7
Previous studies have reported that for every microgram per cubic meter increase in PM10, the daily mortality of CVD increases by 0.69%, and the frequency of hospitalization due to heart failure increases by 0.8%.8 The main sources of these particles are cars and industries.9
Endothelial dysfunction is associated with increased levels of pollutants and has an association with various inflammatory and coagulation factors.10
Other risk factors for venous thromboembolism (VTE) include age, hereditary thrombophilia, surgery, cancer, and other co-morbidities. VTE is more common among women. An important risk factor is exposure to fine particles or particulate matter (PM), for example, PM10, PM25, and PM0.1. Epidemiological studies have supported this relationship, although the extent and the mechanisms of interactions are not understood yet. 11
In the study conducted by Spiezia et al, short-term exposure (for example, one month) to air pollutants was mentioned as a possible risk factor for pulmonary embolism.12 A prospective cohort study by Kan et al in 2010 investigated the association between long-term exposure to traffic-related air pollution and the incidence of VTE. In this study, a total of 13143 middle-aged men and women who were at risk of arteriosclerosis and had no history of DVT or pulmonary embolism were included. Traffic and distance to main roads were evaluated as indicators of exposure to pollutants, and the incidence of VTE by adjusted relative risk models was evaluated. The results of this project showed that there was no significant relationship between traffic pollution and VTE.13
As we know the level of traffic congestion is not the same in different countries and also among different cities of the same country, and the temperature and concentration of different pollutants and their interaction differ in different areas. This concept could make our results unique. Considering the increasing hospitalization rate of patients due to CVDs, the increasing trend of urbanization and exposure to air pollution, and the lack of studies in this field in our country, this descriptive and analytical study was conducted to determine the relationship between air pollution and pulmonary embolism.
Methods
In this cross-sectional study, according to the daily report from the meteorology center of West Azarbaijan province, the data on the concentrations of air pollutants, including PM10, NO2, O3, CO, and PM2.5, between 2016 and 2022 were extracted. Additionally, the files of patients without underlying risk factors hospitalized due to pulmonary embolism were extracted. Finally, admissions from 2 days before until 2 days after the polluted days were compared to hospitalizations on clean air days of the same month.
Participants
All patients over 18 years old, with a definite pulmonary embolism diagnosed by computed tomography (CT) angiography were included in this study. Patients with a previous history of recurrent pulmonary embolism or deep vein thrombosis, any malignancy, and recent surgery were excluded from the study.
Data Collection
According to meteorology center reports, the air quality index (AQI) was analyzed. This index reports the levels of air pollution caused by various pollutants. It was divided into clean (AQI = 0-100), unhealthy (AQI = 101-150), and polluted (AQI = 150-200).
The concentrations of air pollutants, including PM10, NO2, O3, CO, and PM2.5 were used to define good weather (clean) and bad weather (unhealthy and polluted).
These two groups of patients were matched according to co-morbidities, age, and gender. All patients who met the inclusion and exclusion criteria between 2016 and 2022 were included in this study
Data Analysis
For descriptive variables, frequency tables and mean ( ± SD) were used. Pearson’s correlation coefficient and Spearman’s correlation coefficients were used for normally and non-normally distributed data. Data analysis was done using SPSS version 21.0, and a P value of less than 0.05 was considered statistically significant.
Results
This cross-sectional analytical study was conducted between 2016 and 2022. Out of 1779 patients admitted due to pulmonary embolism, 1275 patients met our inclusion and exclusion criteria and were included in the study. The mean age of patients was 64.04 ± 16.75, and 51.8% of patients were male.
During the study, 82 polluted days were recorded. In 27 days (32.9%), the AQI value was 101-150, in 40 days (48.8%), it was 151-200, and in 15 days (18.3%), it was 200-300. Figure 1 shows the distribution of AQI values in different years.
The information on the frequency of hospitalization at different AQI values is shown in Table 1.
