Int J Aging.2023;1 :e11.
doi: 10.34172/ija.2023.e11
Original Article
The Predictive Value of mREMS and NTS Scores in the Hospital Outcomes of Elderly Patients With a Traffic Accident
Hadi Mostafaei 1  , Moloud Balafar 2
, Moloud Balafar 2  , Seyed Pouya Paknezhad 2, Mohammad Saadati 3, Nooshin Milanchian 4, Aysan M. Namdar 5, Tooba Fouladi Yamchi 5, Kavous Shahsavarinia 1, 5, *
, Seyed Pouya Paknezhad 2, Mohammad Saadati 3, Nooshin Milanchian 4, Aysan M. Namdar 5, Tooba Fouladi Yamchi 5, Kavous Shahsavarinia 1, 5, * 
Author information:
1Department of Urology, Comprehensive Cancer Center, Medical University of Vienna, Vienna, Austria
2Emergency and Trauma Care Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
3Khoy University of Medical Sciences, Khoy, Iran
4Islamic Azad University of Medical Sciences, Tabriz, Iran
5Road Traffic Injury Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Objectives:
To investigate the predictive value of two novel scores, including the modified rapid emergency medicine score (mREMS) and new trauma score (NTS), in the outcome of hospitalized elderly patients with traffic injuries.
Design:
Descriptive-analytical cross-sectional study.
Setting(s):
Tabriz, the capital of East Azerbaijan province, northwestern Iran.
Participants:
Over 65 years old patients being injured in traffic accidents were included in the current study and divided into three groups. Logistic regression analysis was used to determine the predictive value of mREMS and NTS scores in elderly patients with traffic accidents.
Outcome measures:
NTS is based on a revision of the revised trauma score (RTS) parameters, which includes replacing the Glasgow coma scale (GCS) score with the GCS code and the number of breaths per minute with blood oxygen saturation (SpO2 ). The mREMS includes age, systolic blood pressure (SBS), heart rate (HR), respiratory rate (RR), SpO2, and GCS.
Results:
Totally, 243 elderlies with road traffic injuries were enrolled in this study. The mREMS score in male patients showed a significant difference, and the odds ratio (OR) in these patients was 1.5 (95% confidence interval [CI]=1.15-1.95, P<0.05). Based on the results, the NTS significantly differed in male patients, and the OR in these patients was 0.97 (95% CI=0.95- 0.99, P<0.05). The NTS had similar discrimination to mREMS in the prediction of elderly patients’ severity of trauma (hospitalization or discharge). In cut-off point 7.5, the sensitivity of mREMS and specificity were 71% and 53%, respectively. In cut-off point 216, the sensitivity and specificity of NTS were 84% and 47%, respectively.
Conclusions:
mREMS and NTS have a moderate degree of predictive usefulness for older patients who have sustained many traumas. It is advised that this problem should be further assessed accurately by a thorough investigation.
Keywords: Trauma, Elderly patients, Emergency department
Introduction
Road accidents are the leading cause of injury-related mortality in hospitals. About 1.35 cases die each year due to road accidents. In addition, 20-50 million people will suffer from non-fatal complications. The cost imposed on communities due to traffic accidents is equal to 3% of the mass production of countries.1 According to the World Health Organization, the number of elderly is increasing, and it is estimated that between 2015 and 2050, it will almost double from 12% to 22%.2 Trauma in the elderly increases with age and is one of the important causes of mortality and morbidity.3,4 Poor vision, hearing, and musculoskeletal system associated with decreased visual acuity, poor sound perception, postural instability, and reduced reaction time are related to age.5,6 Immediate and delayed consequences in the elderly after traumatic events are skeletal fractures, skull injuries, and death.7,8 Compared to young people, older people with similar traumas are at higher risk of death and longer hospital stays.9,10 Trauma scores for trauma patients have long been an important component of prehospital triage.11-13 The Glasgow Coma Scale (GCS) score was replaced with the GCS code, and the respiratory rate (RR) was replaced with blood oxygen saturation (SpO2), making the new trauma score (NTS) a refinement of the revised trauma score (RTS) parameters that were used to determine the prognosis.14-16 Another score created in 2004 is the modified rapid emergency medicine score (mREMS), which incorporates age, systolic blood pressure (SBP), heart rate (HR), RR, SpO2, and GCS.17,18 This investigation will help the healthcare system to plan to reduce mortality in the elderly by choosing efficient methods to assess patients’ prognoses. It also enables better management of elderly traumatic patients by physicians with accurate knowledge of the characteristics affecting mortality in the elderly.
