Int J Aging.2023;1 :e9.
doi: 10.34172/ija.2023.e9
Original Article
The Burden of Ischemic Heart Disease Among Adults 70 Years and Older in Iran, 1990-2019
Seyed Ehsan Mousavi 1  , Asra Fazlollahi 1, Seyed Aria Nejadghaderi 2, 3
, Asra Fazlollahi 1, Seyed Aria Nejadghaderi 2, 3  , Armin Aslani 1, Mark J. M. Sullman 4, 5, Ali-Asghar Kolahi 6, *
, Armin Aslani 1, Mark J. M. Sullman 4, 5, Ali-Asghar Kolahi 6, * 
Author information:
1Social Determinants of Health Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
2Research Center for Integrative Medicine in Aging, Aging Research Institute, Tabriz University of Medical Sciences, Tabriz, Iran
3Systematic Review and Meta-analysis Expert Group (SRMEG), Universal Scientific Education and Research Network (USERN), Tehran, Iran
4Department of Life and Health Sciences, University of Nicosia, Nicosia, Cyprus
5Department of Social Sciences, University of Nicosia, Nicosia, Cyprus
6Social Determinants of Health Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Abstract
Objectives:
To report the ischemic heart disease (IHD) burden and its risk factors among adults aged 70 and older in Iran in terms of sex, at both the national and provincial levels, from 1990 to 2019.
Design:
Systematic analysis.
Outcome measures:
The modelled point prevalence of IHD, years of life lost (YLLs), years lived with disability (YLDs), and disability-adjusted life years (DALYs) were reported using data obtained from the Global Burden of Disease (GBD) 2019 study, as counts and standardized rates, along with their related 95% uncertainty intervals (UIs).
Results:
In 2019, IHD had a point prevalence of 52886.4 per 100000 population for adults aged 70 and above in Iran, which was 7.5% higher than that in 1990, and a death rate of 1932.9, which was 22.0% lower than that in 1990. In 2019, the number of DALYs attributed to IHD was 820.4 thousand with a rate of 23630.9, which was 33.7% lower than that in 1990. Furthermore, Golestan and Tehran with rates of 32484.6 and 12752.5 had the largest and smallest DALY rates in those aged 70 and above in Iran, respectively. The highest point prevalence, death, and DALY rates for both sexes, were found in the 95+age group. In 2019, the Iran DALY rate was lower than the Middle East and North Africa region rate in all age groups in males and females, except for the 90-94 and 95+age groups in females. Nationally, systolic blood pressure (SBP) (47.8%), low-density lipoprotein (LDL) cholesterol (36.2%), and fasting plasma glucose (FPG) (35.3%) had the three highest attributable DALYs.
Conclusions:
Currently, the burden of IHD in Iran is considered a pressing public health issue, indicating the urgent need for effective public health interventions. Further investigations are, therefore, needed to discover causes for the high prevalence of IHD in the country and to develop better strategies for effective prevention and controlling it.
Keywords: Ischemic heart disease, Geriatrics, Iran, Global burden of disease, Risk factor
Introduction
Ischemic heart disease (IHD) refers to a pathological condition in which the myocardium weakens and consequently becomes unable to effectively pump blood throughout the body.1 As the oxygenation of the heart mainly depends on the amount of coronary blood flow,2 a coronary artery stenosis or formation of an intravascular thrombosis at the site of a ruptured atherosclerotic plaque may cause hypoperfusion and eventually results in myocardial infarction.1 Common factors associated with an increased risk of IHD are often categorized as non-modifiable factors (e.g., aging, male sex, and positive family history), semi-modifiable factors, which include comorbidities such as hypercholesterolemia, diabetes, high blood pressure, renal diseases, and obesity, and modifiable factors, including smoking, alcohol consumption, and a sedentary lifestyle.3
IHD imposes a huge burden on the quality of life worldwide.4 In 2019, there were an estimated 197 million prevalent cases of IHD globally.5 The same study also reported that the total number of IHD-attributable disability-adjusted life years (DALYs) have increased consistently since 1990, reaching 182 million DALYs and 9.14 million deaths in 2019, meaning that it was the most common cause of death globally.5
Similar to global estimates, IHD is a large contributor to the disease burden in Iran, raising lots of unpleasant consequences in terms of different aspects of human health.6 The rapidly aging population and the high prevalence of IHD risk factors, including hypertension and diabetes, predispose the country to a huge burden of this disease.7 According to the Global Burden of Disease (GBD) study, the age-standardized prevalence of IHD in 2017 was 1876.5 (per 100 000 population), and its annual incidence rate was 158.8 (per 100 000 population) in Iran.4
While the global burden of IHD was described in GBD 20178 and GBD 2019,5 the country-specific levels were not reported. However, a study that investigated the global, regional, and national burden of IHD reported the epidemiological indicators in Iran between 1990 and 2017, but this study did not provide detailed information on the epidemiological patterns of IHD in Iran or its attributable risk factors.4 Therefore, the present research aimed to provide the most up-to-date information regarding the point prevalence, years of life lost (YLLs), years lived with disability (YLDs) and DALYs in adults aged 70 years and older in Iran based on sex, from 1990 to 2019, at both the national and provincial levels.
Methods
Overview
The GBD 2019 study measured the burden of almost 370 illnesses and injuries as well as 87 risk factors across over 200 nations and territories from 1990 to 2019.9,10 The burden of IHD among Iran’s older population has not yet been comprehensively estimated. As a result, the present article reports the burden of IHD in the Iranian population aged 70 and older from 1990 to 2019. The GBD capstone studies include a thorough description of the techniques used to map the attributable burden of IHD.9,10 More information on the estimates (fatal and non-fatal) is available at https://vizhub.healthdata.org/gbd-compare/ and http://ghdx.healthdata.org/gbd-results-tool.
Case Definition
In this study, we present an overview of the GBD methodology, and a more in-depth description is provided elsewhere.9,10 IHD is defined as acute myocardial infarction (MI) and chronic IHD. According to the third universal definition of acute myocardial infarction, MI is defined as when there is (1) clinical evidence of myocardial necrosis from a clinical environment, (2) an increase or decrease in cardiac biomarker values with one of the following: (i) symptoms of cardiac ischemia, (ii) new or presumed new ST-segment-T wave changes or left bundle branch block, (iii) development of pathological Q waves in electrocardiography, (iv) Changes in regional wall motion or the loss of viable myocardium exhibited in imaging, or (v) determination of the presence of a thrombus inside the coronary arteries using angiography or postmortem examination, (3) abrupt unexplained cardiac death, with or without proof of a non-coronary cause of death, (4) prevalent MI, which is defined as lasting from the commencement of the incident to 28 days after the occurrence and is classified as acute (0-2 days) and subacute (0-2 days), lasting 3–28 days.9 Furthermore, chronic IHD is defined as asymptomatic IHD succeeding MI, with the incidence of surviving 28 days after the MI, and clinically diagnosed stable exertional angina pectoris or definite angina pectoris, according to the Rose Angina Questionnaire, physician diagnosis, or the use of nitrate medication to relieve chest pain.9
Fatal Estimation
Vital registration and verbal autopsy data were used to create the cause of death database. Premature mortality from IHD was calculated using the standard Cause of Death Ensemble model (CODEm), with the location-level covariates, which are presented in the appendix section of the GBD 2019 publication.10 Then, CODCorrect was applied to an age-sex-state-year group to revise the total number of expected deaths from a single cause. Finally, data from the GBD standard life table were used to determine the YLLs, by multiplying the total number of deaths by the remaining life expectancy for each age group.