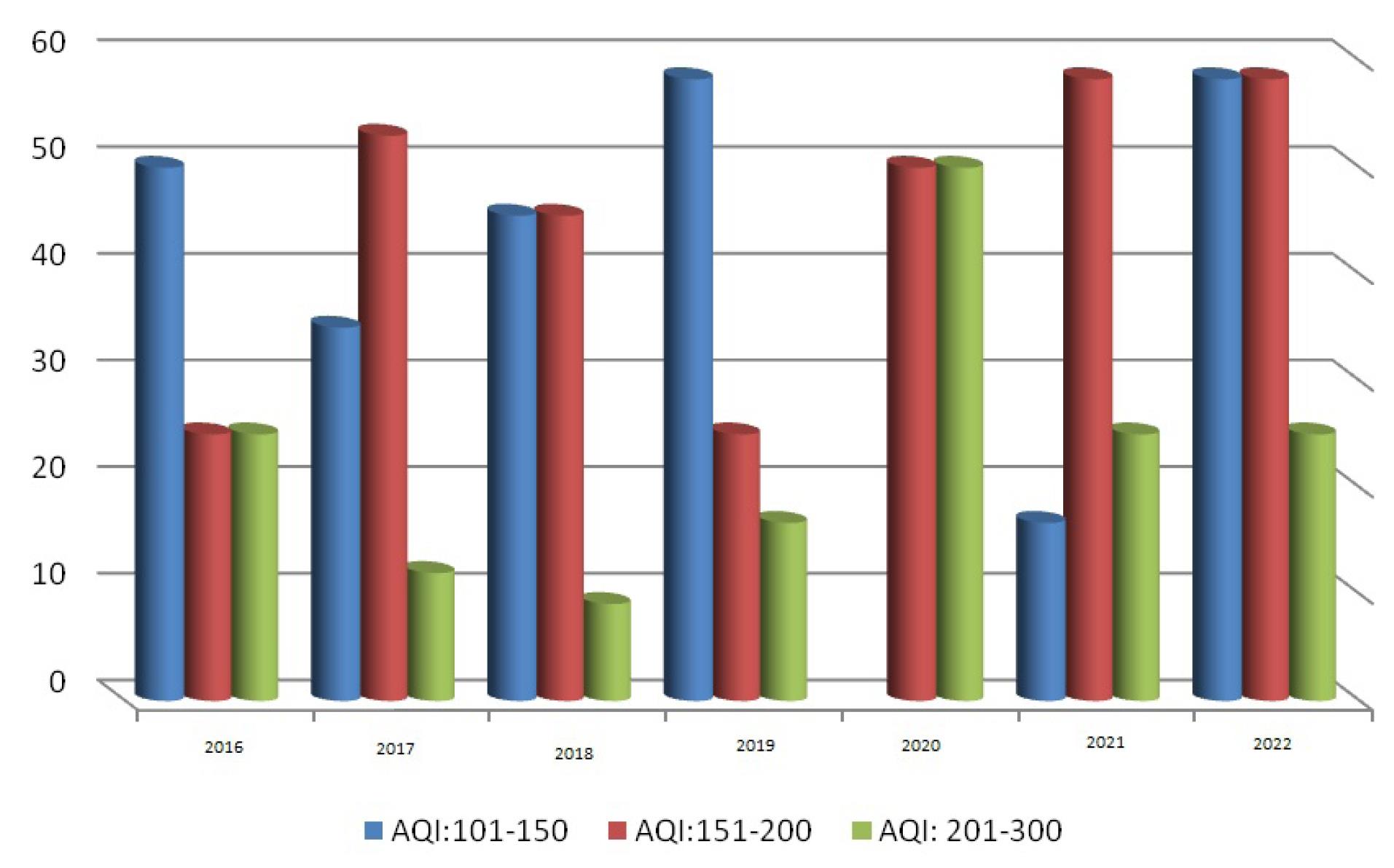
Figure 1.
Distribution of the air quality index (AQI) values in different years
.
Distribution of the air quality index (AQI) values in different years
Table 1.
The frequency of hospitalization at different air quality index values
|
Air quality index
|
Number of admissions
|
Percent
|
| Clean (0-50) and (50-100) |
403 |
34.6 |
| Unhealthy (101-150) |
816 |
64.1 |
| Polluted (150-200) |
56 |
4.4 |
| Total |
1275 |
100 |
According to Pearson’s correlation coefficient, there is a significant relationship between the concentration of carbon monoxide and the frequency of hospitalizations due to pulmonary embolism (r = 0.09, P = 0.0001) (Figure 2).
