Int J Aging. 2023;1:e13.
doi: 10.34172/ija.2023.e13
Original Article
Studying the Affecting Factors in Patient Workflow and Outcome of Patients with Stroke Diagnosis in the Emergency Department
Masoumeh Poureskandari 1  , Elyar Sadeghi-Hokmabadi 2
, Elyar Sadeghi-Hokmabadi 2  , Alireza Ala 1
, Alireza Ala 1  , Kobra Tayyari 1, Samad Shams Vahdati 1, *
, Kobra Tayyari 1, Samad Shams Vahdati 1, * 
Author information:
1Emergency and Trauma Care Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
2Neurosciences Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Objectives:
To investigate the factors involved in the assignment and outcomes of patients with stroke referred to the Emergency Department of Imam Reza hospital in Tabriz in 2018.
Design:
A cross-sectional study.
Setting(s):
Imam Reza hospital, Tabriz, Iran.
Participants:
Patients over 60 years of age.
Outcome measures:
All patients were recorded for admission to discharge, admission to the first visit by the Emergency and Neurosurgery Department, admission to the patient assignment, and patient outcome. The intervals were then calculated from the baseline triage, and the intervals for which the patient was most likely to stay were reviewed and rooted.
Results:
There was a significant relationship between age, sex, type of stroke, outcome, and hyperlipidemia, but the correlation coefficient was weak. Further, there was a significant difference between triage to assignment and triage to emergency leave with a strong correlation, but there was a significant relationship with the type of stroke, and the correlation coefficient was weak. Moreover, there was a significant relationship between triage to emergency leave and the type of stroke, but the correlation coefficient was weak. Moreover, the relationship between the type of stroke and the outcome was significant with a weak correlation coefficient.
Conclusions:
One of the causes of delay in the workload of patients with stroke is the high time interval between requesting a neurologic visit to a neurological service visit. The duration of the assignment for stroke patients is less than 6 hours, but it takes more than 6 hours for the patient to leave the emergency room. There is a weak inverse relationship between the type of stroke, the duration of the assignment, and exit from the emergency, meaning that patients with hemorrhagic stroke are assigned with a delay and are discharged from the emergency room later.
Keywords: Workflow, Stroke, Disposition
Introduction
Time is an extremely important factor in the diagnosis and treatment of stroke patients and even affects the outcome of patients. Among the factors that could also affect physicians and medical staff in this context is a crowded emergency in which patients have been admitted.1 The emergency department is often referred to as the microstructure (miniature image) of the entire hospital. Almost everything that happens in the hospital daily also happens in the emergency department. The emergency is the main hospital door (hospital entrance). Visiting the largest volume of patients is one of the most vital areas and closest to the pulse of society.2
In 2011, Chatterjee et al in a study examined emergency congestion and its association with the duration of care for stroke patients. There was no significant relationship between the crowded emergency department and computerized tomography (CT) and thrombolysis. This study showed that emergency department crowding is not associated with delays in inpatient care. However, patients whose symptoms had started more than 3 hours before referral experienced longer waiting times for CT in the emergency crowding.3 In 2009, Bernstein et al conducted a study aimed at examining the impact of emergency crowding on the quality of services provided. This study indicated that the conditions of patients whose treatment is time-sensitive and those whose quality of service affects mortality are affected by emergency crowding.4 Causes of overcrowding in the emergency department can be attributed to a lack of access to inpatient facilities and beds, which may increase with a rise in the number of patients admitted but still awaiting to leave the emergency department to the wards (afterload).5,6 Emergency congestion in some cases may delay the identification and treatment of patients with diseases that require immediate attention, and delay in their treatment process can have long-term consequences.7 Therefore, in light of the above considerations, we decided to design a study to investigate the factors involved in the workflow of stroke patients and their outcomes referred to the emergency department in 2018.
Methods
Study Type
The present study was a cross-sectional study.
