Int J Aging. 2024;2:e26.
doi: 10.34172/ija.2024.e26
Original Article
Design and Development of a Participatory Intervention Plan for Aging Promotion
Mina Alipour Niaz 1, *  , Tavakol Aghayari Hir 1, Mohammad Bagher Alizadeh Aghdam 1, Babak Akbari Sharghi 2, Katayoun Najarian 3
, Tavakol Aghayari Hir 1, Mohammad Bagher Alizadeh Aghdam 1, Babak Akbari Sharghi 2, Katayoun Najarian 3
Author information:
1Social Sciences Department, Faculty of Law and Social Sciences, University of Tabriz, Tabriz, Iran
2Elderly Visiting and Care Center (Sepideh), East Azerbaijan Welfare Department, Tabriz, Iran
3Elderly Rehabilitation Daily Center (Mehregan), East Azerbaijan Welfare Department, Tabriz, Iran
Abstract
Objectives:
To develop an active aging model through participatory interventions, empowering elderly individuals to take part in enhancing their physical and mental well-being. By fostering self-care and increasing awareness of aging health needs, the project sought to provide both theoretical and practical resources for promoting healthy aging.
Design:
This quasi-experimental study included two groups: an experimental group and a control group. To control for confounding variables, participants were fully matched across groups.
Setting(s):
Elderly rehabilitation centers in Tabriz, Iran.
Participants:
Fifty women aged 60–65 who were members of rehabilitation centers participated in this study over three months, during which they contributed to designing an aging promotion model.
Interventions:
Three-month promotional participatory intervention.
Outcome measures:
Income; Self-care awareness; Healthy & active aging; Quality of life.
Results:
Individuals in the experimental group created an intervention framework that enhanced their active aging and overall health. Post-test results indicated a significant improvement in active aging and general health, highlighting the intervention’s positive impact on the health and active aging of the experimental group.
Conclusions:
Recent studies underscore the critical role of social participation in promoting health in later life, fostering a new understanding of successful aging by emphasizing active aging, resilience, and similar concepts. The structure of the designed model enables participants to organize their activities and social interactions, enhancing their quality of life by addressing age-related challenges and promoting recovery
Keywords: Active aging, Community-based promotion of aging health
Copyright and License Information
© 2024 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
None.
Please cite this article as follows: Alipour Niaz M, Aghayari Hir T, Alizadeh Aghdam MB, Akbari Sharghi B, Najarian K. Design anddevelopment of a participatory intervention plan for aging promotion. Int J Aging. 2024;2:e26. doi: 10.34172/ija.2024.e26
Introduction
The world is always engaged in demographic changes. Recent technological and cultural developments have transformed the population pyramid of the world. This transformation, sometimes called “the silent revolution” and has been extensively considered a threat in terms of public health and economic costs named an aging global phenomenon. The growth rate of the elderly population is increasing, along with the decrease in the fertility rate and an increase in life expectancy, mutation of medical sciences, and health index promotion.
Demographists have appraised that the elderly population in five continents will grow twice and even more by 2050, so that 20% of the world’s population will be over the age of 65 years. In Asia, this growth will increase from 7.9% in 2015 to 18.8% in 2050. Similarly, we will witness the growth at the same rate in Europe, Africa, Latin and North America, and Oceania. This growing process has the fastest rise in East Asia, east South Asia, Latin America, and the Caribbean, so that the world’s mostly old population is now residing in east Asia and east South Asia (260 million). It is estimated that one person from each three (80% of older adults) will be living in the mentioned areas and low-to-middle-income countries. Iran, as an Asian country, has similar conditions as well. Although Iran is currently one of the youngest populations in the world, the plummet in the birth rate, the elevation in life expectancy, and the high percentage of the middle population indicate the rapid aging of Iran’s population in the coming years.1
The United Nations Population Fund (2021) reported that the annually growing percentage of the population of Iran will decline to 1.2% in 2026 and then will face a negative rise. For this reason, the wide part of the population pyramid will jump up to the elderly part.2
Now the important point is that the population of Iran is rapidly aging, and aging drops people’s health and increases the burden of diseases, so it is associated with chronic and costly diseases. Many older adults live with chronic illnesses, including heart disease, cancer, diabetes, infectious diseases, and dementia. The prevalence of chronic diseases presents unique public health challenges. Although there is no clear picture of the prevalence of chronic diseases among the elderly in Iran, the danger bell for the country has been called.3
These conditions can lower the quality of life of older adults and contribute to the leading causes of death among them. Thus, they need care and support to maintain and even improve their health.