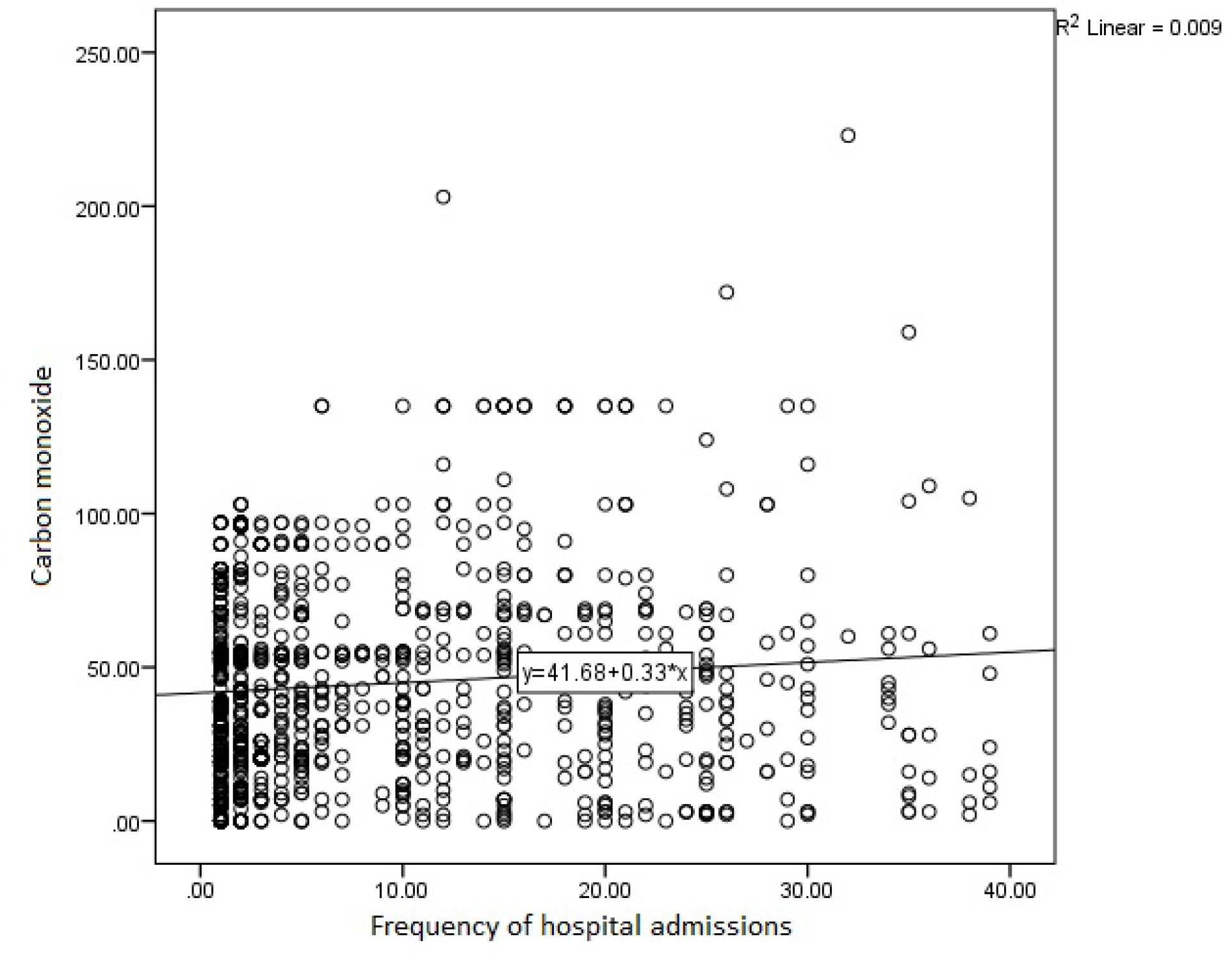
Figure 2.
Correlation Between Carbon Monoxide Concentration and Frequency of Hospitalization Due to Pulmonary Embolism
.
Correlation Between Carbon Monoxide Concentration and Frequency of Hospitalization Due to Pulmonary Embolism
Pearson’s correlation coefficient showed a significant relationship between sulfur dioxide concentration and the frequency of hospitalization due to pulmonary embolism (r = 0.11, P = 0.001) (Figure 3).