Study Design
This study was conducted in the Emergency Department of Imam Reza hospital in 2018. In this observational, descriptive, cross-sectional study, 100 days were selected using a randomized computer program (Random Allocation software), and eight days of each month were randomly selected. All patients who were suspected of having an acute stroke, with informed consent from the patient if possible, otherwise from the patient legal guardian were included. Patients who did not have a stroke or comorbidity with acute stroke or who left the hospital before treatment and confirming the diagnosis were excluded. The duration of admission to discharge and duration of admission to the first visit by emergency medicine and neurology services were recorded for all patients to determine patient disposition and patient outcomes. Then, the intervals were calculated from the baseline triage, and the intervals for which the patient was most likely to stay were reviewed and analyzed.
Statistical Analysis
The obtained data were entered into IBM SPSS statistics software Version 24 and analyzed with a significance level under 0.05. In the descriptive section, frequency (percent) was used for qualitative variables, and quantitative variables were used to summarize information using the mean (standard deviation) if their distribution was normal and using median quadratic in the absence of normal distribution.
Results
General Information
In this study, 226 individuals were selected based on inclusion criteria in 100 days. Despite the absence of a normal distribution, the mean age was 72.42 ± 11.58 (confidence interval 95%,70.90-73.94), and due to the multiple modes, the smallest mode was 60 years, and the median was 73 years. In this study, 121 (53.5%) were male, and 105 (46.5%) were female.
The time between patient triage to patient admission and patient specification in the hospital admission system was 8.21 ± 6.97 (1-51 minutes) minutes with a median of 6 minutes and a mode of 4 minutes. Moreover, the interval between patient triage and the first visit by emergency medicine was 22.02 ± 16. 01 (1-130) with a median and mode of 18 and 15 minutes, respectively. Furthermore, the time between patient triage to neurologic service visit request was 74.70 ± 67.92 (0-368) minutes, with a median of 50 minutes and a mode of 30 minutes. The time between the triage of the patient and the first visit by the neurologist was 164.81 ± 112.56 (0-665) minutes, with a median of 135 minutes and a mode of 60 minutes. In addition, the time between patient triage to brain CT scan was 86.86 ± 91.60 (0-841) minutes, with a median of 60 minutes and a mode of 50 minutes. Further, the time between patient triage to the patient assignment was 301.68 ± 238.91 (33-1395) minutes with a median of 235 minutes and a mode of 140 minutes. The time between patient triage and patient exit from the emergency department was 422.37 ± 354.23 (2-1754) minutes, with a median of 287 minutes and a mode of 155 minutes.
Of 226 patients, 38 had a hemorrhagic stroke, and 188 had an ischemic stroke. Patient length of stay in the hospital was 8.53 ± 7.54 (1-42) days, with a median of 6 days and a mean of 3 days. Of these patients, 98 were admitted to the neurological ward and 78 to the clitoral ward (Figure 1).
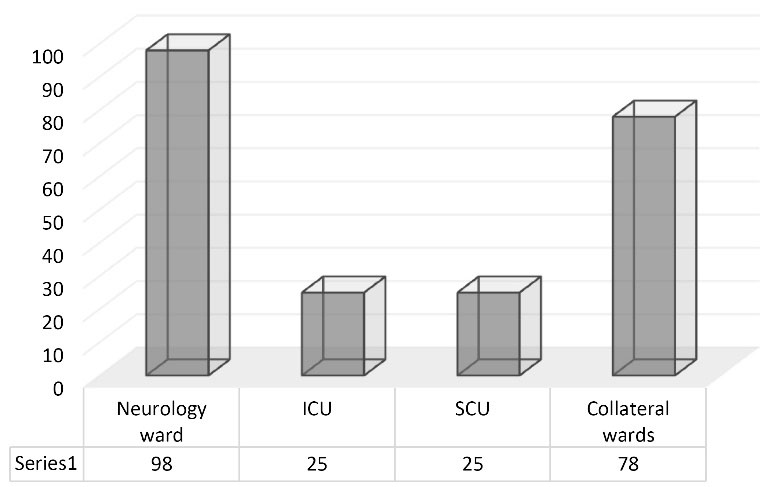
Figure 1.