However, similar to many developing countries, Iran lacks policies to address the elderly’s needs, such as income, healthcare, and housing, and the country’s social institutions are slow to respond to demographic changes. The increase of the elderly population is one of the most challenging issues in Iran and in the field of world health, and making the right policies about them is a global common concern.
In recent years, health experts have agreed that the primary care of the elderly should be changed from horizontal and vertical care systems based on the community to person- and goal-oriented manners2. In horizontal systems, services are delivered through publicly mandated and financed health systems commonly referred to as comprehensive primary healthcare or universal health coverage. The vertical systems of health services imply a selective targeting of specific interventions not fully integrated into health systems, often linked with particular interests of the funding entity.4
Person-centered care retrieved from the World Health Organization’s definition of integrated service delivery lies in the health field based on the aim that “integrated care should be centered on the needs of individuals, their families, and communities”5. Person-centered care is also argued to be a means to improve the quality of care. Goal-oriented techniques are moving to a model that focuses on problem-solving strategies. This approach enables the four key components of people-driven care, namely, empowerment, engagement, co-production, and co-design.5 This point shows the necessity of people’s participation and involvement in their life affairs. The literature of the Ottawa Charter, which was adopted in Canada in 1986, is derived from this important point. According to this charter, health promotion, which is the process of empowering persons to increase control over their health and improve it, should simultaneously reduce risk factors and increase protective factors. “Self-care” as an important protective factor in aging health promotion will be impossible without their participation. In addition, in this charter, a healthy person is introduced as someone who is not only physically and mentally healthy but also socially active, plays a role in his/her environment, and takes charge of his/her own destiny. Actually, a healthy person is able to function peacefully and effectively in society and live a socially and economically productive, satisfied life. From this definition, it can be understood that health is not a matter of life but of life itself. Based on this definition and according to the activity theory of aging 6 which posits that older adults need to stay active, resist role losses, and compensate for lost activities with new roles, it is desirable to maintain as many middle-aged activities as possible in late life. In old age, the cells in the body begin to degenerate, which leads to a decrease in their function. This degeneration is a normal function, and no medicine can slow down this degeneration. What matters is how the person sees herself/himself as an elder. A healthy elder who can look after herself or himself is a great support to the rest. From the view of aging psychology, a person’s self‐concept is validated through participation in roles that are characteristic of middle age.7
In addition, in sociological theories of aging, the “elderly participation concept”, linking approaches are concerned with the interplay between meaning and social structures (i.e., social life’s patterned quality).8 formalization of his continuity theory, in which he brings together systems theory and the concept of agency, is one example of this approach in gerontology. It implies that the agency (people) in connection with the system (society) finds life as it deserves. Salma Omer9 believes that the process of participation, intervention, and control of people results in determining what constitutes a superior life from the viewpoint of the people themselves. The “community-based approach” has matured from within these linked theories of system and agency based on social participation. In recent decades, this approach has been the focus of interventions to empower the human population in a world that is moving toward “active aging” with increasing speed.
Active aging is a multidimensional concept, embracing physical and cognitive health, positive affect and control, as well as social relationships and engagement. It is the process of optimizing opportunities for health, participation, and security in order to enhance the quality of life as people age. It is one strategy to manage the increasing rate of the old population and its complications. Active aging programs have been implemented in different countries, including a training program on active aging in Portugal, the active aging program in nursing homes in Spain, the Green Care program in Italy, a national action plan for active and healthy aging in Scotland, and the Vital Aging program in Mexico. The other related programs are intergenerational programs to promote active aging in the UK, “I am active” in Mexico, Opportunities for the Elderly Project, Elder Academy Scheme and Neighborhood Active Aging Project in Hong Kong, and promoting active aging through university programs in Spain. Nevertheless, the difference in active aging indicators in societies is dependent on the capacity of the older population in societies and the provision of age-friendly environments.