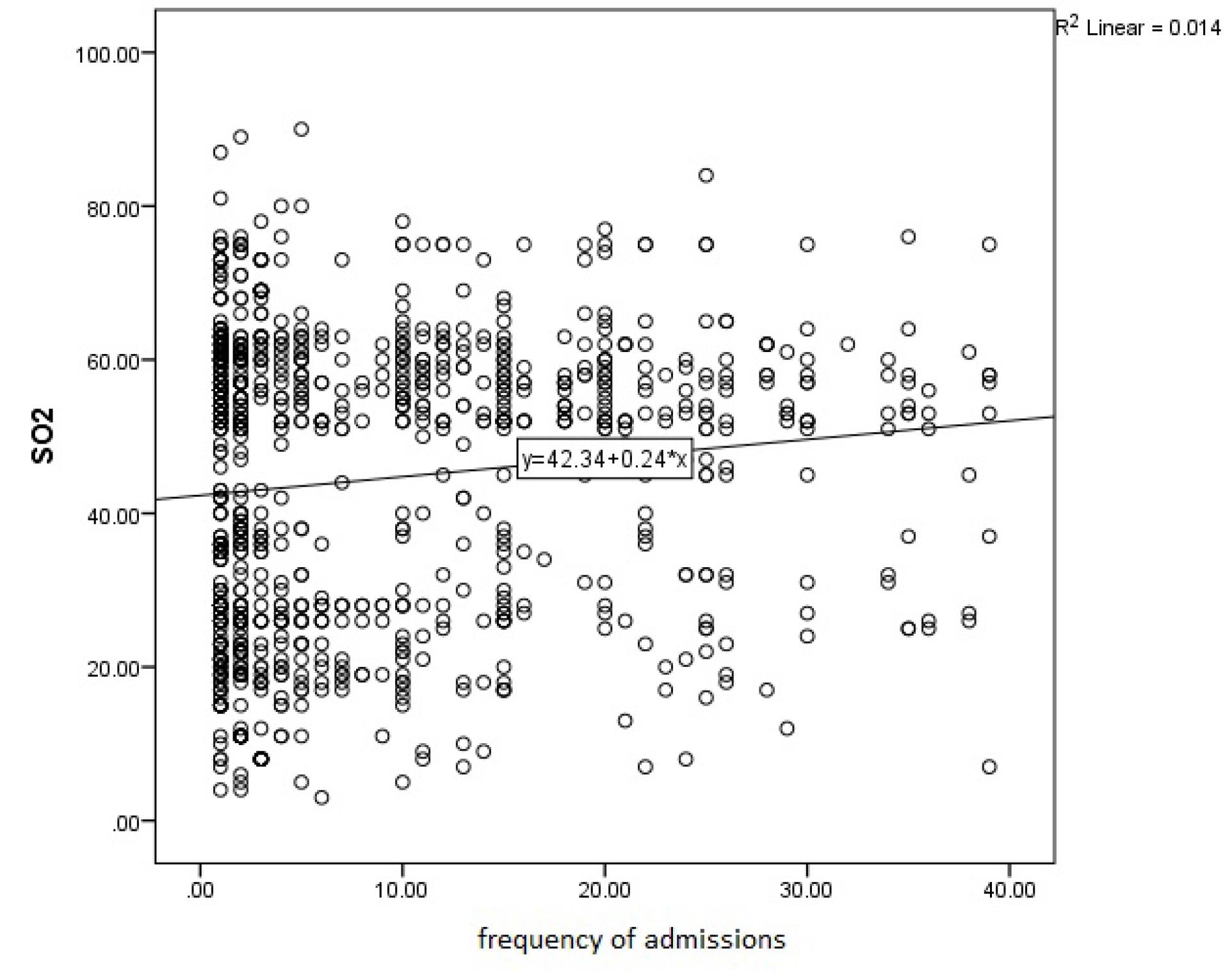
Figure 3.
Correlation Between Sulfur Dioxide Concentration and the Frequency of Hospitalization
.
Correlation Between Sulfur Dioxide Concentration and the Frequency of Hospitalization
Our results also showed a significant relationship between PM10 concentration and the frequency of hospitalization due to pulmonary embolism (r = 0.28, P = 0.001) (Figure 4).