The Frequency of Patients with Stroke Admitted to the Hospital
.
The Frequency of Patients with Stroke Admitted to the Hospital
Nine patients had a history of smoking, 69 had a history of diabetes mellitus, 16 patients had hyperlipidemia, 60 had a history of cerebrovascular disease, 54 had ischemic heart disease, and 162 patients had a history of hypertension.
The patient’s symptoms during the visit are presented in Figure 2.
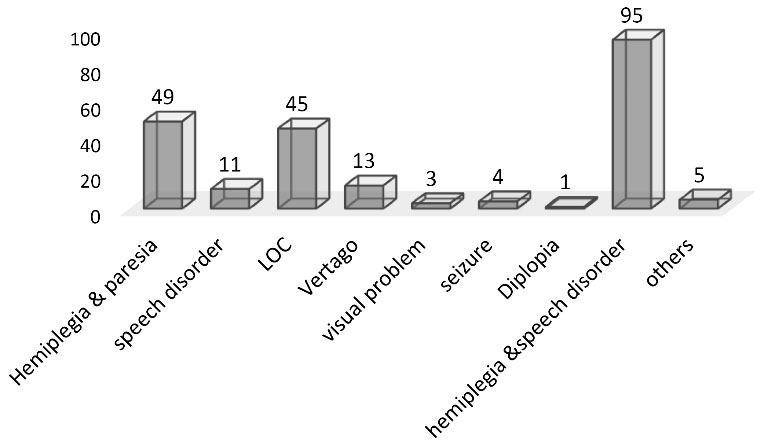
Figure 2.
The Prevalence of Symptoms Suggestive of Stroke in Patients
.
The Prevalence of Symptoms Suggestive of Stroke in Patients
There was a significant relationship between age, sex, type of stroke, outcome, and hyperlipidemia, but the correlation coefficient was weak (P < 0.05, Pearson correlation ≤ 0.30). There was a significant relationship between gender and outcome, smoking risk factors, diabetes, ischemic heart disease, and hypertension, but the correlation coefficient was weak (P < 0.05; Pearson correlation = 0.30). There was also a significant relationship between triage to emergency room admission and triage to first emergency medicine visit and neuroscience request, but the correlation coefficient was low (P < 0.05, Pearson correlation ≤ 0.30). Moreover, there was a significant correlation between triage to first emergency medicine visit and triage to neurology visit, triage to brain CT scan, triage to assignment, outcome, and risk factor, but the correlation coefficient was weak (P < 0.05, Pearson correlation ≤ 0.30).
There was a significant relationship between triage to neurological visit request and triage to first neurological visit (P < 0.05; Pearson correlation ≤ 0.80), but the correlation was moderate. There was a significant relationship between triage to CT scan, triage to assignment, and triage to emergency leave, but the correlation coefficient was low (P < 0.05; Pierson correlation ≤ 0.30). However, there was a significant difference between the triage to the first neurological visit and triage to CT scan, triage to assignment, and triage to emergency leave (P < 0.05; Pearson correlation ≤ 0.80). There was also a significant relationship with stroke type but with a weak correlation coefficient (P < 0.05; Pearson correlation ≤ 0.30). In addition, there was a significant relationship between triage and CT scan and triage to assignment and triage to emergency leave, but the correlation coefficient was poor (P < 0.05; Pearson correlation ≤ 0.30). There was a significant difference between triage to task assignment and triage to emergency leave (P < 0.05; Pearson correlation ≤ 0.80).
