Int J Aging. 2024;2:e25.
doi: 10.34172/ija.2024.e25
Original Article
Determining the Predictive Value of Shock Index, Reverse Shock Index, and Modified Shock Index in Hospital Outcome of Gastrointestinal Bleeding in Elderly Patients
Zahra Vandrajabpour 1  , Seyedpouya Paknezhad 1, *
, Seyedpouya Paknezhad 1, *  , Amir Ghaffarzad 1, Zahra Parsian 2, Hamidreza Mortezabagi 1, Aisan Akhgari 3
, Amir Ghaffarzad 1, Zahra Parsian 2, Hamidreza Mortezabagi 1, Aisan Akhgari 3 
Author information:
1Emergency and Trauma Care Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
2Clinical Fellow, Leeds Teaching Hospital, NHS Trust, Leeds, UK
3Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Objectives:
To investigate the predictive value of the shock index (SI), reverse shock index (RSI), and modified shock index (MSI) in determining the hospital outcomes of elderly patients with gastrointestinal bleeding (GIB).
Design:
A cross-sectional study.
Setting(s):
The study was carried out in Tabriz, East Azarbaijan, North-west Iran.
Participants:
The study included patients aged over 75 years who were presented with acute upper GIB.
Outcome measures:
Specificity, sensitivity, positive, and negative predictive values were calculated to assess the predictive capacity of these three indices in predicting mortality risk among patients as their in-hospital outcome.
Results:
Age distribution among the patients in this study did not follow a normal pattern. Regarding the predictive value of the SI, RSI, and MSI for patient outcomes, the sensitivity and specificity of these criteria were as follows: SI with 48.48% sensitivity and 86.84% specificity (95% CI: 79.23-92.44), RSI with 33.33% sensitivity and 92.04% specificity (95% CI: 85.42-96.29), and MSI with 30.30% sensitivity and 91.23% specificity (95% CI: 84.46-95.71).
Conclusions:
The findings of this study indicated that none of these criteria effectively predicted mortality in patients with GIB. However, SI, RSI, and MSI exhibited high specificity in predicting hospital outcomes for GIB patients, making them valuable tools for ruling out life-threatening conditions. However, due to their low sensitivity, they are less reliable for diagnostic purposes in determining the specific causes of GIB.
Keywords: Gastrointestinal bleeding, Shock index, Reverse shock index, Modified shock index
Copyright and License Information
© 2024 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
This article is funded by the research reward grant of Tabriz University of Medical Sciences. We thank emergency medicine research team of the Tabriz University of Medical Sciences for collaboration on conducting this study.
Please cite this article as follows: Vandrajabpour Z, Paknezhad S, Ghaffarzad A, Parsian Z, Mortezabagi H, Akhgari A. Determining the Predictive value of shock index, reverse shock index, and modified shock index in hospital outcome of gastrointestinal bleeding in elderly patients.Int J Aging. 2024;2: e25. doi: 10.34172/ija.2024.e25
Introduction
Gastrointestinal bleeding (GIB) is a common medical condition that often necessitates hospitalization, with a mortality rate of approximately 10%. While GIB is typically identified through symptoms such as hematemesis or bloody stools, some cases pose diagnostic challenges when patients present at the emergency room with atypical symptoms such as hypovolemia or perfusion disorders.1 Diagnosed as a medical emergency, GIB demands early evaluation and triage, particularly focusing on diagnosing critically ill patients with life-threatening hemodynamic disturbances and initiating appropriate resuscitation. Notably, the precise source of bleeding is not always readily discernible. For instance, approximately 15% of patients with severe hematochezia have upper gastrointestinal bleeding (UGIB), contrary to initial expectations of lower GIB.2 UGIB may manifest with a range of symptoms, including hematemesis, melena, or severe hematochezia. Prolonged bleeding, hypovolemia, and hemorrhagic shock contribute significantly to patient mortality.1 In a study by Stanley et al in 2010, 23% of patients required blood transfusions, while 14% necessitated surgical and endoscopic interventions.3
While previous research has explored various diagnostic parameters, including laboratory values, they can be cost-prohibitive, time-consuming, and challenging to apply in outpatient settings.4 Conversely, simpler parameters such as heart rate and arterial blood pressure have been identified as potential indicators of severe bleeding.5-7 Shock index (SI) is derived by dividing the initial heart rate by the arterial systolic blood pressure (SI = heart rate/systolic blood pressure). Modified shock index (MSI) is also defined as dividing the heart rate by mean arterial pressure (MSI = Heart rate/mean arterial pressure), and reverse shock index (RSI) is defined as the result of dividing arterial systolic pressure by heart rate (RSI = Systolic blood pressure/heart rate).8
This study focused on evaluating the predictive value of three easily assessable parameters, namely, SI, MSI, and RSI in predicting the outcome of GIB in hospitalized patients over 75 years old. Given their cost-effectiveness, these indices offer promise as valuable tools for assessing GIB outcomes.