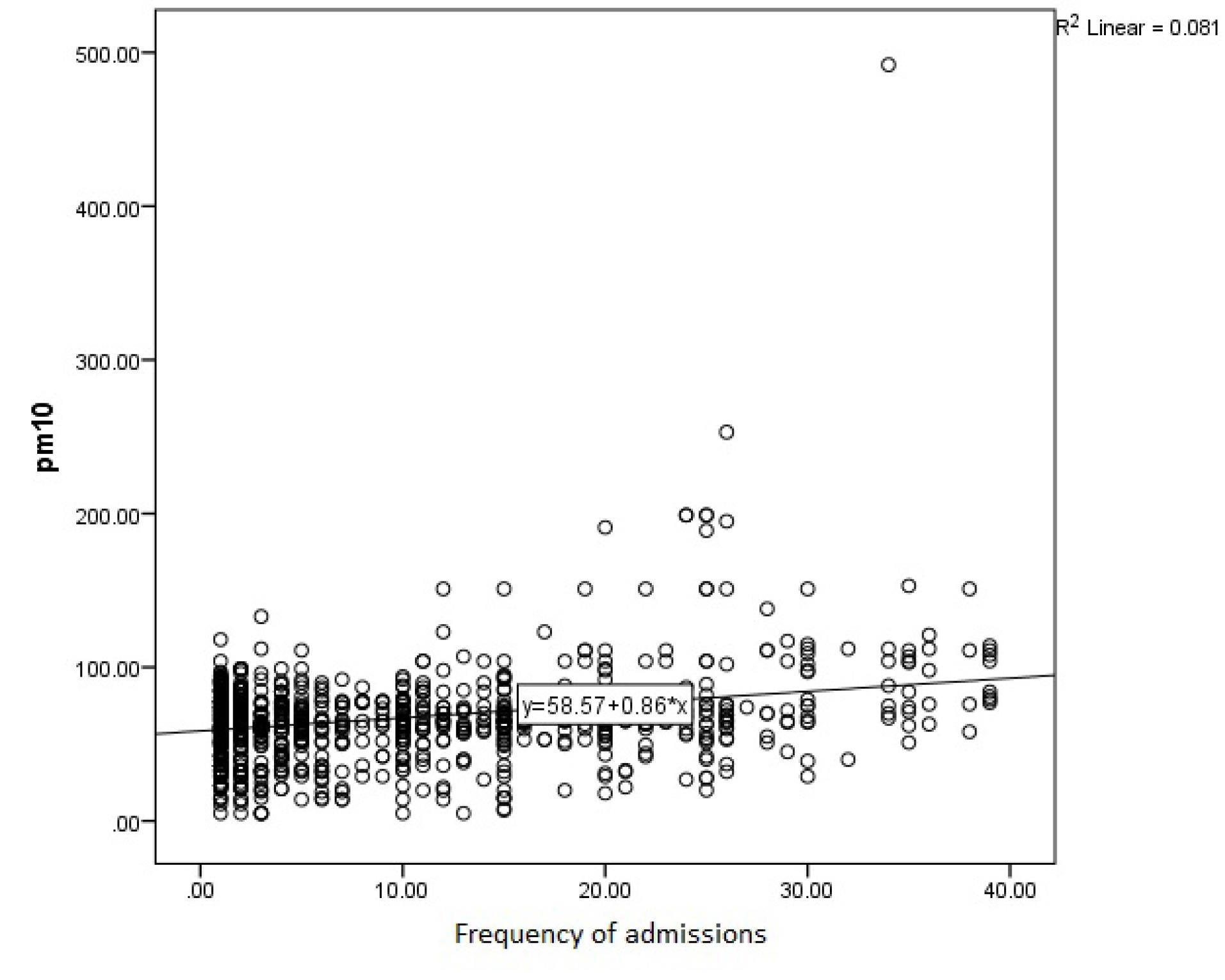
Figure 4.
Correlation Between PM10 Concentration and the Frequency of Hospitalization
.
Correlation Between PM10 Concentration and the Frequency of Hospitalization
According to Pearson’s correlation coefficient, there was a significant relationship between PM2.5 concentration and the frequency of hospitalization due to pulmonary embolism (r = 0.45, P = 0.0001) (Figure 5).