Non-fatal Estimation
A systematic review was done to update the GBD 2019 database for MI. Inpatient hospital, inpatient claims data, and literature for MI were used to create a nonfatal database. The excess mortality data points were split based on age ranges above 25 years. The incidence data with wide age ranges were excluded as they tend to mask the increasing risk of MI with advancing age in the estimates generated from DisMod. Meta-regression –Bayesian regularized trimmed modelling tool with multiple covariates was used to crosswalk the incidence measurements for MI from literature using alternative definitions to the reference case definition. In GBD 2019, no systematic review was conducted for asymptomatic IHD after MI.9 The 28-day survivors computed from the excess mortality estimates for the MI model were the key input for this model. To inform estimations of survival following MI, we incorporated data for excess mortality and the standardized mortality ratio. Additionally, no systematic review has been conducted for angina since GBD 2013. Finally, the World Health Study questionnaires, National Health and Nutrition Examination Survey, and United States claim data were used to estimate the prevalence of angina.9
Modelling Strategy, Severity, and Years Lived with Disability
Before the redistribution of garbage codes, the age-sex-country-specific proportions of IHD fatalities from MI versus other causes (chronic IHD) were estimated with the cause of death data. A DisMod proportion-only model estimated age-sex-country-specific proportions of IHD fatalities for all locations.9 To estimate the cause-specific mortality rate due to MI, the global proportions were multiplied by post-Fauxcorrect IHD deaths by location. These data, along with incidence and excess mortality data, guided a DisMod model to predict the prevalence and incidence of IHD-related MI. These estimates were divided into estimates for 1-2 days and 3-28 days following the incident, with severity estimations of 0.432 and 0.074, respectively.9
The MI model of excess mortality estimates was utilized to calculate the incidence of surviving 28 days post-event. The prevalence of IHD after MI was calculated using these data, the cause-specific mortality rate attributable to chronic IHD, and excess mortality data based on a DisMod model. Based on the literature, a portion of this estimate was deleted to avoid double-counting people with angina and heart failure. This stage estimated post-MI asymptomatic IHD.9
We estimated the prevalence and incidence of angina for all locations using the literature, prevalence data, and mortality risk data sourced from US claims data. MR-BRT-modified Rose Angina Questionnaire data were used to estimate the prevalence of angina. The severity levels for angina pectoris were mild, moderate, and severe angina, with disability weights of 0.033, 0.08, and 0.167, respectively.9
Compilation of Results
To compute the YLLs, the number of deaths in each age group was multiplied by the remaining years of life expected in each age group, as defined by the GBD standard lifetable. The YLDs and YLLs were added together to get the number of DALYs. Then, the GBD standard population was used to standardize all estimates, and all estimates included 95% uncertainty intervals (UIs).9
Risk Factors
All risk factors that were proven to cause IHD were included in this study.10 The proportion of DALYs attributed to the risk factors was estimated by sex at national and provincial levels. The definitions and relative risks of these risk factors were reported elsewhere.10
Results
National Level
In 2019, there were 1.8 million (95% UI: 1.6 to 2.0) prevalent cases of IHD, with a point prevalence of 52886.4 (95% UI: 47543.0 to 58381.6), which was 7.5% (95% UI: 5.5 to 9.9) higher than that in 1990. That same year, IHD caused 67.1 thousand (95% UI: 59.7 to 72.7) deaths, with a death rate of 1932.9 (95% UI: 1720.8 to 2094.2), which was 22.0% (95% UI: -29.2 to -15.1) lower than that in 1990. Furthermore, IHD accounted for 820.4 thousand (95% UI: 745.7 to 882.3) DALYs in 2019, with a DALY rate of 23630.9 (95% UI: 21476.7 to 25413.7), which was 33.7% (95% UI: -39.8 to -28.0) lower than that in 1990 (Table 1).
Table 1.
Prevalent Cases, Deaths, and DALYs Due to Ischemic Heart Disease for Adults Aged 70 and Older in 1990 and 2019 for Both Sexes and Percentage Change in Rates per 100 000 in Iran
|
|
Prevalence (95% UI)
|
Deaths (95% UI)
|
DALYs (95% UI)
|
Counts
(2019)
|
Rate
(2019)
|
Pcs in Rate
1990-2019
|
Counts
(2019)
|
Rate
(2019)
|
Pcs in Rate
1990-2019
|
Counts
(2019)
|
Rate
(2019)
|
Pcs in rate
1990-2019
|
| Iran |
1836178
(1650657, 2026967) |
52886.4
(47543, 58381.6) |
7.5
(5.5, 9.9) |
67109
(59744, 72711) |
1932.9
(1720.8, 2094.2) |
-22
(-29.2, -15.1) |
820446.5
(745654.2, 882346.2) |
23630.9
(21476.7, 25413.7) |
-33.7
(-39.8, -28) |
| Alborz |
58755
(52833, 65026) |
54271.9
(48800.9, 60064.3) |
3
(-0.5, 6) |
2257
(1942, 2548) |
2085.2
(1794.2, 2353.9) |
-17.9
(-32.6, 1.3) |
29117.5
(25305.7, 32851.1) |
26895.5
(23374.6, 30344.3) |
-22.1
(-36.3, -3.6) |
| Ardebil |
31154
(28129, 34201) |
55302.1
(49932.9, 60710.3) |
9.3
(5.8, 13) |
1423
(1250, 1565) |
2525.7
(2219.6, 2778.2) |
-9.7
(-23.5, 8.6) |
17309.7
(15358.1, 19006.5) |
30726.7
(27262.4, 33738.9) |
-19.7
(-32.7, -3.1) |
| Bushehr |
19768
(17684, 21841) |
53552.9
(47905, 59168.5) |
0.8
(-2.3, 4.6) |
765
(680, 847) |
2072.8
(1843.1, 2295.8) |
-23.3
(-34.4, -8.3) |
10151.9
(9079.8, 11254.7) |
27501.6
(24597.3, 30489.2) |
-30.8
(-41.2, -16.6) |
| Chahar Mahaal and Bakhtiari |
20159
(18067, 22236) |
53520.9
(47965.7, 59033.8) |
11
(6.8, 15.4) |
977
(830, 1126) |
2594.7
(2203.8, 2990.7) |
-11
(-25.9, 7.4) |
11460
(9823.8, 13236.9) |
30425
(26081.1, 35142.6) |
-27.1
(-39.6, -11.2) |
| East Azarbayejan |
99119
(89209, 109612) |
53615.6
(48255.2, 59291.9) |
5.9
(2.2, 10) |
3480
(3014, 4223) |
1882.3
(1630.5, 2284.5) |
-29.3
(-41.2, -14.6) |
44468
(38696.4, 53470) |
24053.9
(20931.9, 28923.2) |