Methods
In this descriptive-analytical cross-sectional study, after obtaining approval from the regional ethics committee (IR.TBZMED.REC.1399.119), all elderly people with traffic accidents referred to the emergency department of a Hospital from September 2020 to September 2021 were evaluated by the triage nurse.
Patients over 65 with traffic accidents who were referred to the emergency department met the inclusion criteria. Defects in patients’ clinical records for factors such as personal satisfaction or transfer to other centers were considered the exclusion criteria. The data collecting form included patient demographic information such as age, gender, length of hospital stay, underlying conditions, and accident type. Moreover, areas affected by trauma and patients’ hemodynamic parameters, type of vehicle (car, motorcycle, or non-motorized vehicles), and the role of the elderly in the accident (driver, passenger, or pedestrian) were recorded, and patients were evaluated for mREMS and NTS, as well as radiographic findings and nosocomial infections. To evaluate the anatomical location of the trauma, patients were examined for the abbreviated injury scale. Patients were classified into three groups, including Patients in the age range of 65-74, 75-84, and over 85 years old. Their gender, accident type, contribution to the accident, and results were all investigated as well. Frequencies and percentages, as well as means and standard deviations were utilized for reporting qualitative and quantitative data, respectively. For continuous variables, the means of two unrelated groups were compared using an independent t-test. Patients’ hospital outcomes were divided into two groups, including inpatient and discharge groups, in order to assess the predictive usefulness of mREMS and NTS. The predictive usefulness of the mREMS in elderly individuals involved in traffic accidents was evaluated using logistic regression analysis. The prognostic significance of the NTS in the hospital outcome of elderly patients involved in traffic accidents was also assessed using logistic regression analysis. The statistical analysis of the data was performed using IBM SPSS, version 21.0. (IBM Corp., Armonk, USA). A P value of 0.05 was used in this investigation to determine the significance level.
Results
The information of 243 injured people in traffic accidents being over 65 years old who have been registered in the traffic accident system from the beginning of September 2020 to the end of August 2021, was evaluated in this study. The average age of the elderly injured in traffic accidents was about 73 ± 6.9 years old; overall, 67.6% and 32.4% of them were males and females, respectively. Mean SBP, SpO2 level, level of consciousness, rater, and HR were 120.3 ± 25.8 mm Hg, 95.5 ± 3.3%, 14.4 ± 2.2, 18.5 ± 7.6 per minute, and 84.7 ± 3.6 per minute, respectively. The majority of injured elderly people in each age group were men.
Table 1 provides the demographic information of the elderly injured in traffic accidents. The odds ratio (OR) for male patients with the significantly different mREMSs was 1.5 (95% CI = 1.15-1.95, P < 0.05) in the logistic regression study for the predictive usefulness of the mREMS in senior patients involved in traffic accidents, implying that for one unit increase in the mREMS, the chance of hospitalization in male patients increased by 50%, while the mREMS in female patients demonstrated no significant difference.
Table 1.