Alan Walker and Christian Aspalter10, as they have paltered at in their book as “Active Ageing in Asia”, have focused on the experiences of East Asian societies where active ageing programs have been implemented in 2017. They present a thorough analysis of the concept of active ageing and its potential and problems of implementations in different stages of development in East Asia. They also emphasize the difference in active aging indicators in different Asian societies.10 Now, we may ask whether participation in self-care is nice, essential, or at least a priority. Research shows that individuals who have more knowledge, skills, and confidence to manage their health and healthcare are more likely to engage in positive health behaviors and have better health outcomes. People are less likely to use horizontal or vertical services when they play a more collaborative role in managing their health and care. They are also more likely to stick to their treatment plans and take their medicine correctly. Moreover, they are more satisfied with their health and are more likely to choose treatments based on their values and preferences rather than those of their clinicians.
Therefore, social medicine believes in prioritizing active aging and participation in healthcare programs, understanding that global sustainable development and universal healthcare will not be attainable otherwise.
Considering the importance of this issue, this study was performed to find the answer to this question: “What is the model of participatory intervention developed on the promotion of active aging among the elderly of the statistical society and how effective is it?”
Methods
Procedure
The research method was a “quasi-experimental” type of intervention, before–after study with a non-random control group.
Participants
They included 60‒65 year old women of Tabriz receiving services from daily rehabilitation centers.
Sampling
The sample size included 50 elderly individuals who were selected voluntarily and non-randomly.
Data Gathering Tools
Collection tools included the native scale of the “Active Aging Index”, standardized by Mohammady et al,11 the General Health Scale of the Elderly (GHQ-28) by Goldberg in 1972,12 normed by Malakouti et al in iran(2007), and a researcher-made checklist, including demographic information. The reliability of each of the three questionnaires was calculated to be above 0.96.
Analysis Techniques
The data were analyzed using SPSS and statistical methods of bivariate covariance and dependent t test.
Intervention
Two daily rehabilitation centers for the elderly were selected after coordinating with the Tabriz Welfare Organization. Then, a clarification meeting of the plan was held, and 25 people from the center were separated into the experimental and control groups, completely voluntary. To generalize the findings to society, the samples were placed in groups to have maximum homogeneity.The members of the experimental group participated in the intervention process for 12 sessions of 4 hours and a total of 48 hours. They themselves decided about the days and hours of the meetings. In the first three parts, the role of the facilitator was more colorful because he taught the routine skills of community-based interventions. To implement what was in the researcher’s mind, a protocol was made by her. The important aim of making protocols before the intervention was to follow a regular structure involving Apportionment of a certain time to educational, experimental, and dialog categories. In the first session, before starting the program, the goal was posted on the wall as “a community of people committed to living actively, building friendships, and feeling energized and empowered”. Further, a mailbox was prepared and attached to the wall. It was explained to the participants that they have individual box. At the end of each session, they can put the letters they wrote to their friends in their boxes and check them to pick up if they have received one. The participants could write down their good or bad feelings toward each other, the presenter, and even the content of the program by committing to changes in their mood and put them in the box. At the beginning of the first session, five people were randomly asked to name their favorite flower. Then, five groups were formed with the same names in order to group discussion and brainstorming, and people were randomly assigned to them. Subsequently, each group made a symbol for themselves based on the name of the group and used it in their round table until the end of the intervention period. The next step was to compile the rules and regulations of the course, which were determined through the participants’ thoughts and recorded on cardboard and installed on the wall. The rules remained until the end of the period. For the situation analysis and needs assessment activities, the groups presented their opinions based on brainstorming and consultation with each other, and at the end of the allotted time, the group’s secretary read them. All the points that were raised were summarized by the presenter and recorded on cardboard. The cardboards were installed on the wall to be visible to everyone. Necessary trainings on how to hold meetings and planning were provided. From the fourth session onwards, the participants themselves took control of the sessions. In fact, they were the decision-makers and program managers. The implementation steps are presented in Table 1.
Table 1.
Action Chart of the Intervention Process
|
Object
|
Actor
|
Action
|
| Initial designing |
Researcher |
- Reading texts
- Determining variables and indicators
- Writing guidelines
- Choosing training subjects |
| Training |
Participants/researcher |
- Doing needs assessment
- Prioritizing training needs
- Holding training time |
| Planning |
Participants |
- Doing situation analysis
- Drawing the profile of the community
- Drawing the problem tree
- Preparing health promotion program charts |
| Implementing |
Participants |
Implementing the plan |
| Evaluating |
Participants |
Performing pre- and post-test |
Drawing the problem tree was one of the most important activities of the groups. This is because the model (the operational plan) should be designed based on the problems raised and proposed solutions. Each of the groups drew the mentioned tree and even decorated it. This part was one of the most exciting parts of the program based on the participants’ own words. Basic problems were identified, duplicate problems were removed, and finally, the main tree was drawn and exposed. The results of the needs assessment are depicted in Figure 1.