-35.3
(-46.7, -21.6) |
| Fars |
97502
(87215, 108475) |
48815.2
(43664.9, 54308.6) |
4
(0.2, 8) |
4362
(3723, 5022) |
2183.9
(1864, 2514.5) |
-27
(-38.9, -10.7) |
51690.7
(44550.2, 59653) |
25879.3
(22304.3, 29865.7) |
-40.2
(-50.1, -25.8) |
| Gilan |
84808
(76187, 93482) |
54377.3
(48849.7, 59938.7) |
14.1
(9.8, 18.6) |
3780
(3273, 4252) |
2423.9
(2098.6, 2726) |
-17.7
(-30.2, -2.3) |
46347.3
(40647.2, 52183.4) |
29716.9
(26062.1, 33458.8) |
-31.3
(-42.3, -17.6) |
| Golestan |
32783
(29373, 36054) |
53388.7
(47836.5, 58716) |
6.7
(2.8, 10.6) |
1548
(1373, 1693) |
2520.2
(2236.6, 2757.2) |
-14.6
(-25.9, 2.4) |
19946.7
(17981.6, 21875.3) |
32484.6
(29284.4, 35625.5) |
-24.5
(-35.6, -8.9) |
| Hamadan |
47643
(42640, 52893) |
50447.8
(45149.6, 56006.6) |
14.1
(8.9, 19.4) |
2427
(2065, 2721) |
2569.8
(2186.3, 2881.6) |
-5.9
(-21.2, 12.1) |
29140.7
(25317.9, 32628.6) |
30856
(26808.3, 34549.3) |
-24.4
(-37.5, -9.5) |
| Hormozgan |
25861
(23214, 28482) |
51444.3
(46177.8, 56656.5) |
7
(2.7, 11) |
1050
(908, 1168) |
2087.9
(1805.4, 2324.1) |
-26.8
(-38.1, -9.9) |
12920
(11302.4, 14288.3) |
25700.9
(22483.1, 28422.7) |
-39.1
(-48.9, -23.4) |
| Ilam |
9650
(8624, 10622) |
51726.7
(46226.7, 56936.4) |
1.2
(-1.9, 4.2) |
468
(409, 513) |
2507.5
(2191.6, 2750.8) |
-34
(-42, -23.9) |
5677.6
(5050.2, 6191.7) |
30432.7
(27070, 33188.1) |
-38.9
(-46.7, -29.2) |
| Isfahan |
129309
(116064, 142800) |
51229.2
(45982, 56573.9) |
9.8
(5.5, 14.4) |
5273
(4529, 5998) |
2089.2
(1794.2, 2376.3) |
-12.9
(-28, 8.2) |
63350.2
(54699.7, 71923) |
25097.9
(21670.8, 28494.2) |
-26.3
(-39.6, -7.5) |
| Kerman |
60710
(54632, 67075) |
54821.4
(49333, 60568.5) |
7.4
(3.5, 11.8) |
2329
(1997, 2658) |
2103.4
(1803.2, 2400.2) |
-27.1
(-39.4, -13.3) |
27610.2
(23772.5, 31451.1) |
24932.1
(21466.6, 28400.3) |
-42.9
(-52.5, -31.3) |
| Kermanshah |
46386
(41733, 50955) |
54013.7
(48595.7, 59334.3) |
10.6
(6.8, 14.6) |
2059
(1781, 2343) |
2397.3
(2073.9, 2727.9) |
-20.4
(-33.4, -3.6) |
25119.6
(22050.1, 28469.8) |
29250.4
(25676.1, 33151.5) |
-33.2
(-44.6, -18.7) |
| Khorasan-e-Razavi |
143616
(128958, 158679) |
54336.9
(48791.1, 60036.2) |
6.3
(2.7, 10.3) |
5033
(4322, 5853) |
1904
(1635.4, 2214.6) |
-30.1
(-41.8, -17.4) |
63499.4
(55451.7, 73426.6) |
24025
(20980.1, 27780.9) |
-42.6
(-52.4, -32.2) |
| Khuzestan |
89988
(81192, 99086) |
55891.5
(50428.3, 61542.1) |
8.8
(5.5, 12.4) |
3973
(3471, 4442) |
2467.8
(2156.1, 2758.6) |
-12.1
(-25.2, 4) |
49145.4
(43468.1, 54978.9) |
30524.1
(26997.9, 34147.2) |
-23.9
(-35.5, -9.3) |
| Kohgiluyeh and Boyer-Ahmad |
11501
(10387, 12668) |
54028.2
(48791.1, 59505.9) |
14
(9.7, 18.2) |
569
(471, 663) |
2674
(2213.1, 3113.9) |
2.5
(-16.6, 25.6) |
6559.7
(5468.1, 7644.4) |
30814.2
(25686.5, 35909.6) |
-12.4
(-29.2, 8.4) |
| Kurdistan |
35712
(32182, 39204) |
52569.7
(47373.2, 57709.9) |
8
(4.3, 11.8) |
1419
(1213, 1588) |
2088.5
(1785.4, 2338.3) |
-31
(-40.9, -19.3) |
17230.1
(15075.4, 19130.6) |
25363.5
(22191.6, 28161.1) |
-40.4
(-49.4, -30) |
| Lorestan |
38364
(34564, 42309) |
52578.3
(47371.4, 57985.5) |
8.4
(4.6, 12.5) |
1830
(1579, 2059) |
2508
(2164.1, 2822) |
-9.8
(-24.1, 7.5) |
22559.9
(19465.7, 25427.7) |
30918.8
(26678.2, 34849.2) |
-22.1
(-35, -7.1) |
| Markazi |
47049
(42523, 51891) |
56126.7
(50727.6, 61902.7) |
13.4
(9.1, 18.3) |
1454
(1226, 1717) |
1734.7
(1462.2, 2048.6) |
-23
(-36.3, -7.6) |
16863.8
(14408.6, 19796.3) |
20117.6
(17188.6, 23615.9) |
-38.9
(-49.7, -26) |
| Mazandaran |
96580
(87692, 106150) |
54920.5
(49866.3, 60362.6) |
11
(7.3, 15.6) |
3360
(2881, 3881) |
1910.9
(1638.4, 2207.2) |
-20.8
(-33.8, -3.9) |
40943.5
(35472.8, 47005) |
23282.7
(20171.8, 26729.6) |
-33.4
(-44.5, -19.1) |
| North Khorasan |
19779
(17833, 21762) |
56005.7
(50496.6, 61621) |
13.3
(8.8, 18.2) |
735
(640, 849) |
2080.2
(1811.4, 2403) |
-6
(-22, 13.5) |
9278
(8181.3, 10698) |
26271.6
(23166.2, 30292.5) |
-23.5
(-36.8, -7.7) |
| Qazvin |
28186
(25331, 31231) |
51845.5
(46595.2, 57447.8) |
7.9
(3.8, 12.4) |
1053
(896, 1188) |
1936.1
(1647.7, 2185.2) |
-11.9
(-27.5, 7.1) |
13127.3
(11330.3, 14847.1) |
24146.8
(20841.3, 27310.3) |
-26.6
(-39.7, -10.5) |
| Qom |
26072
(23433, 28710) |
54624.3
(49095.3, 60150.2) |
7.9
(3.8, 11.8) |
958
(816, 1071) |
2006.4
(1708.8, 2243.6) |
2.4
(-16.1, 27.3) |
11638.1
(10072.3, 12938.9) |
24383
(21102.5, 27108.3) |
-14.9
(-30.3, 7) |
| Semnan |
18507
(16640, 20454) |
54746.5
(49222.2, 60505.2) |
7
(3.2, 10.7) |
618
(529, 715) |
1828.4
(1563.4, 2114.3) |
-13.9
(-27.6, 4.6) |
7865.7
(6754.3, 9099.7) |
23267.8
(19980.2, 26918.2) |
-28.3
(-40.1, -11.6) |
| Sistan and Baluchistan |
28115
(25204, 31083) |
49451.5
(44330.7, 54670.4) |
8.7
(4.5, 13.8) |
1001
(828, 1175) |
1761.4
(1456.2, 2067.1) |
-14
(-30.1, 8.7) |
12514.7
(10586.1, 14615.3) |
22011.8
(18619.7, 25706.4) |
-28.7
(-42.4, -6.6) |
| South Khorasan |
21293
(19168, 23425) |
53022.2
(47731, 58331.3) |
10.7
(5.5, 15.4) |
716
(608, 824) |
1783.9
(1513.5, 2052.2) |
-3.3
(-19.2, 16) |
8417.1
(7226, 9625.5) |
20959.6
(17993.5, 23968.6) |
-23.5
(-36.1, -7.9) |
| Tehran |
353082
(317770, 389815) |
51572.9
(46415.1, 56938.2) |
2.8
(-0.3, 6.5) |
7391
(6080, 8647) |
1079.6
(888, 1263) |
-27.8
(-42.9, -8.6) |
87307
(73612.8, 101642.2) |
12752.5
(10752.2, 14846.3) |
-34.1
(-48.1, -16.7) |
| West Azarbayejan |
59888
(53627, 66427) |
50361.2
(45096.1, 55860) |
7.5
(3.8, 11.9) |
2790
(2461, 3120) |
2346.3
(2069.4, 2624.1) |
-23.1
(-34.6, -9.4) |
34794.5
(30757.3, 38886.4) |
29259.4
(25864.5, 32700.5) |
-31.5
(-42, -18.2) |
| Yazd |
26417
(23749, 29044) |
56365
(50673.4, 61970.6) |
11
(6.9, 15.5) |
816
(694, 971) |
1740.8
(1480.2, 2071.9) |
-18
(-32.8, 0.6) |
9895.7
(8466.7, 11616.3) |
21114.2
(18065.1, 24785.4) |
-33.3
(-45.2, -17.2) |
| Zanjan |
28421
(25517, 31300) |
54070.1
(48546.1, 59547.2) |
10.9
(7.2, 15.2) |
1194
(1029, 1312) |
2271.9
(1957.7, 2495.6) |
-5.8
(-19.7, 10.2) |
14496.6
(12705.9, 15915.5) |
27579.6
(24172.7, 30279.1) |
-21.9
(-34.3, -8) |
Note. DALY: Disability-adjusted life year; UI: Uncertainty interval.