Methods
Study Design
This prospective descriptive study aimed to assess the predictive value of SI, MSI, and RSI in elderly patients aged over 75 years with acute UGIB. It was conducted at Imam Reza Hospital’s emergency department, a general tertiary hospital in Tabriz, East Azarbaijan, north-west of Iran.
Patient Selection
We used a total population sampling, and all eligible patients were included in our study during 6 months. Patients meeting the following criteria were included in the study:
-
Age over 75 years
-
Diagnosis with acute UGIB
-
Presentation at the emergency department
-
Willingness to participate and provide informed consent
Patients who met any of the following criteria were excluded from the study:
-
Non-hospitalized patients
-
Patients who did not undergo endoscopy
-
Trauma-related cases
-
Patients with lower GIB
-
Referrals from other medical centers (due to primary treatment initiation)
-
Patients who declined to participate
-
Patients presented with cardiac arrest
-
Patients who leave the hospital against medical advice
Data Collection
After the approval of the Ethics Committee and obtaining informed consent, demographic information, including gender, age, and contact details was recorded. Additionally, data related to endoscopic interventions, endoscopy results (e.g., varicose veins, ulcers, malignancies, esophagitis, gastritis, Mallory-Weiss syndrome, and non-specific findings), surgical requirements and their types, intensive care unit (ICU) admissions, duration of hospitalization, packed cell transfusion needs, and discharge and mortality outcomes were collected. Furthermore, vital signs at the triage unit, including systolic and diastolic blood pressure, heart rate, and respiratory rate were documented for each patient.
Calculation of Indices
SI at the triage unit, MSI at the triage unit, and RSI at the triage unit were calculated for patients as part of the investigation.
Statistical Analysis
IBM SPSS Statistics version 18.0 software was used for data analysis. The normality of data was determined using the Kolmogorov-Smirnov test. Qualitative data were analyzed using the chi-square statistical test, while quantitative variables were assessed using the independent t-test. Sensitivity, specificity, positive and negative predictive values, and positive and negative likelihood ratios (LR) were calculated to evaluate the predictive value of the indices concerning hospital outcomes. Moreover, a significance level of P< 0.05 was considered statistically significant.
Assessment of Diagnostic Values
The receiver operating characteristic (ROC) curve, sensitivity, specificity, and area under the curve (AUC) were utilized to assess the diagnostic value of the indices for in-hospital outcomes. The Youden’s index (J), calculated as J = sensitivity + specificity - 1 and ranging between 0 and 1, was used to interpret the results. A score of 0 indicated test ineffectiveness, while a score of 1 indicated test efficacy.