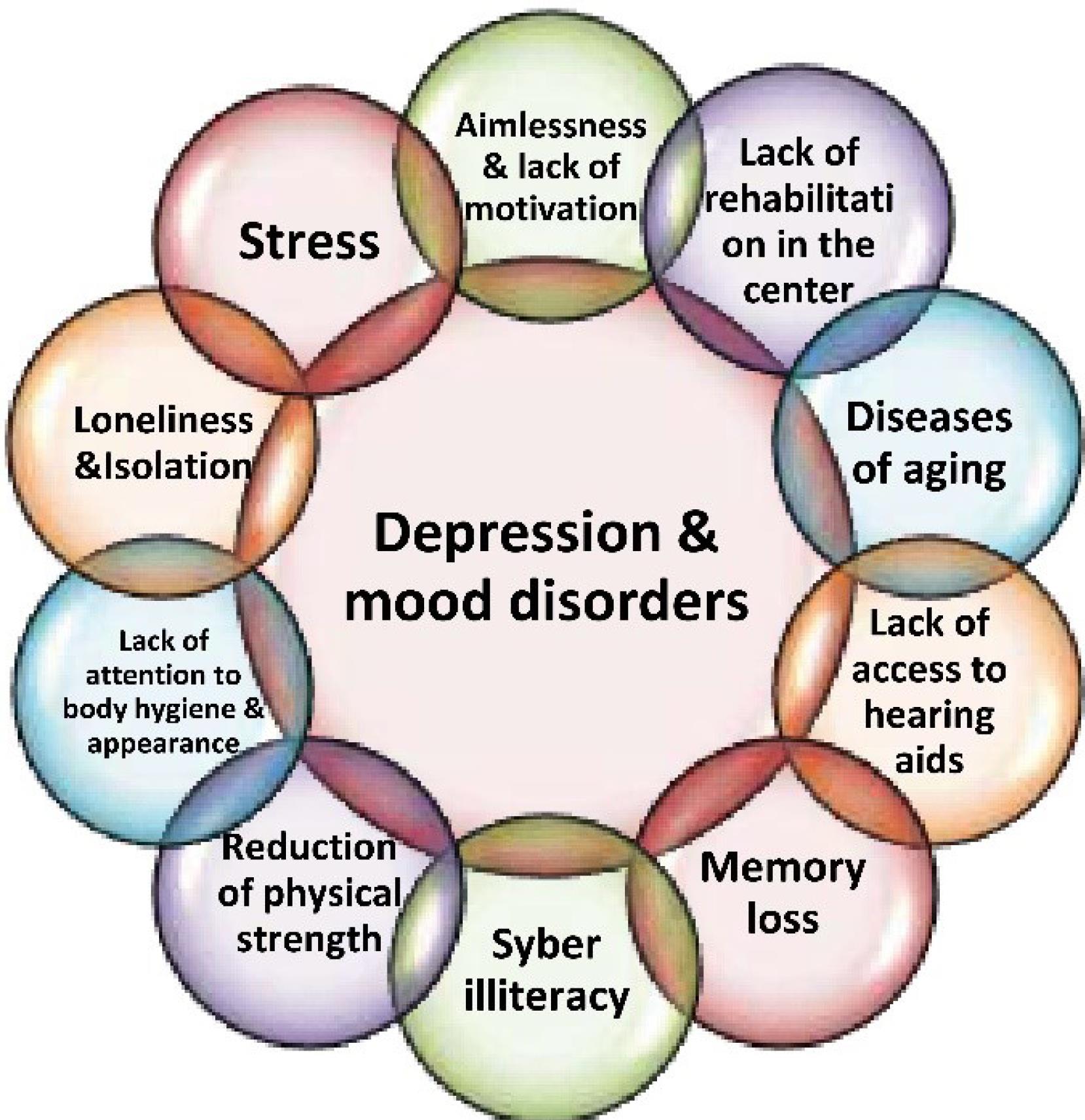
Figure 1.