Provincial Level
In 2019, the highest point prevalent cases were found in Yazd [56365.0 (95% UI: 50673.4 to 61970.6)], Markazi [56126.7 (95% UI: 50727.6 to 61902.7)], and North Khorasan [56005.7 (95% UI: 50496.6 to 61621.0)], while the lowest cases were reported in Fars [48815.2 (95% UI: 43664.9 to 54308.6)], Sistan and Baluchistan [49451.5 (95% UI: 44330.7 to 54670.4)], and West Azarbayejan [50361.2 (95% UI: 45096.1 to 55860)], as depicted in Figure 1A and Table S1. The 201 sex-specific point prevalence of IHD for adults aged 70 and older at the provincial level is presented in Figure S1.
In 2019, the highest death rates were found in Kohgiluyeh and Boyer-Ahmad [2674.0 (95% UI: 1635.4 to 2214.6)], Chahar Mahaal and Bakhtiari [2594.7 (95% UI: 2203.8 to 2990.7)], and Hamadan [2569.8 (95% UI: 2186.3 to 2881.6)]. In contrast, the lowest rates were found in Tehran [1079.6 (95% UI: 888.0 to 1263.0)], Markazi [1734.7 (95% UI: 1462.2 to 2048.6)], and Yazd [1740.8 (95% UI: 1480.2 to 2071.9)], as illustrated in Figure 1B and Table S2. Figure S2 presents the sex-specific death rates for adults aged 70 and older at the provincial level.
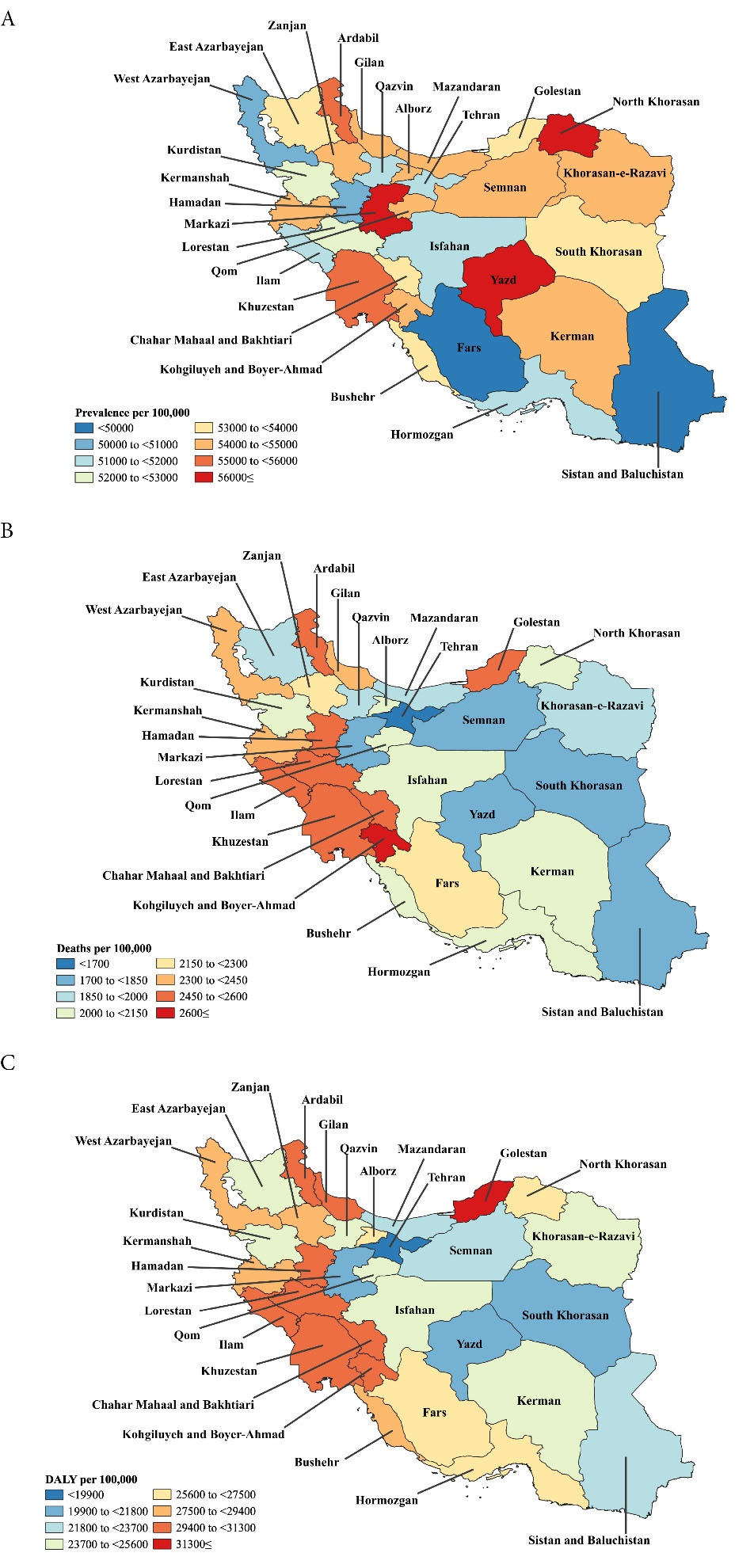
Figure 1.
Point Prevalence (A), Deaths (B), and DALY Rates (C) for Ischemic Heart Disease (Per 100 000 Population) for Adults Aged 70 Years and Older in Iran in 2019 by Province. Note. DALY: Disability-adjusted life year. Using data from http://ghdx.healthdata.org/gbd-results-tool
.
Point Prevalence (A), Deaths (B), and DALY Rates (C) for Ischemic Heart Disease (Per 100 000 Population) for Adults Aged 70 Years and Older in Iran in 2019 by Province. Note. DALY: Disability-adjusted life year. Using data from http://ghdx.healthdata.org/gbd-results-tool
The highest DALY rates in 2019 were found in Golestan [32484.6 (95% UI: 29284.4 to 35625.5)], Lorestan [30918.8 (95% UI: 26678.2 to 34849.2)], and Hamadan [30856.0 (95% UI: 26808.3 to 34549.3)]. Conversely, the lowest DALY rates were observed in Tehran [12752.5 (95% UI: 10752.2 to 14846.3)], Markazi [20117.6 (95% UI: 17188.6 to 23615.9)], and South Khorasan [20959.6 (95% UI: 17993.5 to 23968.6)], as depicted in Figure 1C and Table S3. Moreover, the 2019 sex-specific DALY rates are presented at the provincial level in Figure S3.
The highest increases in the point prevalence of IHD, between 1990-2019, were seen in Hamadan [14.1% (95% UI: 8.9 to 19.4)], Gilan [14.1% (95% UI: 9.8 to 18.6)], and Kohgiluyeh and Boyer-Ahmad [14.0% (95% UI: 9.7 to 18.2)]. Conversely, the lowest increases were found in Bushehr [0.8% (95% UI: -2.3 to 4.6)], Ilam [1.2% (95% UI: -1.9 to 4.2)], and Tehran [2.8% (95% UI: -0.3 to 6.5)]. As Table 1 indicates, the point prevalence of IHD did not decrease in any of the provinces of Iran. Further, Figure S4 presents the sex-specific estimates at the provincial level for the percentage change in the point prevalence of IHD for adults aged 70 and above from 1990 to 2019 in Iran.
The IHD-attributable death rate for adults aged 70 and older in Iran decreased from 1990 to 2019 in all provinces, except for Kohgiluyeh and Boyer-Ahmad and Qom which increased by 2.5% (95% UI: -16.6 to 25.6) and 2.4% (95% UI: -16.1 to 27.3), respectively. The highest decreases, from 1990 to 2019, were found in Ilam [-34.0% (95% UI: -42.0 to -23.9)], Kurdistan [-31.0% (95% UI: -40.9 to -19.3)], and Khorasan-e-Razavi [-30.1% (95% UI: -41.8 to -17.4)], as illustrated in Table 1. Further, Figure S5 presents the sex-specific percentage change in the death rates for each province from 1990 to 2019.