Results
Demographic and Clinical Characteristics
A total of147 patients were included in the study, and their ages were not normally distributed. The mean age of the patients was 81.49 years (95% CI: 80.62-82.36) with a standard deviation (SD) of ± 5.37 years. The median age was 81 years, and the mode was 75 years. Of the participants, 78 (53.1%) were male, and 69 (46.9%) were female. The most common endoscopic findings were clean-based ulcers, followed by normal endoscopy and gastritis, and 10 patients presented with active bleeding (Figure 1).
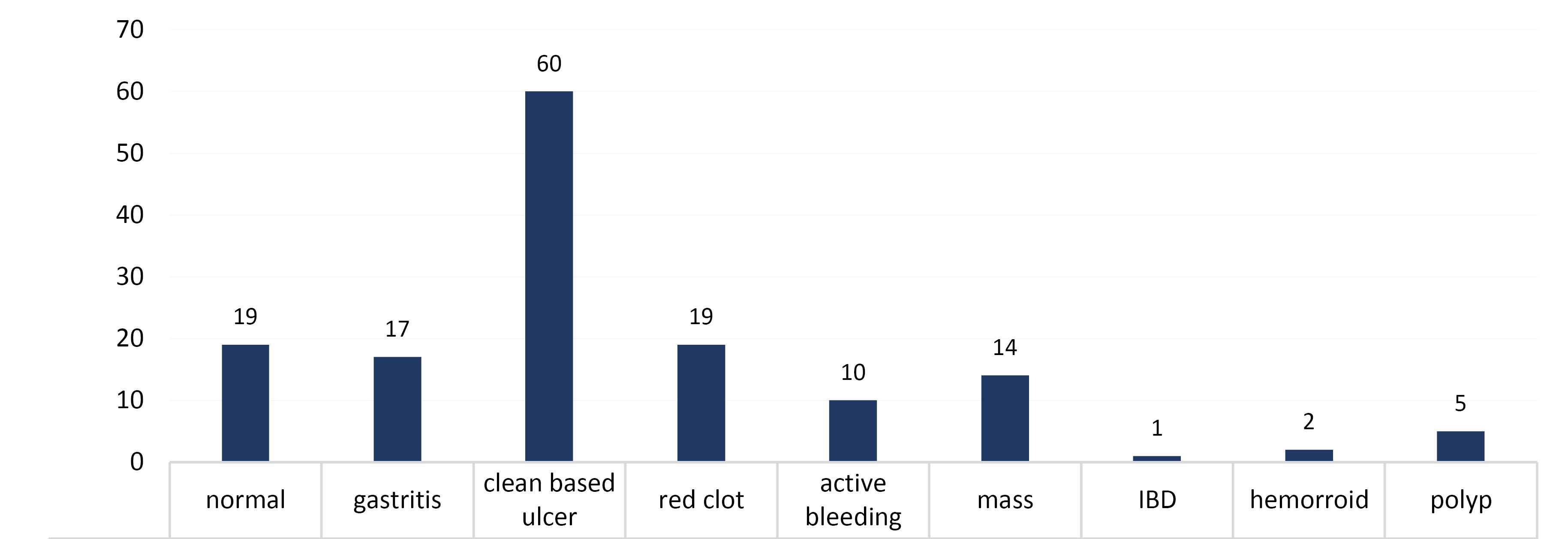
Figure 1.
Frequency of Endoscopic Findings in Patients
.
Frequency of Endoscopic Findings in Patients
Clinical Interventions
A total of 8 patients (5.4%) required surgical intervention, while 139 patients (94.6%) did not have surgical indications. Twenty-eight patients (19%) required hospitalization in the ICU, but 119 patients (81%) did not require intensive care. The average length of hospitalization was 6.41 days (SD ± 8.07 days), with a minimum of 1 day and a maximum of 54 days, and the median and mode hospitalization duration was 3 days.
Patient Outcomes
Regarding patient outcomes, 70% of cases achieved remission, indicating the control of bleeding (remission does not imply the absence of underlying disease, but rather the resolution of GIB), while 30% of patients, unfortunately, passed away.