Results of Needs Assessment
.
Results of Needs Assessment
In the planning stage, the goals were defined with the participation of the members themselves, and the relevant activities were defined for the realization of each of them. The designed model was focused on self-care (the cognitive dimension of health promotion), stimulating its emotional and behavioral dimensions, as well as increasing resilience, self-efficacy, and collective spirit and promoting a healthy lifestyle. The trainings and activities that were performed to solve each of the needs are summarized in Table 2.
Table 2.
Action Chart of the Intervention Based on Needs Assessment
|
Needs
|
Trainings
|
Activities
|
| Depression and mood disorders |
- Symptoms and complications of depression; prevention and treatment
- Resilience increase techniques
- Aggression against techniques
- Flexibility techniques |
- Meditation
- Relaxation
- Visualization
- Deep breathing
- Memory writing
- Poetry reading and storytelling
- Skill games |
| Stress |
- Stress sources
- Stress management techniques
- Mental obsession
- Replacement of positive thoughts with negative thought techniques
- Commitment and sustainability |
| Reduction of physical strength |
- Physical exercises for the elderly
- Suitable diet for the elderly
- How to prepare food
- How to take vitamins and supplements |
- Chair yoga
- Dancing
- Blood sugar and blood pressure control
- Water drinking
- Vitamin trampy |
| Lack of attention to body hygiene and appearance |
- Hygiene and controlling infectious diseases
- Hygiene of mouth and tooth
- Skin and hair care
- The role of beauty in mental welfare |
|
| Diseases of aging |
- Diabetes
- Blood pressure
- Blood fat
- Obesity
- Cardiovascular diseases
- Fatty liver
- Heart attack and stork
- Infectious diseases
- Pulmonary diseases
- Hearing loss
- Eyes care
- Constipation and digestive diseases
- Urinary tract problems
- Uterus and appendages
- Osteoporosis
- Falling
- Dementia and Alzheimer’s
- Body scan and principles of self-care |
|
| Aimlessness and lack of motivation |
- Self-awareness skills
- Successful aging in the world with tangible examples
- Goal setting and daily plans |
- Painting
- Cooking competition
- Swimming pool plans
- Craft making |
| Cyber illiteracy |
- Teaching how to use social networks and meeting |
|
| Loneliness and isolation |
- Social communication and networking
- Meeting programs with community friends |
|
| Memory loss |
- Memory loss techniques
- Reminder techniques |
- Strengthening of the mind and
memory techniques |
| Lack of access to hearing aids |
|
- Provision of 2 hearing aids |
| Lack of rehabilitation in the center |
|
- Preparation of pressure gauge |
The needs listed based on priority. During the intervention, participants were ordered to daily practice everything they learned at home. Participants received sheets as self-control memories to record practices. The facilitator collected them at the end of the class and returned them with comments in the next section. Physical, mental, and breezy activities were performed in each section, and the researcher’s assistant team including a doctor, a nurse, a psychologist, a yoga coach, and an occupational therapist, were training them. Vacation in the last séance, cooking, pastry and desert competition, body health checkups, thanksgiving, and game-based learning were key activities. As a general rule for voluntary participatory models, as a general rule for voluntary participatory models, participants made a friendship network that will continue for at least one year. In addition to the monitoring of the process during the intervention, the evaluation was conducted by comparing pre- and post-test data in order to explain the effectiveness of the designed model.
Results
In the descriptive analysis of demographic data, the high homogeneity of the participants in both groups was evident. The average age of the participants was 63 years, and most of them (in both groups) were married. Most participants in both groups had a low level of literacy, were housewives, and lived with their spouses in private houses. In addition, they had a monthly income below 90 million rails. The average number of children in each group was between one and three children. Less than half of the participants were healthy at the time. Compared to the last five years, 36% of the experimental group and 28% of the control group had become ill. The average of the socio-economic index (which was obtained by calculating the average standard scores of items related to the educational status, employment status, residence status, source of livelihood, and amount of income) was reported as 0.963 in the scale (0–100), indicating the equality of the socio-economic state of both groups.