Demographic and Traffic Information of the Elderly Injured in Traffic Accidents
|
Age Group
|
Gender
|
Frequency (%)
|
Type of Accident
|
Frequency (%)
|
Patient Role in the Accident
|
Frequency (%)
|
Outcome
|
Frequency (%)
|
| 65-74 |
Male |
99 (65.6) |
Vehicle-passerby |
73 (48.3) |
Passerby |
74 (48.7) |
Outpatient |
49 (65.3) |
|
|
Vehicle-object |
8 (5.3) |
|
36 (23.7) |
|
|
|
|
Vehicle-animal |
1 (0.7) |
Driver |
|
|
|
|
|
Vehicle-Vehicle |
46 (30.5) |
|
|
|
|
| Female |
52 (34.4) |
Overturning |
13 (8.6) |
Passenger |
40 (26.3) |
Inpatient |
26 (34.7) |
|
|
Fall |
4 (2.6) |
|
|
|
|
|
|
Off the road |
2 (1.3) |
Others |
2 (1.3) |
|
|
|
|
Others |
4 (2.6) |
|
|
|
|
| 75-84 |
Male |
43 (70.5) |
Vehicle-passerby |
43 (69.3) |
Passerby |
3 (69.3) |
Outpatient |
17 (56.7) |
|
|
Vehicle-object |
3 (4.8) |
|
|
|
|
|
|
Vehicle-vehicle |
13 (21.0) |
|
|
|
|
| Female |
|
Overturning |
2 (3.2) |
Passenger |
11 (17.7) |
Inpatient |
13 (43.3) |
|
|
Others |
1 (1.6) |
|
|
|
|
| > 85 |
Male |
13 (68.4) |
Vehicle-passerby |
13 (72.2) |
Passerby |
14 (73.7) |
Outpatient |
4 (50.0) |
|
|
Vehicle-vehicle |
4 (22.2) |
Driver |
1 (5.3) |
|
|
| Female |
6 (31.6) |
Overturning |
1 (5.6) |
Passenger |
4 (21.0) |
Inpatient |
4 (50.0) |
Note. OR: Odds ratio; CI: Confidence interval; NTS: New trauma score; GCS: Glasgow Coma Scale; SBP: Systolic blood pressure; SpO2: Peripheral oxygen saturation.
The NTS in male patients showed a significant difference in the hospital outcome of elderly patients involved in traffic accidents, and the OR in these patients was 0.97 (95% CI = 0.95-0.99, P < 0.05). More precisely, for every unit increase in the NTS, the likelihood of hospitalization in male patients decreased by 0.03%, while NTSs represented the discernible difference in female patients (Table 2).
Table 2.
Univariate Logistic Regression Analysis for mREMS and NTS Scores
|
Score
|
Gender
|
OR
|
95% CI
|
P
Value
|
| mREMS |
Male |
1.5 |
1.15-1.95 |
0.003 |
| Female |
1.2 |
0.77-1.89 |
0.414 |
| NTS |
Male |
0.97 |
0.95-0.99 |
0.01 |
| Female |
0.98 |
0.96-1.01 |
0.182 |
Note. OR: Odds ratio; CI: Confidence interval; NTS: New trauma score; GCS: Glasgow Coma Scale; SBP: Systolic blood pressure; SpO2: Peripheral oxygen saturation; mREMSL Modified rapid emergency medicine score.
The ROC and the AUC formulas were utilized to determine the predictive value of the NTS and mREMS in the severity of trauma (hospitalization or discharge). Tables 3 and 4, as well as Figures 1 and 2, demonstrate how the AUC of scores is roughly equal. Based on the results, the sensitivity and specificity of mREMS and NTS were 71% and 53% at cutoff point 7.5, as well as 84% and 47% at cut-off point 216, respectively.
Table 3.
Predictive Value of NTS in the Severity of Trauma (Hospitalization or Discharge) of Patients Using the ROC
|
AUC |
|
Test Result Variable(s): NTS Scores
|
|
Area
|
SE
|
P
Value
|
Asymptotic 95% CI
|
|
Lower limit
|
Upper limit
|
| 0.642 |
0.054 |
0.010 |
0.535 |
0.748 |
Note. AUC: Area under the curve; CI: Confidence interval; SE: Standard error.
Table 4.