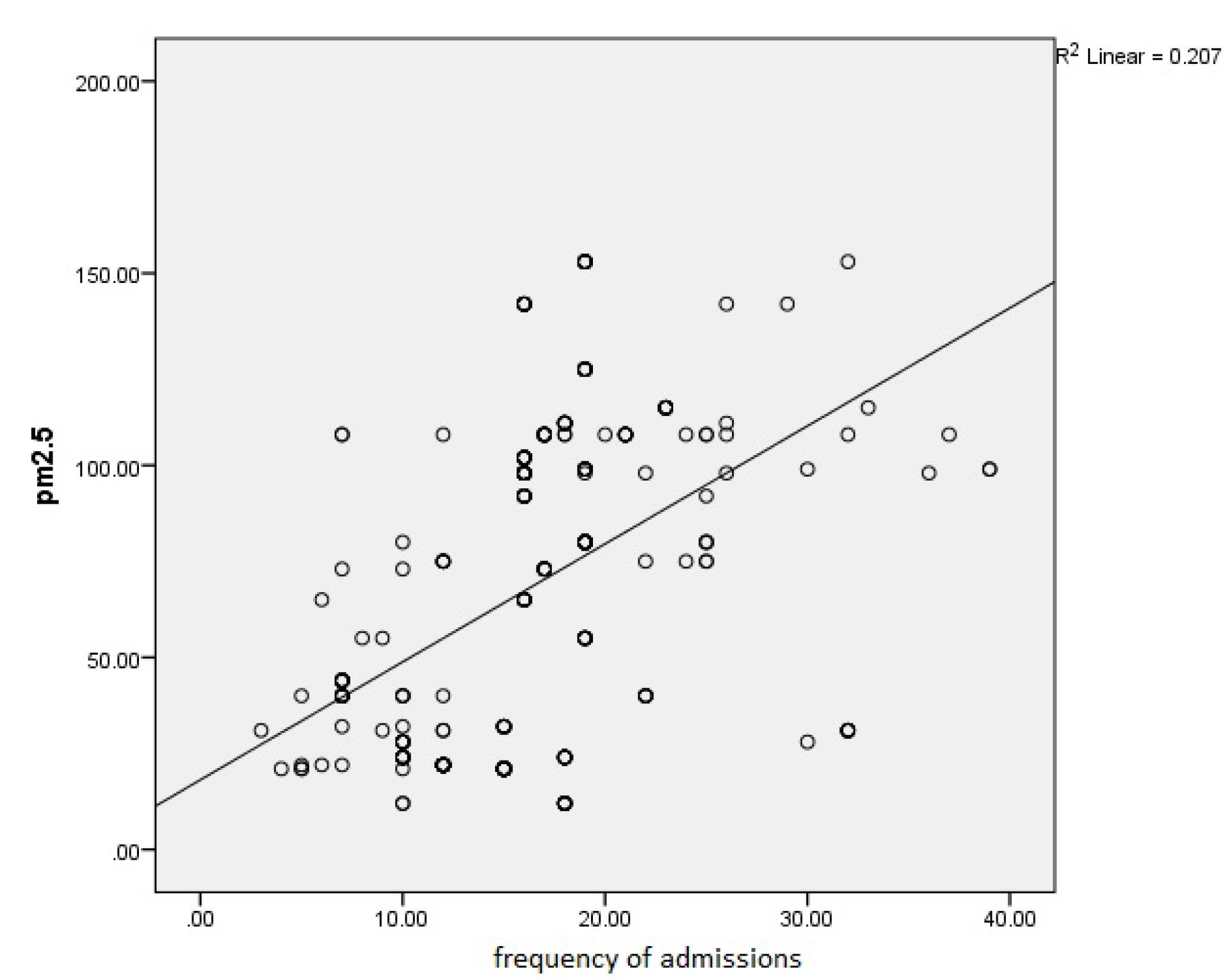
Figure 5.
Correlation Between PM2.5 Concentration and the Frequency of Hospitalization
.
Correlation Between PM2.5 Concentration and the Frequency of Hospitalization
Discussion
Considering the increasing hospitalization rate of patients due to CVDs, the increasing trend of urbanization and air pollution, and insufficient data in this field, this descriptive-analytical study was conducted to investigate the relationship between air pollution and pulmonary embolism in northwest of Iran.
Our study showed that hospitalizations of patients on days with a high air pollution index increased by 32.5% compared to clean days. Kloog et al showed that exposure to PM2.5 was associated with an increased risk of hospitalizations due to DVT and pulmonary embolism, which is in line with our results.14
The results of our study showed that there is a significant relationship between the concentration of carbon monoxide, sulfur dioxide, No2, and PM10 with the frequency of hospitalizations due to pulmonary embolism.