The averages obtained for the total index of active aging and general health confirmed the effect of the intervention on the scores of the mentioned variables in the experimental group. Despite the overall average, the active aging index in the experimental group increased from 3.262 in the pre-test to 3.694 in the post-test, while in the control group, a noticeable decrease was found in the active aging score; in other words, the average score of the mentioned index decreased from 2.580 to 2.517. As regards general health and quality of life, an increasing trend was observed in the experimental group, whereas a decreasing pattern was found in the control group (due to the nature of biological aging). A dependent t test was used to compare the pre-test and post-test scores of the groups. The difference in the averages of active aging in the experimental group was reported as -6.287 (P value = 0.00). It can be concluded that there was a statistically significant improvement in the level of active aging in the experimental group after the intervention with 0.431 units. However, considering t = 1.432 and a significant level of 0.165, such an improvement was not observed in the control group. The significance level of 0.00 indicates that general health has improved by 0.609 unit in the experimental group as a result of the intervention. In terms of general health, the general health score of the elderly in the control group significantly decreased after the intervention (t = 3.165, P = 0.04). To test the research hypothesis, covariance analysis was used in accordance with the necessary assumptions.
According to the information in Table 3, the quantity of F regarding the total index of active aging, taking into account belonging to the experimental group, was calculated to be 151.78, and the significance level was smaller than 0.05; therefore, belonging to the experimental group had a significant effect on Active aging and could increase it by 0.76 unit.
Table 3.
Results of Covariance Analysis of Active Aging and General Health
|
|
Sucre of Variance
|
Sum of Square
|
df.
|
Mean of Square
|
F
|
Sig.
|
Eta Squared
|
| Active aging |
Experimental group |
5.34 |
1 |
5.034 |
151.783
112.407 |
0.000
0.000 |
0.764
0.705 |
| Pre-test |
3.928 |
1 |
3.928 |
| Error |
1.643 |
1 |
0.35 |
| General health |
Experimental group |
10.451 |
1 |
10.451 |
486.545
107.925 |
0.000
0.000 |
0.912
0.697 |
| Pre-test |
2.318 |
1 |
2.318 |
| Error |
1.010 |
47 |
0.044 |
Based on the covariance test results, the amount of F for general health and the significance level were 486.54 and 0.00, respectively. Moreover, the eta squared indicates that the post-test score of the experimental group has expanded by 0-912 units, demonstrating a considerably high level of efficacy.
According to the results obtained from the research hypothec test, a model that is designed in a community-based method is influential in increasing general health and improving active aging.5
Discussion
In the last 4 decades, demographic and epidemiological studies have proposed new models for the well-being of the elderly. Coping/resilience theories, participatory rehabilitation based on social interaction and social participation, self-care lifestyle theory and finally the community-based approach to aging try to increase life expectancy by reducing and adjusting the years of life lost due to disability, premature mortality, and disabilities. In addition; one of the important functions of participating in community-based programs is to access social networks, which is also a determinant of mental and social well-being. With these descriptions, societies have designed and implemented programs to promote the health of the elderly, each of which has had different results, and various models that help to have a peaceful life in middle age and adulthood have been proposed. The present study was conducted in line with these results, and its achievements were based on confirming the effectiveness of the participatory model of aging health on the post-test score of active aging and general health of the experimental group, which indicates the influential role of the target community itself in increasing and improving health and self-care, social interactions, and other components of healthy aging.