Outcome Relationship
ICU admission and an increase in the duration of hospitalization corresponded to a higher mortality rate (P value = 0.002). In the ROC curve analysis for SI, RSI, and MSI, the AUCs were 0.339, 0.662, and 0.389, respectively (Figure 2). Concerning the predictive value of these criteria for patient outcomes, it was found that SI, with a cut-off point of 0.9, exhibited a sensitivity of 48.48% (95% CI: 30.80-66.46), a specificity of 86.84% (95% CI: 79.23-92.44), a positive LR of 3.68, and a negative LR of 0.59 (Table 1). Using a cut-off point of 0.7, RSI showed a sensitivity of 33.33% (95% CI: 17.51-96.83), a specificity of 92.04% (95% CI: 85.42-96.29), a positive LR of 4.19, and a negative LR of 0.72 (Table 2). Moreover, MSI, with a cut-off point of 1.46, had a sensitivity of 30.30% (95% CI: 15.48-59.71), a specificity of 91.23% (95% CI: 84.46-95.71), a positive LR of 3.45, and a negative LR of 0.76 (Table 3).
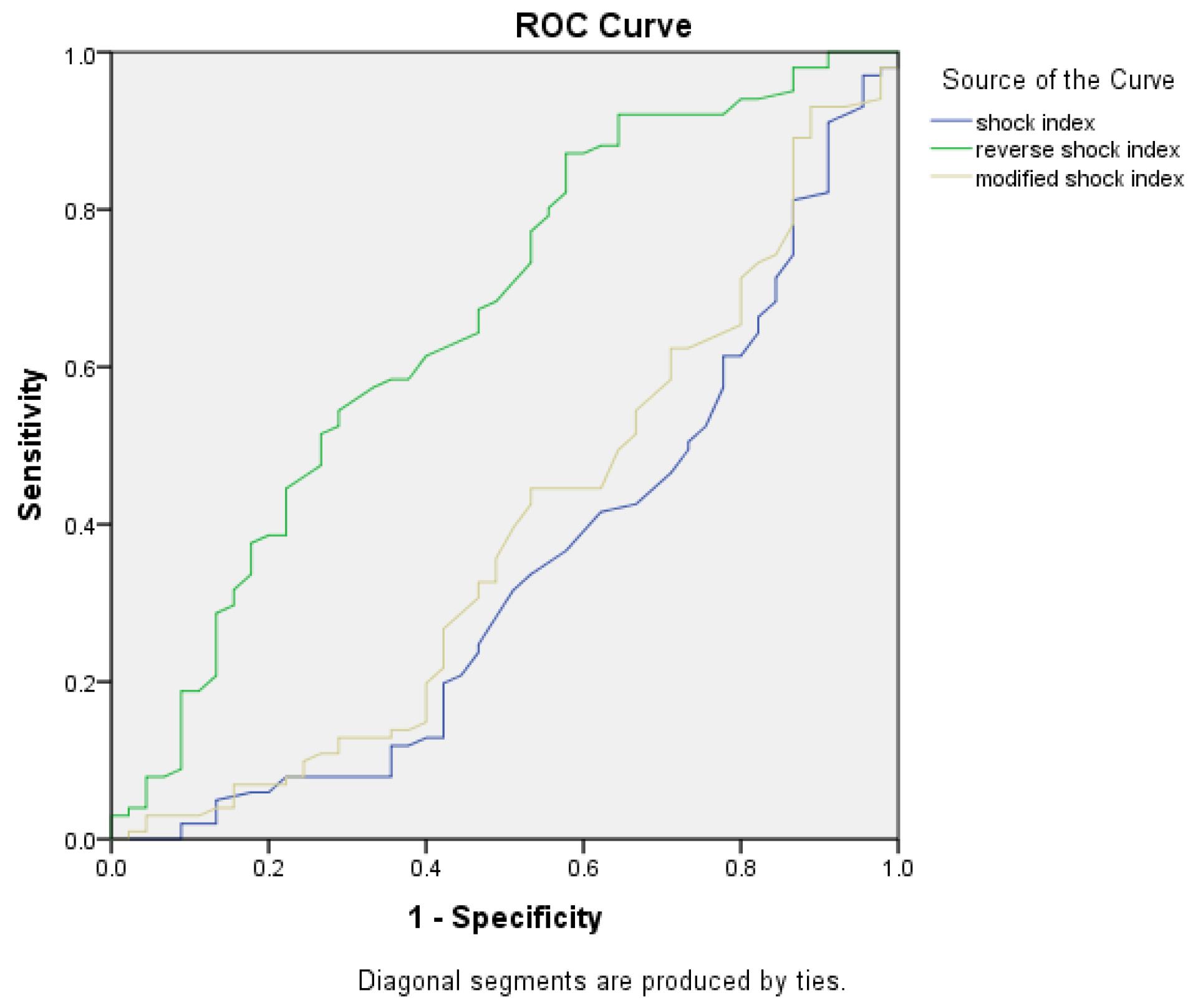
Figure 2.