Predictive Value of mREMS Trauma Scores in the Severity of Trauma (Hospitalization or Discharge) of Patients Using the ROC Curve
|
AUC
|
|
Test Result Variable(s): mREMS
|
|
Area
|
SE
|
P
Value
|
Asymptotic 95% CI
|
|
Lower Limit
|
Upper Limit
|
| 0.668 |
0.055 |
0.003 |
0.560 |
0.775 |
Note. AUC: Area under curve; SE: Standard error; CI: Confidence interval.
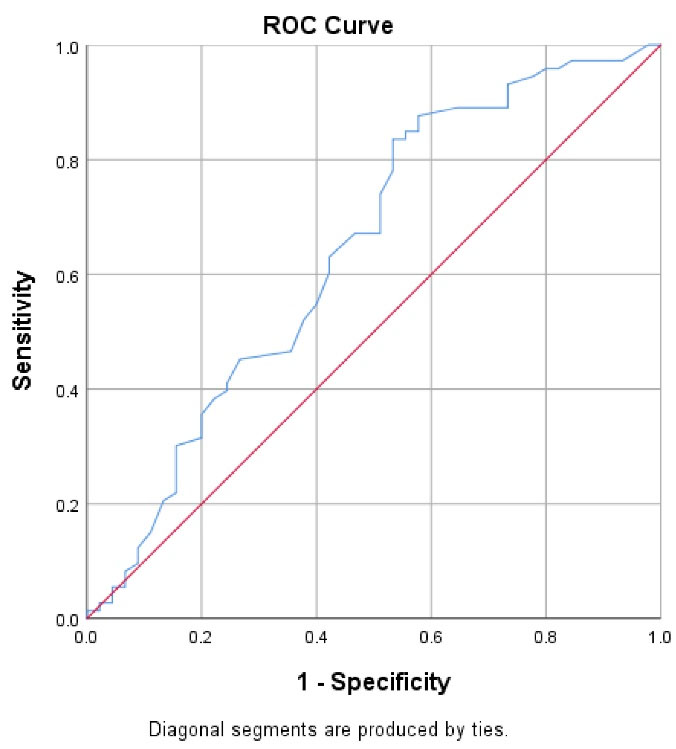
Figure 1.
ROC Curve of NTS Variable in Predicting the Severity of Trauma (Hospitalization or Discharge). Note. ROC: Receiver operating characteristic curve; NTS: New trauma score
.
ROC Curve of NTS Variable in Predicting the Severity of Trauma (Hospitalization or Discharge). Note. ROC: Receiver operating characteristic curve; NTS: New trauma score
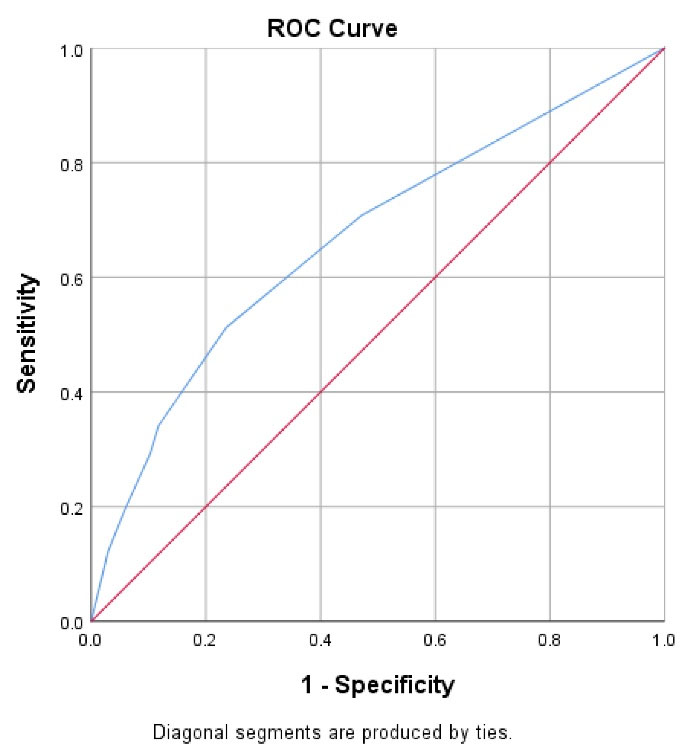
Figure 2.