Conclusions
This study analyzed the effectiveness of an intervention program aiming at improving active aging through self-determined activities in a group of community older adults receiving empowerment services from daily rehabilitation centers for the elderly. Actually, this research was performed to promote active aging with the participation of the target community. While the participants were benefiting from empowerment services, the goal was to know whether the model prescribed by the experts was more effective in their health and activity or the model they designed themselves. The results of the analysis confirmed the significant effect of the social-oriented intervention (as participating in pattern designing) on the scales of active aging and general health in the experimental group. On both scales, a significant increase was observed in post-test scores. Therefore, both the active aging index and general health improved as a result of the intervention. In other words, the model designed by the participants was more effective than the systematic model. The results of this survey conform to those of studies conducted by Ahmadi et al,13 comparing the quality of life of active and non-active old women with an emphasis on physical exercise, and Shiani,M & Zaare,H,14 investigating the effectiveness of community-based programs on elderly mental wellbeing. Likewise, the findings of this study corroborate those of studies performed by Noor,15 Malaysian Older Women Empowerment Program Using a Community-Based Approach and Oyama et al,16 focusing on community-based prevention for suicide in the elderly by depression screening and mental community follow-ups. Other studies by Caprara et al,17 examining active aging promotion by the vital aging program, and Dumitrache et al,18 promoting active aging in rural settings using an intervention program implemented in Orense, Spain, demonstrated results that match those of the present study. Numerous programs have been developed in the gerontological context, especially active aging, that involve maintaining and improving cognitive functioning, or at preserving a good physical status. Meanwhile, only a limited number of interventions include other social aspects, such as participation in self-care planning. Despite the similarities, which are mostly focused on the social field, namely, communication outside the home and the network of relationships, what makes this study different is the definition and application of the community-based intervention for the promotion of the elderly, which is less common in the Iranian context (society). The synthesis of physical, emotional, and financial costs of providing medical and care services to the population can threaten the sustainability of healthcare and social welfare programs. These challenges include not only individual conditions but also barriers and facilitators in social and physical environments, which are often conceptualized as micro-, mid-, and macro-environmental factors in the socio-ecological model. when Lawton emphasized the value of preventive social action aiming to overcoming environmental challenges in late life The concept of activism proposed in collective categories. In recent gerontology literature, much attention has been paid to the value of social capital as a personal and social potent resource.19 The research results revealed that many successful interventions in the field of aging have used the participation model and behavioral change theories to inform program design and implementation.20 Although the results indicate that the social participation of the elderly plays a key role in the success of interventions related to aging, the literature in this field of studies is dominated by person-centered approaches. Therefore, future research should focus more on evaluating social environment-focused interventions and develop a comprehensive framework that combines both personal- and social approaches to healthy aging. The findings of this review will help inform policymakers in developing and implementing relevant evidence-based local policies and strategies to move toward creating an age-friendly social environment.21
This research, similar to other studies, especially in the field of humanities and social sciences, has faced limitations, such as the single-sex nature of the participants (users of the services of the centers were only females) and age sensitivity to the implementation of some tactics. In addition, this study was conducted in Corona pandemic conditions. However, in all cases, efforts have been made to keep the impact of such restrictions on the results of the research at the minimum level, with suggested measures based on the research literature. Considering the significant effect of the designed model on active aging, it can be suggested that the organizations or institutions responsible for the health of the elderly use community-oriented intervention in the form of a suitable intervention package.
Acknowledgments
Thanks to Professor Amir Hassan Rafiei, the founder of the community-centered approach in Iran. We are grateful to the owners of the two centers, Mehregan and Hamaraz. We are grateful for the sincere cooperation of the elderly women who participated in the research.
Author contributions
Conceptualization: Mina Alipouri Niaz, Tavakol Aghayari Hir.
Formal analysis: Mina Alipouri Niaz, Tavakol Aghayari Hir.
Investigation: Mina Alipouri Niaz, Tavakol Aghayari Hir, Mohammed Bagher Alizadeh Aghdam, Babak Akbari Sharghi, Katayoun Najjarian.
Methodology: Mina Alipouri Niaz, Mohammed Bagher Alizadeh Aghdam.
Project administration: Tavakol Aghayari Hir, Mohammed Bagher Alizadeh Aghdam.
Resources: Babak Akbari Sharghi, Katayoun Najjarian.
Software: Mina Alipouri Niaz.
Supervision: Tavakol Aghayari Hir.
Validation: Mina Alipouri Niaz, Tavakol Aghayari Hir.
Visualization: Babak Akbari Sharghi, Katayoun Najjarian.
Writing–original draft: Mina Alipouri Niaz.
Writing–review & editing: Mina Alipouri Niaz, Tavakol Aghayari Hir, Mohammed Bagher Alizadeh Aghdam, Babak Akbari Sharghi, Katayoun Najjarian.
Data availability statement
Data will be available by contacting corresponding author.
Ethical approval
This study is the result of an approved research project from Tabriz University of with ethics code
IR.TABRIZU.REC.1403. 039.
Consent for publication
The authors express their consent to publish this article in International Journal of Aging.
Conflict of interests
The authors declare no conflict of interests
References
- Özkan Ş. Health services and policies for elderly health in Turkey. In: Health Sciences Research in the Globalizing World 2018;129(196.8):1072. Sofia: St. Kliment Ohridski University Press; 2018.