ROC Diagram for SI, MSI, and RSI. Note. ROC: Receiver operating characteristic; SI: Shock index; RSI: Reverse shock index; MSI: Modified shock index
.
ROC Diagram for SI, MSI, and RSI. Note. ROC: Receiver operating characteristic; SI: Shock index; RSI: Reverse shock index; MSI: Modified shock index
Table 1.
Predicting Value of Shock Index
|
Statistics
|
Value
|
95% CI
|
| Sensitivity |
48.48% |
30.80% - 66.46% |
| Specificity |
86.84% |
79.23% - 92.44% |
| Positive likelihood ratio |
3.68 |
2.05 - 6.64 |
| Negative likelihood ratio |
0.59 |
0.42 - 0.83 |
| Disease prevalence (*) |
22.45% |
15.98% - 30.06% |
| Positive predictive value (*) |
51.61% |
37.20% - 65.76% |
| Negative predictive value (*) |
85.34% |
80.59% - 84.61% |
| Accuracy (*) |
78.23% |
70.68% - 84.61% |
Note. CI: Confidence interval; * These values are dependent on disease prevalence.
Table 2.
Predicting Value of Reverse Shock Index
|
Statistics
|
Value
|
95% CI
|
| Sensitivity |
33.33% |
17.96% - 51.83% |
| Specificity |
92.04% |
85.42% - 96.29% |
| Positive likelihood ratio |
4.19 |
1.90 - 9.23 |
| Negative likelihood ratio |
0.72 |
0.57 - 0.93 |
| Disease prevalence (*) |
22.60% |
16.10% - 30.25% |
| Positive predictive value (*) |
55.00 % |
35.66% - 72.94% |
| Negative predictive value (*) |
82.54% |
78.69% - 85.82% |
| Accuracy (*) |
78.77% |
71.24% - 85.09% |
Note. CI: Confidence interval; * These values are dependent on disease prevalence.
Table 3.
Predicting Value of Modified Shock Index
|
Statistics
|
Value
|
95% CI
|
| Sensitivity |
30.30% |
15.59% - 48.71% |
| Specificity |
91.23% |
84.46% - 95.71% |
| Positive likelihood ratio |
3.45 |
1.57 - 7.58 |
| Negative likelihood ratio |
0.76 |
0.61 - 0.96 |
| Disease prevalence (*) |
22.45% |
15.98% - 30.06% |
| Positive predictive value (*) |
50.00 % |
31.30% - 68.70% |
| Negative predictive value (*) |
81.89% |
78.19% - 85.08% |
| Accuracy (*) |
77.55% |
69.94% - 84.02% |
Note. CI: Confidence interval; * These values are dependent on disease prevalence.