Table S3 indicates that the DALY rate for IHD among adults aged 70 and above did not increase in Iran from 1990 to 2019. The largest decreases, from 1990 to 2019, were observed in Kerman [-42.9% (95% UI: -52.5 to -31.3)], Khorasan-e-Razavi [-42.6% (95% UI: -52.4 to -32.2)], and Kurdistan [-40.4% (95% UI: -49.4 to -30.0)] during the measurement period. Moreover, Figure S6 displays the sex-specific percentage changes in the DALY rates at the provincial level over the period 1990 to 2019.
Age and Sex Patterns
The results suggested that the 2019 national point prevalence and prevalent cases of IHD are higher for males than for females in the geriatric population. The highest number of prevalent cases were found in the 70-74 age group, and the point prevalence increased with increasing age among the elderly in Iran in 2019 (Figure 2A). For both sexes, the highest death rate in 2019 was found in the 95 + age group, while the highest number of deaths was found in the 80-84 age group (Figure 2B).
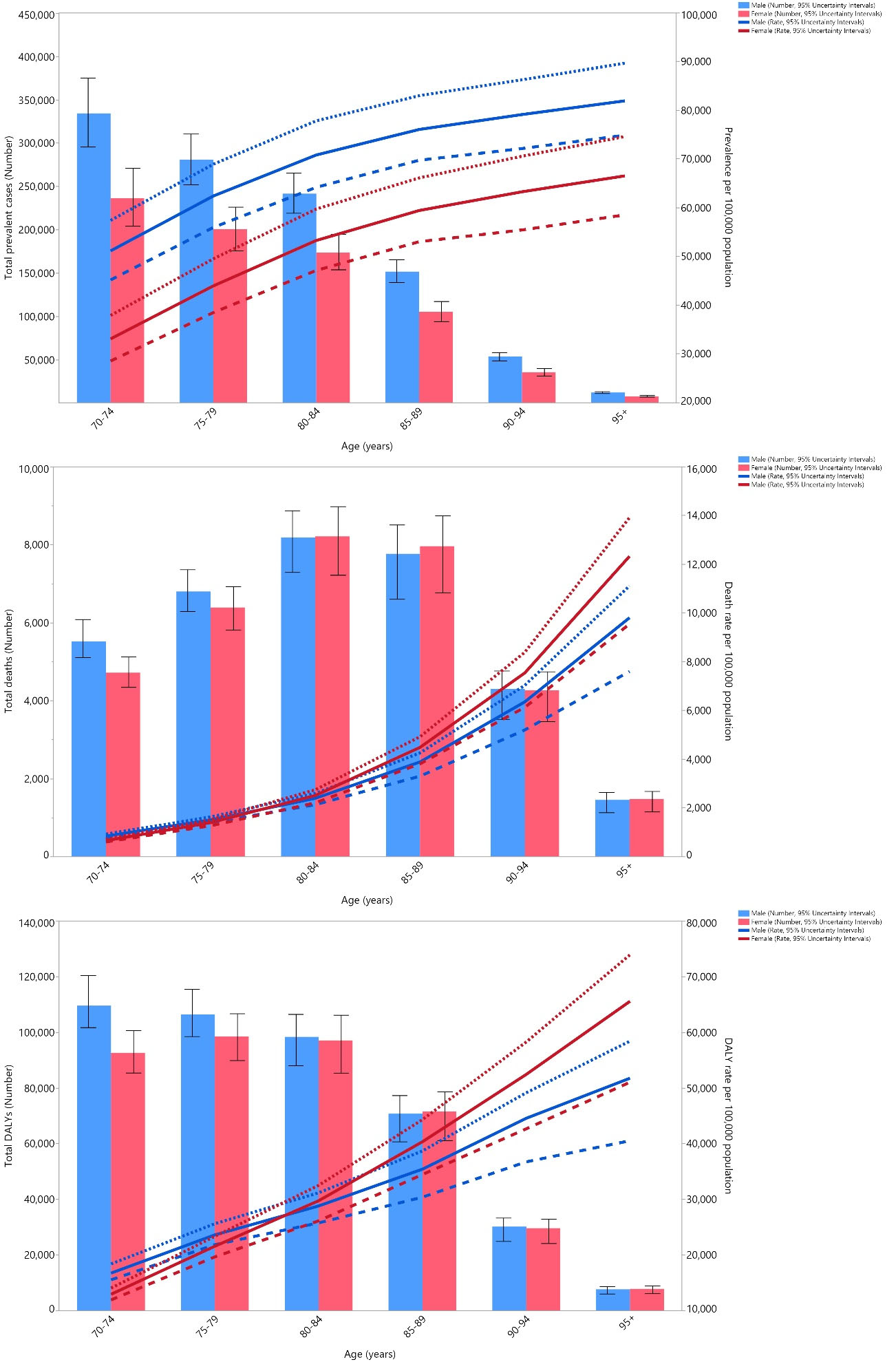
Figure 2.
The Number of Prevalent Cases and Prevalence (A), Number of Death Cases and Death Rate (B), and the Number of DALYs and DALY Rate (C) for Ischemic Heart Disease (Per 100 000 Population) in Iran in 2019 by Age and Sex. Note. DALY: Disability-adjusted life year. Dotted and dashed lines indicate 95% upper and lower uncertainty intervals, respectively. Using data from http://ghdx.healthdata.org/gbd-results-tool
.
The Number of Prevalent Cases and Prevalence (A), Number of Death Cases and Death Rate (B), and the Number of DALYs and DALY Rate (C) for Ischemic Heart Disease (Per 100 000 Population) in Iran in 2019 by Age and Sex. Note. DALY: Disability-adjusted life year. Dotted and dashed lines indicate 95% upper and lower uncertainty intervals, respectively. Using data from http://ghdx.healthdata.org/gbd-results-tool
In 2019, the national DALY rate increased with age in both males and females. Moreover, the largest number of DALYs in 2019 was observed in the 70-74 age group and the 75-79 age group for males and females, respectively (Figure 2C).
In 2019, the IHD-associated DALY rate for adults aged 70 and older in Iran was lower than the MENA DALY rate (ratio of Iran/MENA DALY rate < 1) in all age groups for males and aged 70-89 for females. Overall, the ratio of Iran/MENA DALY rate was higher in 1990 than in 2019 in all age groups for both sexes, except for females above 95 years of age (Figure 3).