However, there was a significant relationship with the type of stroke, but the correlation coefficient was weak (P < 0.05, Pearson correlation ≤ 0.30). There was also a significant relationship between triage to emergency leave and the type of stroke, but the correlation coefficient was weak (P < 0.05, Pearson correlation ≤ 0.30). Moreover, there was a significant relationship between the type of stroke and outcome, but the correlation coefficient was weak, and there was a significant relationship between diabetes risk factors and blood pressure, but the correlation coefficient was weak (P < 0.05, Pearson correlation = 0.30). Furthermore, there was a significant relationship between the duration of hospital stay and outcome but a weak inverse correlation. There was also a significant relationship between the smoking risk factor and blood pressure, but the correlation coefficient was weak (P < 0.05, Pearson correlation = 0.30).
Discussion
In 2015, a regular review was published which identified three key factors related to the quality of patient care, including the number of patients waiting to be triaged, the emergency department emergency rate, and the number of patients waiting to be admitted to the ward. However, this study did not find a significant relationship between emergency department crowding and the quality of care for stroke patients.8 Jungehulsing et al in another study also evaluated the factors affecting the care of patients with acute stroke. Their study showed that admissions in two specific cases, including the weekends and having private insurance and private healthcare facilities were less delayed.9 In 2015, Ben-Yakov et al found no significant relationship between emergency department crowding and transient ischemic attacks and minor strokes.10 However, in our study, although there was a significant difference between the time of triage of stroke patients and the first visit by the emergency medical service, neurology service visit, CT scan of the brain, assignment of patients, and patient outcome, the relationship was weak, and this weak statistical relationship in the clinical setting could not be considered a significant relationship.
In support of the results of this study, a study conducted by Chen et al in 2006 demonstrated that the concurrent trauma assessment in the emergency room leads to more emergency workloads and delayed CT preparation of patients with suspected stroke.11 According to the present study, the waiting time of stroke patients for brain CT was more than one hour, which can be reduced with management plans. In the present study, the type of stroke was strongly correlated with the time of assigning patients, and patients with ischemic stroke were assigned earlier, but there was no obvious clinical connection regarding the outcome or length of hospitalization of patients.
Another study showed that the groups are not correlated across conditions (demographics and risk factors). However, we did not find any evidence to modulate the effects of individual illnesses during residency after multivariate logistic regression analysis. The adjustment of individual factors suggests that the benefits observed in stroke care during the stay are more significant in ischemic stroke patients than in hemorrhagic stroke patients and are independent of age, gender, and associated conditions. Moreover, more patients were generally admitted to the stroke ward compared to the general/general ward. Neurologic hospitalization has been attributed to a 4-day decrease in length of stay, which may increase the care capacity of patients in the neurological ward.12 In the current study, demographic factors such as age, sex, and risk factors were not significantly associated with length of hospital stay, type of stroke, patient assignment, and patient exit from the emergency room. Additionally, this study showed that hospital admission has no significant effect on patient outcomes.
Field et al reported that hospital mortality due to stroke of all types (e.g., ischemic, hemorrhagic) decreases with admission to the stroke center, and readmission for recurrent stroke after transient ischaemic attack decreased by approximately 50%.13 They consistently observed a significant decrease in mortality in their study. This indicates that the management of stroke patients in a stroke unit is associated with a continuous decrease in the length of stay compared to general/clerical units, whereas the present study did not show a significant association with patient mortality.
From the economic point of view of the hospital, a shorter hospital stay in a stroke unit is promising in the present study. The main costs of care are related to the cost of a hospital bed per day. Another study from the Canadian Stroke Unit found that a 2-day reduction in the length of stay of each patient in the stroke unit saves more than 2.1 million dollars per 1000 treated patients. With a 4-day reduction in the length of stay, this estimate doubles. With $1200 per night in hospitals and 1000 patients per year, stroke unit care has resulted in $24 million in savings over 5 years.14 Despite the Brain Attack Coalition’s15 consensus statement and several national institutions in Europe,16 the US,17 and Canada14 recommend that stroke care be widely practiced, structured stroke care is not yet widespread in Canada,18 but it is changing with the development of stroke strategies. The economic analysis should be done according to the complete chain of care not just the length of hospital stay. The present study also showed no significant difference between patients in the stroke center and patients admitted to other wards, even the neuroscience ward, and the neuroscience itself, and patients’ outcomes did not exhibit a significant relationship with hospitalization.