Discussion
This study assessed the predictive value of SI, MSI, and RSI in predicting hospital outcomes for patients with GIB. SI, a measure of hemodynamic instability, has been used since 1967 and has shown higher sensitivity in assessing hemodynamic instability compared to heart rate or systolic blood pressure alone.9,10 The normal range for SI was initially established between 0.5-0.7, but various thresholds have been used in different studies.10-12 This study employed a cut-off point of 0.9, which provides higher specificity but lower sensitivity. Furthermore, SI has found utility in various clinical contexts. For example, it has been associated with increased mortality in septic shock patients,13 the need for massive transfusion and emergency surgical procedures in trauma patients,14 and poorer outcomes in patients with acute myocardial infarction 15. Additionally, it has been used as a triage tool in the emergency department, indicating higher inpatient mortality and hospitalization rates at certain cut-off points.16 Moreover, SI has been associated with bleeding severity in GIB patients.17
The current study revealed that SI, MSI, and RSI exhibit low sensitivities (48%, 30%, and 33%, respectively), with SI having the highest sensitivity. However, these criteria demonstrated high specificities (86%, 91%, and 92%, respectively), with RSI showing the highest specificity. Consequently, none of these criteria proved reliable in predicting poor outcomes for patients. Nonetheless, their high specificities make them useful for ruling out poor outcomes if a patient’s score (SI, MSI, or RSI) falls below the cutoff values.
Interestingly, some studies have reported different results. For instance, Bourque et al found SI to be accurate in predicting 30-day mortality in GIB patients, with a sensitivity of 79% and specificity of 56% at a cutoff point of 0.7.18 Terceros-Almanza et al also demonstrated high sensitivity and specificity for SI and MSI in predicting severe bleeding prognosis.8 However, other studies have reported varying results, emphasizing the need for further investigation.
The present study did not reveal a significant relationship between these indices and the duration of hospitalization or ICU admission. Previous studies have suggested associations between SI and clinical outcomes, considering various confounding variables.19,20
It is important to note that SI and related indices can be influenced by several factors such as pain, anxiety, and measurement methods. Therefore, their use as prognostic tools in UGIB patients remains uncertain. Hence, further research, ideally with larger sample sizes and in multi-center settings, is needed to clarify their prognostic utility. Additionally, accounting for patients’ drug histories in future studies could provide valuable insights.
Strengths and Limitations
Strength
Prospective design: This study utilized a prospective design, allowing for the collection of real-time data on elderly patients with acute UGIB. This design also enhances the accuracy of data collection and minimizes recall bias
Focus on elderly population: Our study specifically focused on patients over 75 years old, addressing a critical gap in the literature regarding the predictive value of SI, MSI, and RSI in this vulnerable population.
Clinical relevance: This research addresses a clinically significant issue, namely, the prediction of patient outcomes in cases of GIB. Identifying effective predictive tools can aid healthcare providers in making timely and informed decisions for patient management.
Calculation of predictive indices: We rigorously calculated SI, MSI, and RSI for all patients, enabling a direct comparison of these indices in predicting hospital outcomes. This standardized approach ensures consistency in the evaluation of the indices.
Limitations
Small sample size: One of the primary limitations of this study is the relatively small sample size. Although 147 elderly patients were included, a larger sample size would enhance the statistical power and improve the generalizability of the findings.
Single-center study: This research was conducted exclusively at a single university hospital in Tabriz, Iran. The use of a single-center design limits the generalizability of the results to a broader population of elderly patients with GIB. Future research should prioritize external validation of these indices in larger and more diverse patient populations to confirm their predictive value across different healthcare settings.
Cutoff values: The study utilized predetermined cutoff values for SI, MSI, and RSI to classify patients. These cutoff values may not be universally applicable, and different thresholds might yield different results.
Limited sensitivity: The findings of the study revealed that SI, MSI, and RSI exhibit relatively low sensitivity in predicting patient outcomes. This suggests that while these indices demonstrated high specificity, they may not be effective in identifying patients at risk of poor outcomes.