ROC curve of mREMS Variable in Predicting the Severity of Trauma (Hospitalization or Discharge). Note. ROC: Receiver operating characteristic curve; mREMS: Modified rapid emergency medicine score
.
ROC curve of mREMS Variable in Predicting the Severity of Trauma (Hospitalization or Discharge). Note. ROC: Receiver operating characteristic curve; mREMS: Modified rapid emergency medicine score
Discussion
Approximately 5.8 million deaths from trauma occur each year, accounting for 10% of all mortality worldwide.19 The results of studies represented that the highest incidence of accidents was related to people over 60 years. Elderly people are more at risk of injuries and deaths due to motor vehicle accidents than young people, and among elderly road users, pedestrians are highly vulnerable.20 Iran is one of the countries with the highest number of deaths due to traffic accidents. On the other hand, the issue of accidents in the elderly is of great importance today because, first of all, the elderly population is increasing, and statistical indicators show that the aging process has begun in our country, and according to forecasts by 1429, the elderly population in the country will reach 24.9%. Secondly, the mobility and lifestyle of the elderly put them at risk of serious harm. Additionally, consistent with the results of the present study, Furtado et al found that most of the elderly who were injured in road accidents were men.21 A thorough assessment of the severity of the trauma is essential for enhancing trauma care since the severity of trauma injuries affects mortality and morbidity in trauma patients. Several scoring systems have been created in recent years to evaluate the severity of trauma patients’ injuries and to offer an impartial scale for the patient’s initial condition as part of the therapy selection criteria. Nevertheless, there is no widely used grading system for determining the severity of trauma.22 It goes without saying that better trauma patient care outcomes result from the ability to forecast death at the moment of admission with speed and accuracy. The optimum scoring system for emergency use should include a limited number of factors.23 Since Champion et al introduced RTS roughly 30 years ago, this technique has been extensively utilized to assess the prognosis of trauma patients. Changes to RTS parameters are required according to recent studies. As a result, NTS was created using the updated parameters, which included a change to the actual GCS rather than the GCS code, a change to the SBP interval used to calculate the code value, and a change in SpO2 rather than the rate of respiration.24 To determine the predictive value of the NTS in elderly patients, the results of this study are consistent with previous findings.24,25 REMS is a simplified version of Acute Physiology and Chronic Health Evaluation II that allows rapid score calculation.26 REMS is determined based on the GCS, RR, SpO2, MAP, HR, and age. This score has been demonstrated to be an accurate predictor of death in emergency room patients who are not undergoing surgery.27 REMS has been altered, along with mREMS. The results of the current study, which assessed the predictive usefulness of the mREMS in elderly patients involved in traffic accidents, are consistent with those of the earlier study.17 In contrast to more sophisticated scores that frequently call for aggressive measures, the mREMS is an adaptation of the REMS and is intended to be a real-time triage score that can accurately predict mortality during hospitalization. The mREMS is less arbitrary and takes less time to calculate than certain other models (e.g., injury severity score), while still serving as a predictor of death.17 Given the frequency of traffic accidents and severe and fatal injuries in Iran and its individual, social, and economic consequences, it is obvious that the first and most basic step in preventing and controlling accidents in the elderly, timely identification, and evaluation of problems and drawing of accurate situation is available to be able to make the necessary plans to control them and thus reduce the burden of injuries caused by traffic accidents in the elderly.