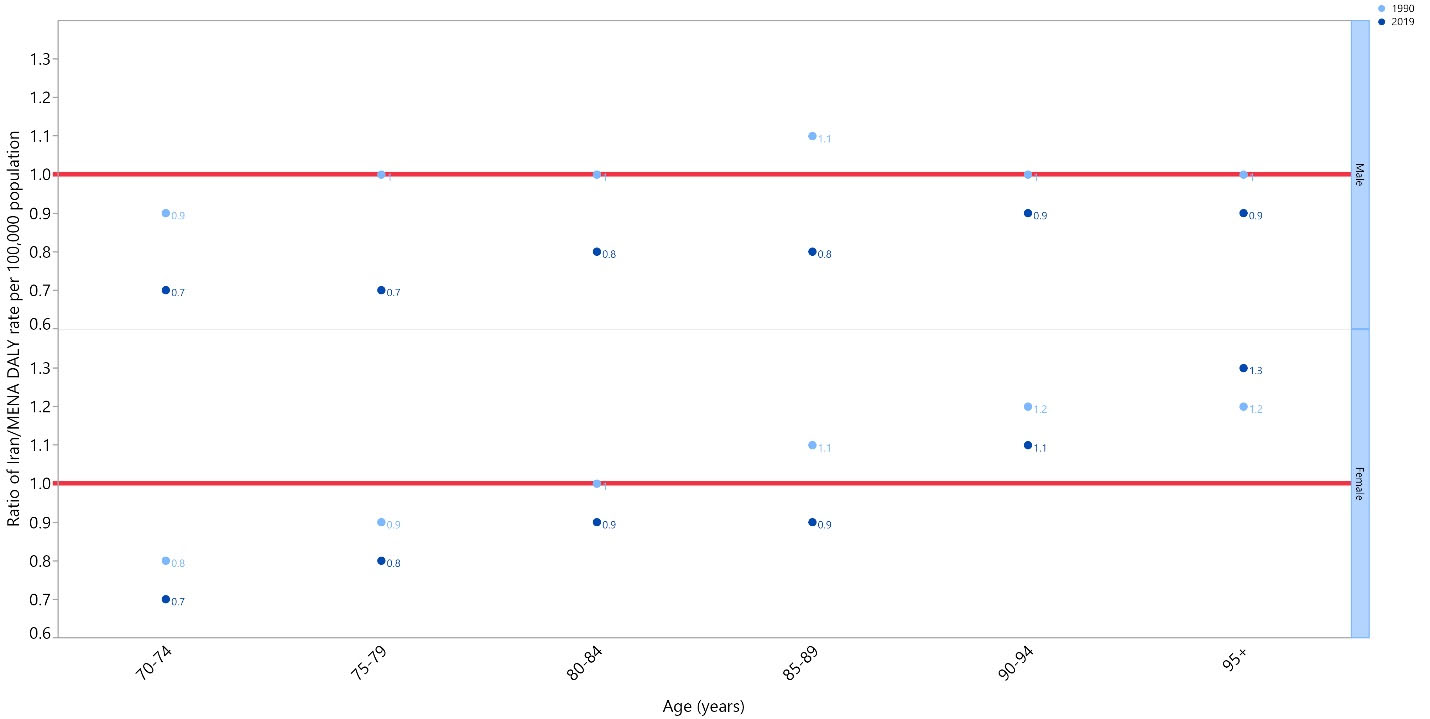
Figure 3.
The Ratio of Iran to Middle East and North Africa Ischemic Heart Disease DALY Rate According to Age Group and Sex between 1990–2019. Note. DALY: Disability-adjusted life year. Using data from http://ghdx.healthdata.org/gbd-results-tool
.
The Ratio of Iran to Middle East and North Africa Ischemic Heart Disease DALY Rate According to Age Group and Sex between 1990–2019. Note. DALY: Disability-adjusted life year. Using data from http://ghdx.healthdata.org/gbd-results-tool
Risk Factors
The proportion of DALYs that were attributable to each risk factor was not the same at the national and provincial levels. Nationally, high systolic blood pressure (SBP) with 47.8%, high low-density lipoprotein (LDL) cholesterol with 36.2%, and high fasting plasma glucose (FPG) with 35.3% had the three highest attributable DALYs. Furthermore, there were wide ranges in the percentage of DALYs attributable in each province, that is, high SBP (from 40.8% in Sistan and Baluchistan to 54.8% in Ardebil), high LDL cholesterol (from 33.7% in Fars and Hamadan to 40.5% in Yazd), and high FPG (from 26.2% in Zanjan to 38.2% in North Khorasan and Khuzestan), as presented in Figure 4. In addition, Figures S7 and S8 illustrate the percent of DALYs that were attributable to each risk factor in Iran and its provinces for males and females individually, respectively.
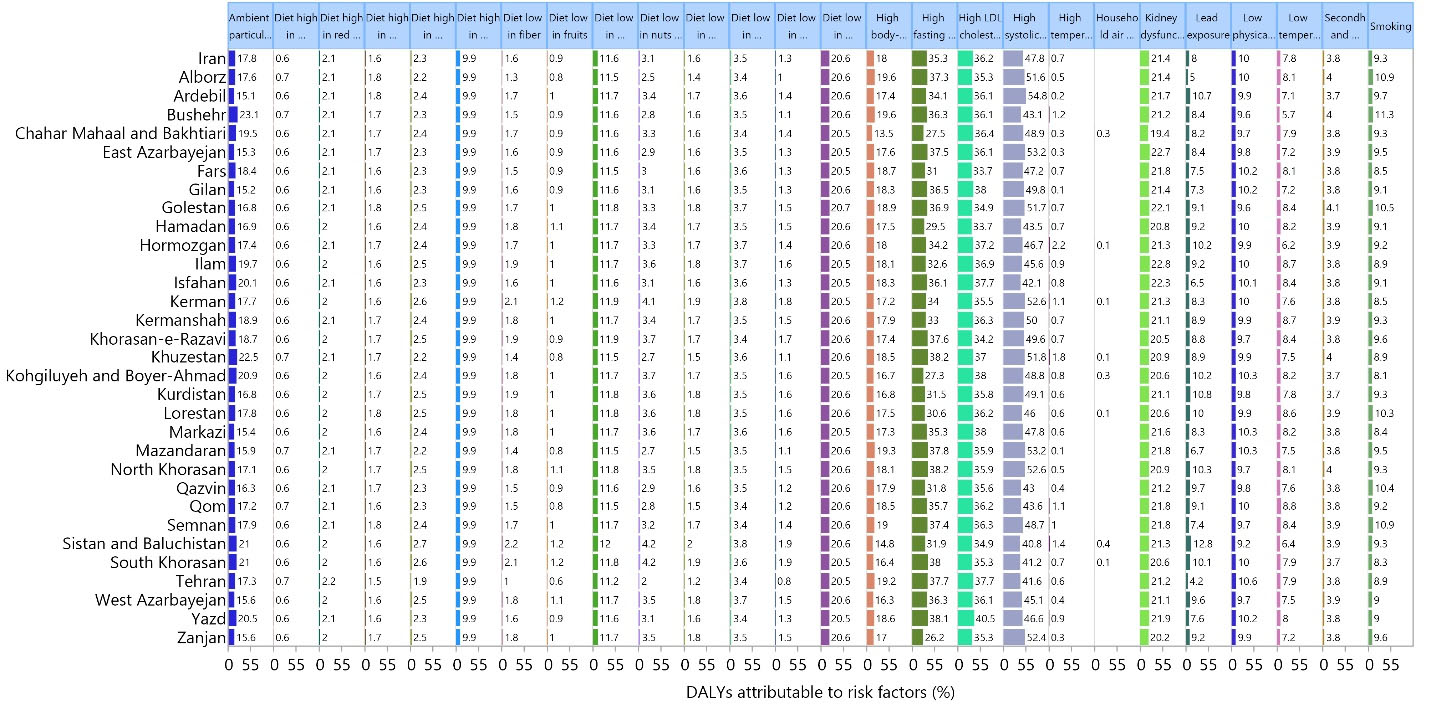
Figure 4.
The Percentage of DALYs due to Ischemic Heart Disease Attributed to Each Risk Factor among Those Aged 70 and Above in Iran in 2019 for Both Sexes. Note. DALY: Disability-adjusted life year. Using data from http://ghdx.healthdata.org/gbd-results-tool
.
The Percentage of DALYs due to Ischemic Heart Disease Attributed to Each Risk Factor among Those Aged 70 and Above in Iran in 2019 for Both Sexes. Note. DALY: Disability-adjusted life year. Using data from http://ghdx.healthdata.org/gbd-results-tool
Discussion
This study was the first to use GBD 2019 data to present recent information on IHD and its related risk factors among individuals aged 70 and older in Iran and its provinces from 1990 to 2019. In 2019, there were 1.8 million prevalent cases of IHD in Iran, with a point prevalence of 52 886.4. The number of prevalent cases increased by 7.5% between 1990 and 2019, and the IHD-attributable death rate was 1932.9 (per 100 000 population), with 67.1 thousand deaths occurring in 2019. The death rate decreased by 22% across the measurement period, and IHD accounted for 820.4 thousand DALYs in 2019, with a DALY rate of 23 630.9. Furthermore, there was a 33.7% decrease in DALYs across the reporting period.