Conclusions
First and foremost, the findings of the current study unequivocally demonstrated that none of these indices possesses the requisite efficacy to serve as reliable predictors of mortality in cases of GIB. While SI, RSI, and MSI exhibited remarkable specificity in predicting the hospital outcomes for patients with GIB, their performance falters when it comes to diagnosing the condition and prognosticating unfavorable outcomes. Despite their effectiveness in ruling out life-threatening conditions, the limited sensitivity of these criteria renders them less effective for diagnostic and prognostic purposes. It is imperative to acknowledge that our study uncovered no conclusive relationship between these three indices and the duration of hospitalization or the need for ICU admission.
Author contributions
Conceptualization: Seyedpouya Paknezhad, Amir Ghafarzad.
Formal analysis: Zahra Vandrajabpour, Zahra parsian.
Investigation: Zahra Vandrajabpour, Hamidreza Mortezabagi.
Methodology: Seyedpouya Paknezhad.
Resources: Hamidreza Mortezabagi.
Supervision: Seyedpouya Paknezhad.
Validation: Zahra parsian, Amir Ghafarzad.
Visualization: Aisan Akhgari.
Writing- original draft: Aisan Akhgari, Zahra Vandrajabpour.
Writing- review & editing: Amir Ghafarzad, Seyedpoua Paknezhad, Hamidreza Mortezabagi.
Data availability statement
Data will be available by contacting corresponding author.
Ethical approval
This study was aproved by Regional Ethic Commitee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1398.805).
Consent for publication
None.
Conflict of interests
There is not any conflict of interests.
References
- Walls R, Hockberger R, Gausche-Hill M. Rosen’s Emergency Medicine-Concepts and Clinical Practice E-Book. Elsevier Health Sciences; 2017.
- Doshi A, Boudreaux ED, Wang N, Pelletier AJ, Camargo CA Jr. National study of US emergency department visits for attempted suicide and self-inflicted injury, 1997-2001. Ann Emerg Med 2005; 46(4):369-75. doi: 10.1016/j.annemergmed.2005.04.018 [Crossref] [ Google Scholar]
- Stanley AJ, Dalton HR, Blatchford O, Ashley D, Mowat C, Cahill A. S1385: multicentre comparison of the Glasgow-Blatchford and Rockall scores in the prediction of clinical end-points in upper GI haemorrhage. Gastrointest Endosc 2010; 71(5):AB147. doi: 10.1016/j.gie.2010.03.159 [Crossref] [ Google Scholar]
- Chico-Fernández M, García-Fuentes C, Alonso-Fernández MA, Toral-Vázquez D, Bermejo-Aznarez S, Alted-López E. [Massive transfusion predictive scores in trauma Experience of a transfusion registry]. Med Intensiva 2011; 35(9):546-51. doi: 10.1016/j.medin.2011.06.010.[Spanish] [Crossref] [ Google Scholar]
- Victorino GP, Battistella FD, Wisner DH. Does tachycardia correlate with hypotension after trauma?. J Am Coll Surg 2003; 196(5):679-84. doi: 10.1016/s1072-7515(03)00128-5 [Crossref] [ Google Scholar]
- Brasel KJ, Guse C, Gentilello LM, Nirula R. Heart rate: is it truly a vital sign?. J Trauma 2007; 62(4):812-7. doi: 10.1097/TA.0b013e31803245a1 [Crossref] [ Google Scholar]
- Gutierrez G, Reines HD, Wulf-Gutierrez ME. Clinical review: hemorrhagic shock. Crit Care 2004; 8(5):373-81. doi: 10.1186/cc2851 [Crossref] [ Google Scholar]