The predicted travel time (PTT) is a measure of how far the traumatic patient has to travel to get to a competent injury care facility.28 Understanding how PTTs affect patient outcomes may help advance the value and effectiveness of injury care delivery by highlighting changes to the injury framework organization given that significant resources are invested to maintain trauma center (TC) status. Greater PTTs to trauma care result in lower TC use rates after serious injury according to a recent Canadian study.29 There have also been reports of variations in PTTs to Canadian TCs. Uncertainty persists on the connection between PTTs to TCs and mortality following significant trauma. There is a higher chance of death for trauma patients hurt in locations with higher PTTs to TCs. The method of injury alters the strength of this link and the possible causes behind it. Higher chances of ejection after motor vehicle crashes in more rural regions imply that behavioral patterns (e.g., seatbelt use) may be at least partially to blame for this link. Higher PTTs to trauma care increased the chance of death in cases of penetrating trauma, and this association persisted after scene deaths were excluded, suggesting that variations in post-injury care or delayed post-scene transport durations may account for this finding. Reducing prehospital delays for patients hurt in distant places may improve their outcomes because patients injured in areas with less access to trauma care were more likely to have longer prehospital intervals.29
In-hospital mortality in trauma patients was not significantly predicted by the NTS according to the study of Galvagno et al; nonetheless, the result of this result is in line with that of the other research, claiming that NTS was a substantial predictor of mortality in trauma patients.30 One meta-analysis comprehensively examined the accuracy of physiological scoring systems (WPS) in predicting the mortality of critically ill patients based on data from 25 articles. The overall study revealed that for the REMS, RAPS, mREMS, and WPS criteria, the respective areas under the summary ROC curve were 0.83, 0.89, 0.64, and 0.86, respectively. In-hospital mortality was well predicted by the three models (i.e., RAPS, REMS, and WPS) according to the analysis. Additionally, compared to other patient scenarios, the value of these models in trauma patients was significantly higher.31
To the best of our knowledge, few comparative studies have been performed, especially in Iran, on the two scoring systems. Therefore, it is suggested that in future research, the efficiency of these two scoring systems is examined more comprehensively and compared with other systems in the emergency department on trauma patients.
Conclusions
The findings suggested that mREMS and NTS have a moderate degree of predictive usefulness for older patients who have sustained many traumas. It is recommended that this issue be further evaluated appropriately by applying a thorough investigation.
Acknowledgments
The authors would like to appreciate the cooperation of the Clinical Research Development Unit, Imam Reza General Hospital, Tabriz, Iran, in conducting this research. This article was written based on a dataset of Tooba Fouladi Yamchi’s Medical degree thesis entitled, “The predictive value of mREMS and NTS scores in the hospital outcome of elderly patients with traffic accidents, Tabriz, Iran.” This study was registered at Tabriz University of Medical Sciences (Code No: 63836).
Funding
Not applicable.
Data availability statement
The datasets generated and analyzed during the current study are not publicly available due to the restriction of the Ethic Committee of Tabriz University of Medical Sciences but are available from the corresponding author upon reasonable request.
Ethical approval
The Tabriz University of Medical Sciences, Tabriz, Iran (Ethics code: IR.TBZMED.REC.1399.119) approved the present report. All aspects of the present study were explained to patients, and written informed consent was obtained from the participants or their next of kin.
Consent for publication
Not applicable.
Conflict of interests
The authors declare that they have no conflict of interests.
References
- World Health Organization (WHO). Global Status Report on Road Safety 2018: Summary. WHO; 2018.
- World Health Organization (WHO). World Report on Aging and Health. WHO; 2015.