- Iliffe S. Community-based interventions for older people with complex needs: time to think again?. Age Ageing 2016; 45(1):2-3. doi: 10.1093/ageing/afv185 [Crossref] [ Google Scholar]
- Sakala JJ, Chimatiro CS, Salima R, Kapachika A, Kalepa J, Stones W. The integration of vertical and horizontal programmes for health systems strengthening in Malawi: a case study. Malawi Med J 2022; 34(3):206-12. doi: 10.4314/mmj.v34i3.11 [Crossref] [ Google Scholar]
- Steele Gray C, Grudniewicz A, Armas A, Mold J, Im J, Boeckxstaens P. Goal-oriented care: a catalyst for person-centred system integration. Int J Integr Care 2020; 20(4):8. doi: 10.5334/ijic.5520 [Crossref] [ Google Scholar]
- Anselmi L, Lagarde M, Hanson K. Going beyond horizontal equity: an analysis of health expenditure allocation across geographic areas in Mozambique. Soc Sci Med 2015; 130:216-24. doi: 10.1016/j.socscimed.2015.02.012 [Crossref] [ Google Scholar]
- Havighurst RJ, Albrecht R. Older People. London: Longmans, Green; 1953.
- Mutchler J, Coyle C, Velasco Roldán N, Watanabe P, Woods C, Rivera L, et al. Aging Strong for All: Examining Aging Equity in the City of Boston. University of Massachusetts Boston; 2020.
- Ashley-Smith J. Risk Assessment for Object Conservation. Routledge; 2013.
- Omer S. Women’s work in community development-its significance and impediments. Community Development Bulletin 1961; 12(4):133-8. [ Google Scholar]
- Walker A, Aspalter C. Active Ageing in Asia. London: Routledge; 2015.
- Mohammadi E, Allahyari T, Darvishpoor Kakhaki A, Saraei H. Determining psychometric properties of Iranian active aging measurement instrument. Iran J Ageing 2018; 12(4):414-29. doi: 10.21859/sija.12.4.414 [Crossref] [ Google Scholar]
- Malakouti SK, Fatollahi P, Mirabzadeh A, Zandi T. Reliability, validity and factor structure of the GHQ-28 used among elderly Iranians. Int Psychogeriatr 2007; 19(4):623-34. doi: 10.1017/s1041610206004522 [Crossref] [ Google Scholar]
- Ahmadi M, Noudehi M, Esmaeili M, Sadrollahi A. Comparing the quality of life between active and non-active elderly women with an emphasis on physical activity. Iran J Ageing 2017; 12(3):262-75. doi: 10.21859/sija.12.3.262 [Crossref] [ Google Scholar]
- Shiani M, Zare H. The effectiveness of community-based programs on older adult’s subjective well-being. Iran J Ageing 2013; 8(2):16-29. [ Google Scholar]
- Noor NM, Alwi A, Mohd MI. Development and effectiveness of a community-based intervention program for elderly women in Malaysia. J Behav Sci 2016; 11(2):1-20. [ Google Scholar]
- Oyama H, Koida J, Sakashita T, Kudo K. Community-based prevention for suicide in elderly by depression screening and follow-up. Community Ment Health J 2004; 40(3):249-63. doi: 10.1023/b:comh.0000026998.29212.17 [Crossref] [ Google Scholar]
- Caprara M, Molina M, Schettini R, Santacreu M, Orosa T, Mendoza-Núñez VM. Active aging promotion: results from the vital aging program. Curr Gerontol Geriatr Res 2013; 2013:817813. doi: 10.1155/2013/817813 [Crossref] [ Google Scholar]
- Dumitrache CG, Rubio L, Bedoya I, Rubio-Herrera R. Promoting active aging in rural settings: an intervention program implemented in Orense, Spain. Univ Psychol 2017; 16(3):112-23. doi: 10.11144/Javeriana.upsy16-3.paar [Crossref] [ Google Scholar]
- Bengtson VL, Settersten R Jr. Handbook of Theories of Aging. Springer Publishing Company; 2016.
- World Health Organization (WHO). Decade of Healthy Ageing: Baseline Report. WHO; 2021.
- Hjelle EG, Bragstad LK, Zucknick M, Kirkevold M, Thommessen B, Sveen U. The General Health Questionnaire-28 (GHQ-28) as an outcome measurement in a randomized controlled trial in a Norwegian stroke population. BMC Psychol 2019; 7(1):18. doi: 10.1186/s40359-019-0293-0 [Crossref] [ Google Scholar]