- Terceros-Almanza LJ, García-Fuentes C, Bermejo-Aznárez S, Prieto-Del Portillo IJ, Mudarra-Reche C, Sáez de la Fuente I. Prediction of massive bleeding Shock index and modified shock index. Med Intensiva 2017; 41(9):532-8. doi: 10.1016/j.medin.2016.10.016 [Crossref] [ Google Scholar]
- Allgöwer M, Burri C. Schockindex. Dtsch Med Wochenschr 1967; 92(43):1947-50. [ Google Scholar]
- Rassameehiran S, Teerakanok J, Suchartlikitwong S, Nugent K. Utility of the shock index for risk stratification in patients with acute upper gastrointestinal bleeding. South Med J 2017; 110(11):738-43. doi: 10.14423/smj.0000000000000729 [Crossref] [ Google Scholar]
- Tseng J, Nugent K. Utility of the shock index in patients with sepsis. Am J Med Sci 2015; 349(6):531-5. doi: 10.1097/maj.0000000000000444 [Crossref] [ Google Scholar]
- Balhara KS, Hsieh YH, Hamade B, Circh R, Kelen GD, Bayram JD. Clinical metrics in emergency medicine: the shock index and the probability of hospital admission and inpatient mortality. Emerg Med J 2017; 34(2):89-94. doi: 10.1136/emermed-2015-205532 [Crossref] [ Google Scholar]
- Jouffroy R, Pierre Tourtier J, Gueye P, Bloch-Laine E, Bounes V, Debaty G. Prehospital shock index to assess 28-day mortality for septic shock. Am J Emerg Med 2020; 38(7):1352-6. doi: 10.1016/j.ajem.2019.11.004 [Crossref] [ Google Scholar]
- Marenco CW, Lammers DT, Morte KR, Bingham JR, Martin MJ, Eckert MJ. Shock index as a predictor of massive transfusion and emergency surgery on the modern battlefield. J Surg Res 2020; 256:112-8. doi: 10.1016/j.jss.2020.06.024 [Crossref] [ Google Scholar]
- Zhang X, Wang Z, Wang Z, Fang M, Shu Z. The prognostic value of shock index for the outcomes of acute myocardial infarction patients: a systematic review and meta-analysis. Medicine (Baltimore) 2017; 96(38):e8014. doi: 10.1097/md.0000000000008014 [Crossref] [ Google Scholar]
- Balhara KS, Hsieh YH, Hamade B, Circh R, Kelen GD, Bayram JD. Clinical metrics in emergency medicine: the shock index and the probability of hospital admission and inpatient mortality. Emerg Med J 2017; 34(2):89-94. doi: 10.1136/emermed-2015-205532 [Crossref] [ Google Scholar]
- Hagiwara A, Kimura A, Kato H, Mizushima Y, Matsuoka T, Takeda M. Hemodynamic reactions in patients with hemorrhagic shock from blunt trauma after initial fluid therapy. J Trauma 2010; 69(5):1161-8. doi: 10.1097/TA.0b013e3181d27c94 [Crossref] [ Google Scholar]
- Bourque JS, Cliche J, Chauny J, Daoust R, Paquet J, Piette É. Accuracy of the shock index and various modified shock indexes to predict early mortality in patients suffering from gastrointestinal haemorrhage. Crit Care 2013; 17(Suppl 2):P219. doi: 10.1186/cc12157 [Crossref] [ Google Scholar]
- Torabi M, Moeinaddini S, Mirafzal A, Rastegari A, Sadeghkhani N. Shock index, modified shock index, and age shock index for prediction of mortality in emergency severity index level 3. Am J Emerg Med 2016; 34(11):2079-83. doi: 10.1016/j.ajem.2016.07.017 [Crossref] [ Google Scholar]
- Myint PK, Sheng S, Xian Y, Matsouaka RA, Reeves MJ, Saver JL. Shock index predicts patient-related clinical outcomes in stroke. J Am Heart Assoc 2018; 7(18):e007581. doi: 10.1161/jaha.117.007581 [Crossref] [ Google Scholar]