These findings are in line with the results of the study conducted by Spiezia et al. The results of his study showed that people who were exposed to PM10, NOx, benzene, benzopyrene, cadmium, and lead showed a significant increase in the risk of sudden pulmonary embolism. The odds ratio (OR) for exposure to PM10 per month before the diagnosis of pulmonary embolism was 5.24 (18.12-1.52, 95% CI), and for exposure to benzopyrene, it was reported to be 3.95 (14.71-1.6, 95% CI). Therefore, short-term exposure to air pollutants can be regarded as a risk factor for pulmonary embolism.12
Recent studies have linked endothelial damage, arterial vessel constriction, changes in blood coagulation factors, and activation of inflammation to exposure to air pollution, and the production of reactive oxygen species.15,16
Venous thromboembolism is the third most common CVD after acute coronary syndrome and stroke.17 Recent studies have shown that there is an association between arterial thromboembolism and common risk factors such as age, obesity, diabetes mellitus, hyperlipidemia, and exposure to air pollution.18
Available limited evidence suggests that exposure to air pollution can contribute to pulmonary and systemic inflammation and blood coagulation. Additionally, an epidemiological association between air pollution and both arterial thromboembolism and VTE has been reported in recent studies. Two retrospective case-control studies investigating the long-term effects of air pollution estimated a 70% increased risk of DVT for every 10 μg/m3 increase in PM10 during the year before diagnosis.19
Colais et al evaluated the short-term effects of air pollution and showed that there was a strong relationship between pulmonary embolism and NO2, which is similar to our results.20
On the contrary, two large prospective studies conducted in the United States found no evidence of any association between the risk of acute or chronic VTE and exposure to air pollution (assessed by PM10 concentration and traffic overload).13,21
Systemic inflammation, oxidative stress, and vascular dysfunction are possible etiologies causing pulmonary embolism and deep vein thrombosis in unhealthy air conditions.22
Limitations
Our study is based on the concentrations of air pollutants and the duration of exposure to these pollutants was not evaluated in this study. Further evaluations in urban and rural areas especially on those who live in clean areas traveling to polluted areas for short periods could help to get better insights.
Conclusions
According to the results of our study, there is a positive and significant relationship between air pollutants and the number of hospitalizations due to pulmonary embolism. Hence, preventive measures should be taken into account regarding the air pollution at the provincial and national levels.
Author contributions
Conceptualization: Ali Soleimany
Data curation: Saeed Ghanbari Kaljahi.
Formal analysis: Reza Hajizadeh.
Investigation: Ali Soleimany.
Methodology: Reza Hajizadeh.
Project administration: Ali Soleimany.
Resources: Saeed Ghanbari Kaljahi.
Software: Ali Soleimany, Reza Hajizadeh.
Supervision: Ali Soleimany.
Validation: Ali Soleimany.
Visualization: Ali Soleimany, Saeed Ghanbari Kaljahi, Reza Hajizadeh.
Writing-original draft: Reza Hajizadeh.
Writing-reviewing & editing: Reza Hajizadeh.
Data availability statement
All data generated or analyzed during the study are included in this published article.
Ethical approval
This study was approved by the Ethics Committee of Urmia University of Medical Sciences (IR.UMSU.REC.1399.119).
Consent for publication
Not Applicable.
Conflict of interests
The authors declare that there is no conflict of interests.
References
- Beyranvand MR, Manhoobi H, Shahraz S, Kolahi AA. Myocardial infarction in Iran: epidemiology, management, and prognosis. J Tehran Heart Cent 2023; 18(2):82-6. doi: 10.18502/jthc.v18i2.13316 [Crossref] [ Google Scholar]
- Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB. Executive summary: heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation 2013; 127(1):143-52. doi: 10.1161/CIR.0b013e318282ab8f [Crossref] [ Google Scholar]
- Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB. Executive summary: heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation 2012; 125(1):188-97. doi: 10.1161/CIR.0b013e3182456d46 [Crossref] [ Google Scholar]