In their study on the evaluation of eligibility for intravenous thrombolytic therapy in acute ischemic stroke patients, Ayromlou et al found that the main obstacle in the treatment of ischemic stroke patients with thrombolytics is the delay in providing in-hospital services such as initial patient assessment, CT scan, or laboratory findings, so it can be concluded that these cases also affect the workflow of stroke patients in the hospital.19 In stroke rehabilitation, Soleimanpour’s study suggested that bilirubin can have an inhibitory effect on nerve damage caused by ischemia and may be a potential treatment method for ischemic stroke, and since it has neuroprotective effects on stroke, it can affect the incidence and prognosis of ischemic stroke.20
Conclusions
According to the study, one of the causes of delay in the workload of patients with stroke is a considerably long interval between the first visit to the emergency room and a CT scan, which is an average of 60 minutes. Further, the assignment time for stroke patients is less than 6 hours, which complies with the criteria of the Ministry of Health and Medical Education, but it takes more than 6 hours for the patient to leave the emergency room. According to this study, a relatively significant percentage of patients were admitted to the collateral ward, which requires either the expansion of the neurology ward or building new wards. However, there is a weak inverse relationship between the type of stroke and the duration of assignment and discharge from the emergency room, that is, patients with hemorrhagic stroke are assigned with a delay and are discharged from the emergency room later. There is a strong correlation between triage to assignment and patient exit from the emergency room, meaning patients who are assigned later are often discharged from the emergency room later, which appears to be the same patients with hemorrhagic stroke.
Acknowledgments
Special thanks to Dr. Mehdi Farhoudi who helped us access the data of stroke patients in the stroke registry. All data were gathered from the stroke registry of the neurosciences research center of Tabriz University of medical sciences.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Not applicable.
Ethical approval
This study was approved by the Research Committee of the Faculty of Medical Sciences, Tabriz University of Medical Sciences with the ethical approval code: IR.TBZMED.REC.1397.924.
Consent for publication
Not applicable.
Conflict of interests
The author(s) declare no potential conflict of interests with respect to the research, authorship, and/or publication of this study.
References
- Mohseni M, Alikhani M, Tourani S, Azami-Aghdash S, Royani S, Moradi-Joo M. Rate and causes of discharge against medical advice in Iranian hospitals: a systematic review and meta-analysis. Iran J Public Health 2015; 44(7):902-12. [ Google Scholar]
- Derlet RW, McNamara RM, Kazzi AA, Richards JR. Emergency department crowding and loss of medical licensure: a new risk of patient care in hallways. West J Emerg Med 2014; 15(2):137-41. doi: 10.5811/westjem.2013.11.18645 [Crossref] [ Google Scholar]
- Chatterjee P, Cucchiara BL, Lazarciuc N, Shofer FS, Pines JM. Emergency department crowding and time to care in patients with acute stroke. Stroke 2011; 42(4):1074-80. doi: 10.1161/strokeaha.110.586610 [Crossref] [ Google Scholar]
- Bernstein SL, Aronsky D, Duseja R, Epstein S, Handel D, Hwang U. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med 2009; 16(1):1-10. doi: 10.1111/j.1553-2712.2008.00295.x [Crossref] [ Google Scholar]
- Derlet RW, Richards JR. Ten solutions for emergency department crowding. West J Emerg Med 2008; 9(1):24-7. [ Google Scholar]
- Barish RA, McGauly PL, Arnold TC. Emergency room crowding: a marker of hospital health. Trans Am Clin Climatol Assoc 2012; 123:304-10. [ Google Scholar]
- Hoot NR, Epstein SK, Allen TL, Jones SS, Baumlin KM, Chawla N, et al. Forecasting emergency department crowding: an external, multicenter evaluation. Ann Emerg Med 2009;54(4):514-22.e19. 10.1016/j.annemergmed.2009.06.006.