- Aschkenasy MT, Rothenhaus TC. Trauma and falls in the elderly. Emerg Med Clin North Am 2006; 24(2):413-32. doi: 10.1016/j.emc.2006.01.005 [Crossref] [ Google Scholar]
- da Silva HC, de Lima Pessoa R, de Menezes RM. Trauma in elderly people: access to the health system through pre-hospital care. Rev Lat Am Enfermagem 2016; 24:e2690. doi: 10.1590/1518-8345.0959.2690 [Crossref] [ Google Scholar]
- Kirshenbom D, Ben-Zaken Z, Albilya N, Niyibizi E, Bala M. Older age, comorbid illnesses, and injury severity affect immediate outcome in elderly trauma patients. J Emerg Trauma Shock 2017; 10(3):146-50. doi: 10.4103/jets.jets_62_16 [Crossref] [ Google Scholar]
- Gioffrè-Florio M, Murabito LM, Visalli C, Pergolizzi FP, Famà F. Trauma in elderly patients: a study of prevalence, comorbidities and gender differences. G Chir 2018; 39(1):35-40. doi: 10.11138/gchir/2018.39.1.035 [Crossref] [ Google Scholar]
- Jacobs DG. Special considerations in geriatric injury. Curr Opin Crit Care 2003; 9(6):535-9. doi: 10.1097/00075198-200312000-00012 [Crossref] [ Google Scholar]
- Schoeneberg C, Probst T, Schilling M, Wegner A, Hussmann B, Lendemans S. Mortality in severely injured elderly patients: a retrospective analysis of a German level 1 trauma center (2002-2011). Scand J Trauma Resusc Emerg Med 2014; 22:45. doi: 10.1186/s13049-014-0045-3 [Crossref] [ Google Scholar]
- Demetriades D, Sava J, Alo K, Newton E, Velmahos GC, Murray JA. Old age as a criterion for trauma team activation. J Trauma 2001; 51(4):754-6. doi: 10.1097/00005373-200110000-00022 [Crossref] [ Google Scholar]
- Kuhne CA, Ruchholtz S, Kaiser GM, Nast-Kolb D. Mortality in severely injured elderly trauma patients--when does age become a risk factor?. World J Surg 2005; 29(11):1476-82. doi: 10.1007/s00268-005-7796-y [Crossref] [ Google Scholar]
- McCoy GF, Johnston RA, Duthie RB. Injury to the elderly in road traffic accidents. J Trauma 1989; 29(4):494-7. doi: 10.1097/00005373-198904000-00013 [Crossref] [ Google Scholar]
- Champion HR, Copes WS, Buyer D, Flanagan ME, Bain L, Sacco WJ. Major trauma in geriatric patients. Am J Public Health 1989; 79(9):1278-82. doi: 10.2105/ajph.79.9.1278 [Crossref] [ Google Scholar]
- Garkaz O, Salari Lak S, Mehryar HR, Khalkhali HR. Study ending of hospitalized traffic accidents injured in Urmia Imam Khomeini hospital by using TRISS method. Iran J Forensic Med 2019;24(4):23-9. [Persian].
- Eid HO, Abu-Zidan FM. New Injury Severity Score is a better predictor of mortality for blunt trauma patients than the Injury Severity Score. World J Surg 2015; 39(1):165-71. doi: 10.1007/s00268-014-2745-2 [Crossref] [ Google Scholar]
- Nakhjavan-Shahraki B, Yousefifard M, Hajighanbari MJ, Karimi P, Baikpour M, Mirzay Razaz J. Worthing physiological score vs revised trauma score in outcome prediction of trauma patients; a comparative study. Emerg (Tehran) 2017; 5(1):e31. [ Google Scholar]
- Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Flanagan ME. A revision of the trauma score. J Trauma 1989; 29(5):623-9. doi: 10.1097/00005373-198905000-00017 [Crossref] [ Google Scholar]
- Miller RT, Nazir N, McDonald T, Cannon CM. The modified rapid emergency medicine score: a novel trauma triage tool to predict in-hospital mortality. Injury 2017; 48(9):1870-7. doi: 10.1016/j.injury.2017.04.048 [Crossref] [ Google Scholar]
- Setioputro B, Listiyawati I, Muhammad Nur KR. The Risk of Mortality on Patients with Traffic Accidents of Emergency Department at dr. Soebandi Regional Hospital, Jember Regency. 2020. http://localhost:8080/xmlui/handle/123456789/645.