- Hong J, Lee JH, Lee JY, Lee JO, Choi WI, Ahn S. Prominent seasonal variation in pulmonary embolism than deep vein thrombosis incidence: a Korean venous thrombosis epidemiology study. Korean J Intern Med 2020; 35(3):682-91. doi: 10.3904/kjim.2018.370 [Crossref] [ Google Scholar]
- Di Nisio M, van Es N, Büller HR. Deep vein thrombosis and pulmonary embolism. Lancet 2016; 388(10063):3060-73. doi: 10.1016/s0140-6736(16)30514-1 [Crossref] [ Google Scholar]
- Doherty S. Pulmonary embolism an update. Aust Fam Physician 2017; 46(11):816-20. [ Google Scholar]
- Chardon B, Host S, Pedrono G, Gremy I. [Contribution of case-crossover design to the analysis of short-term health effects of air pollution: reanalysis of air pollution and health data]. Rev Epidemiol Sante Publique 2008; 56(1):31-40. doi: 10.1016/j.respe.2007.11.002.[French] [Crossref] [ Google Scholar]
- Morris RD. Airborne particulates and hospital admissions for cardiovascular disease: a quantitative review of the evidence. Environ Health Perspect 2001; 109(Suppl 4):495-500. doi: 10.1289/ehp.01109s4495 [Crossref] [ Google Scholar]
- Carlisle AJ, Sharp NC. Exercise and outdoor ambient air pollution. Br J Sports Med 2001; 35(4):214-22. doi: 10.1136/bjsm.35.4.214 [Crossref] [ Google Scholar]
- Risom L, Møller P, Loft S. Oxidative stress-induced DNA damage by particulate air pollution. Mutat Res 2005; 592(1-2):119-37. doi: 10.1016/j.mrfmmm.2005.06.012 [Crossref] [ Google Scholar]
- Signorelli SS, Ferrante M, Gaudio A, Fiore V. Deep vein thrombosis related to environment (review). Mol Med Rep 2017; 15(5):3445-8. doi: 10.3892/mmr.2017.6395 [Crossref] [ Google Scholar]
- Spiezia L, Campello E, Bon M, Maggiolo S, Pelizzaro E, Simioni P. Short-term exposure to high levels of air pollution as a risk factor for acute isolated pulmonary embolism. Thromb Res 2014; 134(2):259-63. doi: 10.1016/j.thromres.2014.05.011 [Crossref] [ Google Scholar]
- Kan H, Folsom AR, Cushman M, Rose KM, Rosamond WD, Liao D. Traffic exposure and incident venous thromboembolism in the Atherosclerosis Risk in Communities (ARIC) Study. J Thromb Haemost 2011; 9(4):672-8. doi: 10.1111/j.1538-7836.2011.04210.x [Crossref] [ Google Scholar]
- Kloog I, Zanobetti A, Nordio F, Coull BA, Baccarelli AA, Schwartz J. Effects of airborne fine particles (PM25) on deep vein thrombosis admissions in the northeastern United States. J Thromb Haemost 2015; 13(5):768-74. doi: 10.1111/jth.12873 [Crossref] [ Google Scholar]
- Donaldson K, Stone V, Seaton A, MacNee W. Ambient particle inhalation and the cardiovascular system: potential mechanisms. Environ Health Perspect 2001; 109(Suppl 4):523-7. doi: 10.1289/ehp.01109s4523 [Crossref] [ Google Scholar]
- Vermylen J, Nemmar A, Nemery B, Hoylaerts MF. Ambient air pollution and acute myocardial infarction. J Thromb Haemost 2005; 3(9):1955-61. doi: 10.1111/j.1538-7836.2005.01471.x [Crossref] [ Google Scholar]
- Giuntini C, Di Ricco G, Marini C, Melillo E, Palla A. Pulmonary embolism: epidemiology. Chest 1995; 107(1 Suppl):3S-9S. doi: 10.1378/chest.107.1_supplement.3s [Crossref] [ Google Scholar]
- Prandoni P, Bilora F, Marchiori A, Bernardi E, Petrobelli F, Lensing AW. An association between atherosclerosis and venous thrombosis. N Engl J Med 2003; 348(15):1435-41. doi: 10.1056/NEJMoa022157 [Crossref] [ Google Scholar]
- Pope CA 3rd. The expanding role of air pollution in cardiovascular disease: does air pollution contribute to risk of deep vein thrombosis?. Circulation 2009; 119(24):3050-2. doi: 10.1161/circulationaha.109.870279 [Crossref] [ Google Scholar]
- Colais P, Serinelli M, Faustini A, Stafoggia M, Randi G, Tessari R. [Air pollution and urgent hospital admissions in nine Italian cities Results of the EpiAir Project]. Epidemiol Prev 2009; 33(6 Suppl 1):77-94. [ Google Scholar]
- Milojevic A, Wilkinson P, Armstrong B, Bhaskaran K, Smeeth L, Hajat S. Short-term effects of air pollution on a range of cardiovascular events in England and Wales: case-crossover analysis of the MINAP database, hospital admissions and mortality. Heart 2014; 100(14):1093-8. doi: 10.1136/heartjnl-2013-304963 [Crossref] [ Google Scholar]
- Finch J, Conklin DJ. Air pollution-induced vascular dysfunction: potential role of endothelin-1 (ET-1) system. Cardiovasc Toxicol 2016; 16(3):260-75. doi: 10.1007/s12012-015-9334-y [Crossref] [ Google Scholar]