Provincially, the highest point prevalence of IHD in 2019 was found in Yazd, Markazi, and North Khorasan, while the lowest points were found in Fars, Sistan and Baluchistan, and West Azarbayejan. Moreover, the highest death rates were found in Kohgiluyeh and Boyer-Ahmad, Chahar Mahaal and Bakhtiari, and Hamadan, while Tehran, Markazi, and Yazd had the lowest death rates. In 2019, the highest DALY rates were found in Golestan, Lorestan, and Hamadan, while Tehran, Markazi, and South Khorasan had the lowest rates. In addition, the highest increases in the point prevalence, between 1990-2019, were observed in Hamadan, Gilan, and Kohgiluyeh and Boyer-Ahmad, and there were no provinces with a decrease in the point prevalence of IHD. However, the death rate for IHD in adults aged 70 and above decreased in all provinces except for Kohgiluyeh and Boyer-Ahmad and Qom, which exhibited slight increases. Ilam, Kurdistan, and Khorasan-e-Razavi experienced the largest decreases in the death rate for IHD. Additionally, no provinces manifested an increase in the DALY rate of IHD, and Kerman, Khorasan-e-Razavi, and Kurdistan indicated the largest decreases. Nationally, high SBP (47.8%), high LDL cholesterol (36.2%), and high FPG (35.3%) had the three highest attributable DALYs.
In 2014, a cross-sectional study was conducted based on Kherameh cohort study, as a branch of the Prospective Epidemiological Research Studies in IrAN (PERSIAN), which was conducted in 18 different regions of Iran.11 This study was conducted on 10663 people aged 40-70 via cluster sampling to identify the prevalence and risk factors associated with non-communicable diseases.11 Their study reported the age-standardized prevalence rate of IHD among males, females, and both sexes in Iran to be 6.78%, 8.91%, and 8.04%, respectively, which were lower than that in our estimations.11 In addition, the age-standardized prevalence rate of MI among these three groups (males, females, and both sexes) were 3.16%, 1.82%, and 2.44%, respectively.11 The difference between their estimations and ours may be due to the inclusion of individuals younger than those in our research.11 Further, they reported that old age, opium users, smokers, sleeping pill users, and individuals with hypertension have significantly higher odds of having cardiovascular diseases (CVDs).11 Another cross-sectional study, published in 2018, investigated the prevalence of coronary artery disease (CAD) and its risk factors in Borujerd, Iran.12 They conducted the study on 801 people over 35 years old via cluster sampling of individuals with a prior history of CAD.12 The CAD prevalence based on documented history was 9.1%, which was lower than our estimates.12 The differences may again be due to lower age groups, a lower sample size, and methodological discrepancies. Additionally, the prevalent risk factors among those with a history of CAD were hypertension, diabetes mellitus, dyslipidemia, smoking, and obesity.12 Unfortunately, there were no studies investigating the burden of IHD and its risk factors among individuals 70 years and older in all regions of Iran from 1990 to 2019.
IHD is a common cause of morbidity and death globally, and Iran is no exception.13 Furthermore, the burden of IHD and its risk factors is not evenly distributed across Iran. Iran’s recent reforms and developments have resulted in improved health care and an increased life expectancy, in addition to an increased prevalence of non-communicable diseases such as CVDs,10,14 resulting in an increasing burden of IHD. The economic burden of CVDs has recently been highlighted in Iran, with an aging population and rising direct and indirect CVD costs.14,15 The economic burden of CVDs may have a negative impact on the productivity and competitiveness of Iran, increase the economic burden on healthcare systems, exacerbate poverty and unfairness, and reduce opportunity in developing countries.16 The significant economic cost of CVD reduces patients’ access and ability to afford appropriate primary, secondary, and tertiary preventive programs.
To emphasize the importance of primary prevention, particularly in younger age groups, it should be noted that the modifiable risk factors associated with MI can avoid over 90% of MI risk.17 In recent years, the prevalence of lifestyle-related risk factors for CVDs (e.g., smoking, obesity, high blood pressure, insufficient physical activity, and poor diet) has increased significantly in Iran.18-20 A recent population study in Iran examined the trend of seven cardiovascular health metrics from 2007 to 2015, with a total sample size of 37,084 people.19 In 2016, the prevalence of inadequate physical activity, body mass index ≥ 30 mg/dL, poor nutrition score, and mean cardiovascular health index increased significantly when compared to 2007.19 As a result of the increasing trend in the IHD burden and the prevalence of risk factors with a high economic burden, the government’s attention should be drawn to this important public health issue.
The health transformation plan implemented in 2014 was the most recent reform to the Iranian health system, which aimed to increase equity and reduce out-of-pocket expenses for inpatient services in Ministry of Health-affiliated hospitals.21,22 The transformation plan increased the insured patients’ rate, access to health care services, and hospitalization rate23 by reducing the patients’ out-of-pocket expenditures.24-26 In addition, a population-based interventional strategy, aimed at reducing the burden of CVDs is being conducted in Isfahan under the Isfahan Healthy Heart Program.27 This program implemented educational, legislation, mass media, community partnership, and intersectoral collaboration strategies from late 1999 to 2007 with 12,600 individuals.27 Several facilitators and barriers were observed during the administration of the program.28 Factors supporting the program included the involvement of policymakers and stakeholders in projects, political will, and external collaboration, while weak health insurance coverage and low political support were found to be barriers to implementing the program.28
Strengths and Limitations
There has been no previous research to describe the burden of IHD and its attributable risk factors among individuals aged 70 and above in Iran, at both the country and provincial levels. Thus, one strength of the current study is that it exclusively and comprehensively addressed the burden of IHD in Iran. However, the estimates of this study must be read in light of the study’s limitations. Firstly, despite significant efforts to improve data accuracy in GBD studies, there is a probability of misclassification of IHD death because CVDs result from the contributions of multiple coexisting pathological conditions, and it could be sometimes difficult to attribute the occurrence of death to one specific condition. Secondly, the GBD dataset presents data at both the country and provincial levels, so in a vast country such as Iran, large variations in the burden of IHD can exist even at the city level. Thus, providing an overall estimate of aggregated data on IHD for all cities of a province cannot be helpful enough for health system managers and policymakers to address the issue at the city level.
Conclusions
In conclusion, the burden of IHD in Iran is a major public health problem that requires urgent attention. In addition to public health initiatives, there is a need for further research to more clearly recognize the underlying causes of IHD in Iran and to create more effective prevention and treatment strategies. This involves research on the impact of environmental pollution on IHD, as well as studies on the cost-effectiveness of different prevention and treatment interventions.
Acknowledgments
We acknowledge the hard work of the staff from the Institute for Health Metrics and Evaluation and their collaborators who prepared these publicly available data. In addition, we thank the Social Determinants of Health Research Center at the Shahid Beheshti University of Medical Sciences, Tehran (Iran) for their support. The current study, which used publicly available data, only indicates the opinions of its authors.
Funding
The current study was supported by the Shahid Beheshti University of Medical Sciences, Tehran, Iran (Grant No. 43003938). Furthermore, the GBD study was financed by the Bill and Melinda Gates Foundation, which was not involved in any way in the preparation of this manuscript
Data availability statement
The data reported in this study are all publicly available.
Ethical approval
The present study was approved by the Ethics Committee of the Shahid Beheshti University of Medical Sciences, Tehran, Iran (Ethics code: IR.SBMU.RETECH.REC.1401.689).
Consent for publication
Not applicable.
Conflict of interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary files
Supplementary file contains Tables S1-S3 and Figures S1-S8.