- Stang AS, Crotts J, Johnson DW, Hartling L, Guttmann A. Crowding measures associated with the quality of emergency department care: a systematic review. Acad Emerg Med 2015; 22(6):643-56. doi: 10.1111/acem.12682 [Crossref] [ Google Scholar]
- Jungehulsing GJ, Rossnagel K, Nolte CH, Muller-Nordhorn J, Roll S, Klein M. Emergency department delays in acute stroke - analysis of time between ED arrival and imaging. Eur J Neurol 2006; 13(3):225-32. doi: 10.1111/j.1468-1331.2006.01170.x [Crossref] [ Google Scholar]
- Ben-Yakov M, Kapral MK, Fang J, Li S, Vermeulen MJ, Schull MJ. The association between emergency department crowding and the disposition of patients with transient ischemic attack or minor stroke. Acad Emerg Med 2015; 22(10):1145-54. doi: 10.1111/acem.12766 [Crossref] [ Google Scholar]
- Chen EH, Mills AM, Lee BY, Robey JL, Zogby KE, Shofer FS. The impact of a concurrent trauma alert evaluation on time to head computed tomography in patients with suspected stroke. Acad Emerg Med 2006; 13(3):349-52. doi: 10.1197/j.aem.2005.10.011 [Crossref] [ Google Scholar]
- Zhu HF, Newcommon NN, Cooper ME, Green TL, Seal B, Klein G. Impact of a stroke unit on length of hospital stay and in-hospital case fatality. Stroke 2009; 40(1):18-23. doi: 10.1161/strokeaha.108.527606 [Crossref] [ Google Scholar]
- Field TS, Green TL, Roy K, Pedersen J, Hill MD. Trends in hospital admission for stroke in Calgary. Can J Neurol Sci 2004; 31(3):387-93. doi: 10.1017/s0317167100003504 [Crossref] [ Google Scholar]
- Wilson E, Taylor G, Phillips S, Stewart PJ, Dickinson G, Ramsden VR. Creating a Canadian stroke system. CMAJ 2001; 164(13):1853-5. [ Google Scholar]
- Alberts MJ, Latchaw RE, Selman WR, Shephard T, Hadley MN, Brass LM. Recommendations for comprehensive stroke centers: a consensus statement from the Brain Attack Coalition. Stroke 2005; 36(7):1597-616. doi: 10.1161/01.STR.0000170622.07210.b4 [Crossref] [ Google Scholar]
- Kaste M, Skyhoj Olsen T, Orgogozo J, Bogousslavsky J, Hacke W. Organization of stroke care: education, stroke units and rehabilitation European Stroke Initiative (EUSI). Cerebrovasc Dis 2000; 10 Suppl 3:1-11. doi: 10.1159/000047576 [Crossref] [ Google Scholar]
- Alberts MJ, Hademenos G, Latchaw RE, Jagoda A, Marler JR, Mayberg MR. Recommendations for the establishment of primary stroke centers Brain Attack Coalition. JAMA 2000; 283(23):3102-9. doi: 10.1001/jama.283.23.3102 [Crossref] [ Google Scholar]
- Hakim AM, Silver F, Hodgson C. Is Canada falling behind international standards for stroke care?. Cmaj 1998; 159(6):671-3. [ Google Scholar]
- Ayromlou H, Soleimanpour H, Farhoudi M, Taheraghdam A, Sadeghi Hokmabadi E, Rajaei Ghafouri R. Eligibility assessment for intravenous thrombolytic therapy in acute ischemic stroke patients; evaluating barriers for implementation. Iran Red Crescent Med J 2014; 16(5):e11284. doi: 10.5812/ircmj.11284 [Crossref] [ Google Scholar]
- Soleimanpour H. Bilirubin: from a disease predictor to a potential therapeutic in stroke. Int J Aging 2023; 1:e1. doi: 10.34172/ija.2023.e1 [Crossref] [ Google Scholar]