- Lendrum RA, Lockey DJ. Trauma system development. Anaesthesia 2013; 68 Suppl 1:30-9. doi: 10.1111/anae.12049 [Crossref] [ Google Scholar]
- Razzaghi A, Pourrajabi A, Daneshi S. Obstacles and problems related to elderly pedestrians: a qualitative study. Safety Promot Inj Prev (Tehran) 2017;5(2):73-8. [Persian].
- Furtado BM, de Lima AC, Ferreira RC. Road traffic accidents involving elderly people: an integrative review. Rev Bras Geriatr Gerontol 2019; 22(3):e190053. doi: 10.1590/1981-22562019022.190053 [Crossref] [ Google Scholar]
- Raum MR, Nijsten MW, Vogelzang M, Schuring F, Lefering R, Bouillon B. Emergency trauma score: an instrument for early estimation of trauma severity. Crit Care Med 2009; 37(6):1972-7. doi: 10.1097/CCM.0b013e31819fe96a [Crossref] [ Google Scholar]
- Park HO, Kim JW, Kim SH, Moon SH, Byun JH, Kim KN. Usability verification of the emergency trauma score (EMTRAS) and rapid emergency medicine score (REMS) in patients with trauma: a retrospective cohort study. Medicine (Baltimore) 2017; 96(44):e8449. doi: 10.1097/md.0000000000008449 [Crossref] [ Google Scholar]
- Jeong JH, Park YJ, Kim DH, Kim TY, Kang C, Lee SH. The new trauma score (NTS): a modification of the revised trauma score for better trauma mortality prediction. BMC Surg 2017; 17(1):77. doi: 10.1186/s12893-017-0272-4 [Crossref] [ Google Scholar]
- Khajoei R, Abadi MZ, Dehesh T, Heydarpour N, Shokohian S, Rahmani F. Predictive value of the Glasgow Coma Scale, age, and arterial blood pressure and the new trauma score indicators to determine the hospital mortality of multiple trauma patients. Arch Trauma Res 2021; 10(2):86-91. [ Google Scholar]
- Jiang X. An improved modified early warning score that incorporates the abdomen score for identifying multiple traumatic injury severity. PeerJ 2020; 8:e10242. doi: 10.7717/peerj.10242 [Crossref] [ Google Scholar]
- Lee SH, Park JM, Park JS, Kim KH, Shin DW, Jeon WC. Utility of the rapid emergency medicine score (REMS) for predicting hospital mortality in severely injured patients. J Korean Soc Emerg Med 2016; 27(2):199-205. [ Google Scholar]
- Tansley G, Schuurman N, Bowes M, Erdogan M, Green R, Asbridge M. Effect of predicted travel time to trauma care on mortality in major trauma patients in Nova Scotia. Can J Surg 2019; 62(2):123-30. doi: 10.1503/cjs.004218 [Crossref] [ Google Scholar]
- Tansley G, Schuurman N, Bowes M, Erdogan M, Green R, Asbridge M. Effect of predicted travel time to trauma care on mortality in major trauma patients in Nova Scotia. Can J Surg 2019; 62(2):123-30. doi: 10.1503/cjs.004218 [Crossref] [ Google Scholar]
- Galvagno SM Jr, Massey M, Bouzat P, Vesselinov R, Levy MJ, Millin MG. Correlation between the revised trauma score and injury severity score: implications for prehospital trauma triage. Prehosp Emerg Care 2019; 23(2):263-70. doi: 10.1080/10903127.2018.1489019 [Crossref] [ Google Scholar]
- Toloui A, Madani Neishaboori A, Rafiei Alavi SN, Gubari MIM, Zareie Shab Khaneh A, Karimi Ghahfarokhi M. The value of physiological scoring criteria in predicting the in-hospital mortality of acute patients; a systematic review and meta-analysis. Arch Acad Emerg Med 2021; 9(1):e60. doi: 10.22037/aaem.v9i1.1274 [Crossref] [ Google Scholar]