(pdf)
References
- Jensen RV, Hjortbak MV, Bøtker HE. Ischemic heart disease: an update. Semin Nucl Med 2020; 50(3):195-207. doi: 10.1053/j.semnuclmed.2020.02.007 [Crossref] [ Google Scholar]
- Vollmer-Conna U, Cvejic E, Granville Smith I, Hadzi-Pavlovic D, Parker G. Characterising acute coronary syndrome-associated depression: let the data speak. Brain Behav Immun 2015; 48:19-28. doi: 10.1016/j.bbi.2015.03.001 [Crossref] [ Google Scholar]
- Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014; 129(25 Suppl 2):S49-73. doi: 10.1161/01.cir.0000437741.48606.98 [Crossref] [ Google Scholar]
- Dai H, Much AA, Maor E, Asher E, Younis A, Xu Y. Global, regional, and national burden of ischaemic heart disease and its attributable risk factors, 1990-2017: results from the Global Burden of Disease Study 2017. Eur Heart J Qual Care Clin Outcomes 2022; 8(1):50-60. doi: 10.1093/ehjqcco/qcaa076 [Crossref] [ Google Scholar]
- Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM. Global burden of cardiovascular diseases and risk factors, 1990-2019: update from the GBD 2019 study. J Am Coll Cardiol 2020; 76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010 [Crossref] [ Google Scholar]
- Maracy MR, Isfahani MT, Kelishadi R, Ghasemian A, Sharifi F, Shabani R. Burden of ischemic heart diseases in Iran, 1990-2010: findings from the Global Burden of Disease Study 2010. J Res Med Sci 2015; 20(11):1077-83. doi: 10.4103/1735-1995.172832 [Crossref] [ Google Scholar]
- Sarrafzadegan N, Mohammmadifard N. Cardiovascular disease in Iran in the last 40 years: prevalence, mortality, morbidity, challenges and strategies for cardiovascular prevention. Arch Iran Med 2019; 22(4):204-10. [ Google Scholar]
- Khan MA, Hashim MJ, Mustafa H, Baniyas MY, Al Suwaidi S, AlKatheeri R. Global epidemiology of ischemic heart disease: results from the Global Burden of Disease Study. Cureus 2020; 12(7):e9349. doi: 10.7759/cureus.9349 [Crossref] [ Google Scholar]
- Murray CJL, Aravkin AY, Zheng P, Abbafati C, Abbas KM, Abbasi-Kangevari M. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020; 396(10258):1223-49. doi: 10.1016/s0140-6736(20)30752-2 [Crossref] [ Google Scholar]
- Wang H, Abbas KM, Abbasifard M, Abbasi-Kangevari M, Abbastabar H, Abd-Allah F. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet 2020; 396(10258):1160-203. doi: 10.1016/s0140-6736(20)30977-6 [Crossref] [ Google Scholar]
- Baeradeh N, Ghoddusi Johari M, Moftakhar L, Rezaeianzadeh R, Hosseini SV, Rezaianzadeh A. The prevalence and predictors of cardiovascular diseases in Kherameh cohort study: a population-based study on 10,663 people in southern Iran. BMC Cardiovasc Disord 2022; 22(1):244. doi: 10.1186/s12872-022-02683-w [Crossref] [ Google Scholar]
- Maleki A, Ghanavati R, Montazeri M, Forughi S, Nabatchi B. Prevalence of coronary artery disease and the associated risk factors in the adult population of Borujerd city, Iran. J Tehran Heart Cent 2019; 14(1):1-5. [ Google Scholar]
- Gaziano TA, Bitton A, Anand S, Abrahams-Gessel S, Murphy A. Growing epidemic of coronary heart disease in low- and middle-income countries. Curr Probl Cardiol 2010; 35(2):72-115. doi: 10.1016/j.cpcardiol.2009.10.002 [Crossref] [ Google Scholar]
- Sadeghi M, Haghdoost AA, Bahrampour A, Dehghani M. Modeling the burden of cardiovascular diseases in Iran from 2005 to 2025: the impact of demographic changes. Iran J Public Health 2017; 46(4):506-16. [ Google Scholar]
- Darba S, Safaei N, Mahboub-Ahari A, Nosratnejad S, Alizadeh G, Ameri H. Direct and indirect costs associated with coronary artery (heart) disease in Tabriz, Iran. Risk Manag Healthc Policy 2020; 13:969-78. doi: 10.2147/rmhp.s261612 [Crossref] [ Google Scholar]
- Kengne AP, June-Rose McHiza Z, Amoah AG, Mbanya JC. Cardiovascular diseases and diabetes as economic and developmental challenges in Africa. Prog Cardiovasc Dis 2013; 56(3):302-13. doi: 10.1016/j.pcad.2013.10.011 [Crossref] [ Google Scholar]
- Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004; 364(9438):937-52. doi: 10.1016/s0140-6736(04)17018-9 [Crossref] [ Google Scholar]
- Djalalinia S, Saeedi Moghaddam S, Sheidaei A, Rezaei N, Naghibi Iravani SS, Modirian M. Patterns of obesity and overweight in the Iranian population: findings of STEPs 2016. Front Endocrinol (Lausanne) 2020; 11:42. doi: 10.3389/fendo.2020.00042 [Crossref] [ Google Scholar]
- Rahmani F, Asgari S, Khalili D, Habibi Moeini AS, Tohidi M, Azizi F. National trends in cardiovascular health metrics among Iranian adults using results of three cross-sectional STEPwise approaches to surveillance surveys. Sci Rep 2021; 11(1):58. doi: 10.1038/s41598-020-79322-x [Crossref] [ Google Scholar]
- Sarebanhassanabadi M, Shahriari Kalantari M, Boffetta P, Beiki O, Pakseresht M, Sarrafzadegan N. Dietary habits and the 10-year risk of overweight and obesity in urban adult population: a cohort study predicated on Yazd Healthy Heart Project. Diabetes Metab Syndr 2020; 14(5):1391-7. doi: 10.1016/j.dsx.2020.07.024 [Crossref] [ Google Scholar]
- Moradi-Lakeh M, Vosoogh-Moghaddam A. Health sector evolution plan in Iran; equity and sustainability concerns. Int J Health Policy Manag 2015; 4(10):637-40. doi: 10.15171/ijhpm.2015.160 [Crossref] [ Google Scholar]
- Abdi Z, Hsu J, Ahmadnezhad E, Majdzadeh R, Harirchi I. An analysis of financial protection before and after the Iranian Health Transformation Plan. East Mediterr Health J 2020; 26(9):1025-33. doi: 10.26719/emhj.19.026 [Crossref] [ Google Scholar]
- Arab-Zozani M, Pezeshki MZ, Khodayari-Zarnaq R, Janati A. Inappropriate rate of admission and hospitalization in the Iranian hospitals: a systematic review and meta-analysis. Value Health Reg Issues 2020; 21:105-12. doi: 10.1016/j.vhri.2019.07.011 [Crossref] [ Google Scholar]
- Olyaeemanesh A, Behzadifar M, Mousavinejhad N, Behzadifar M, Heydarvand S, Azari S. Iran’s health system transformation plan: a SWOT analysis. Med J Islam Repub Iran 2018; 32:39. doi: 10.14196/mjiri.32.39 [Crossref] [ Google Scholar]
- Tabari-Khomeiran R, Delavari S, Rezaei S, Homaie Rad E, Shahmoradi M. The effect of Iranian health system reform plan on payments and costs of coronary artery bypass surgery in private hospitals of Iran. Int J Hum Rights Healthc 2019; 12(3):208-14. doi: 10.1108/ijhrh-07-2018-0047 [Crossref] [ Google Scholar]
- Alipour V, Zandian H, Yazdi-Feyzabadi V, Avesta L, Zahirian Moghadam T. Economic burden of cardiovascular diseases before and after Iran’s health transformation plan: evidence from a referral hospital of Iran. Cost Eff Resour Alloc 2021; 19(1):1. doi: 10.1186/s12962-020-00250-8 [Crossref] [ Google Scholar]
- Sarrafzadegan N, Sadri G, Malek Afzali H, Baghaei M, Mohammadi Fard N, Shahrokhi S. Isfahan Healthy Heart Programme: a comprehensive integrated community-based programme for cardiovascular disease prevention and control Design, methods and initial experience. Acta Cardiol 2003; 58(4):309-20. doi: 10.2143/ac.58.4.2005288 [Crossref] [ Google Scholar]
- Sarrafzadegan N, Laatikainen T, Mohammadifard N, Fadhel I, Yach D, Puska P. “Isfahan Healthy Heart Program”: a practical model of implementation in a developing country. Prog Prev Med 2018; 3(3):e0014. doi: 10.1097/pp9.0000000000000014 [Crossref] [ Google Scholar]