Int J Aging. 2024;2:e10.
doi: 10.34172/ija.2024.e10
Original Article
Burden of Chronic Obstructive Pulmonary Disease for 70-Year-old Adults and Older in Iran During 1990-2021
Reza Aletaha 1, 2  , Ali Shamekh 1
, Ali Shamekh 1  , Fatemeh Tahmasbi 1, Mark JM Sullman 3, 4, Shahnam Arshi 5, *
, Fatemeh Tahmasbi 1, Mark JM Sullman 3, 4, Shahnam Arshi 5, *  , Ali-Asghar Kolahi 5
, Ali-Asghar Kolahi 5 
Author information:
1Social Determinants of Health Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
2Neurosciences Research Center, Aging Research Institute, Tabriz University of Medical Sciences, Tabriz, Iran
3Department of Life and Health Sciences, University of Nicosia, Nicosia, Cyprus
4Department of Social Sciences, University of Nicosia, Nicosia, Cyprus
5Social Determinants of Health Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Abstract
Objectives:
To comprehensively examine the burden of chronic obstructive pulmonary disease (COPD) among Iranians aged 70 and above, with a focus on gender, age, and provincial differences from 1990 to 2021.
Design:
Systematic analysis.
Outcome measures:
Data were derived from the Global Burden of Disease study 2021. Estimates were provided as numbers and age-standardized rates per 100000, accompanied by their 95% uncertainty intervals (UIs).
Results:
In 2021, COPD had an age-standardized prevalence of approximately 16 thousand per 100000 among Iranians aged 70 and older (95% UI: 13–19 thousand per 100000). This rate increased by 65.2% compared to 1990, which was statistically significant. COPD also accounted for 8,084 deaths in the elderly population of Iran in 2021. Furthermore, the disability-adjusted life year (DALY) rate was 3834.7 per 100000 individuals, reflecting a 6.4% increase from 1990 to 2021. Tehran and Ilam recorded the highest and lowest point prevalence per 100000, at 116000 and 3400, respectively. From 1990 to 2021, every province in Iran experienced a statistically significant increase in age-standardized prevalence rates. In 2021, although men experienced slightly higher deaths and DALYs and women had more prevalent cases, the overall prevalence, mortality, and DALYs related to COPD demonstrated no significant differences between the sexes. Additionally, in 2021, the age-standardized prevalence, mortality, and DALYs attributable to COPD increased with advancing age.
Conclusions:
The burden of COPD among the elderly in Iran has increased since 1990, paralleling the growth of the elderly population and an increase in COPD-related risk factors. Implementing preemptive measures, raising public awareness, and enacting risk management policies can effectively curb the ongoing rise of COPD in Iran.
Keywords: Chronic obstructive pulmonary disease, Epidemiology, Burden of disease, Iran, Mortality, Prevalence, Disability-adjusted life years
Copyright and License Information
© 2024 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
The Bill and Melinda Gates Foundation, not involved in any way in the preparation of this manuscript, funded the GBD study. The Shahid Beheshti University of Medical Sciences (Grant No. 21411) supported the present report.
Please cite this article as follows: Aletaha R, Shamekh A, Tahmasbi F, JM Sullman M, Arshi S, Kolahi AA. Burden of chronic obstructive pulmonary disease for 70-year-old adults and older in Iran during 1990-2021. Int J Aging. 2024;2: e10. doi: 10.34172/ija.2024.e10
Introduction
Chronic obstructive pulmonary disease (COPD) is marked by an irreversible limitation of airflow, as outlined by the American Thoracic Society and European Respiratory Society. This progressive restriction is linked to an abnormal inflammatory response in the lungs triggered by harmful particles or gases.1 Although there is no definitive cure for this condition, good self-management techniques can substantially reduce the impact of the illness and enhance life quality.2
Among the identified risk factors for COPD, smoking, indoor biomass burning, low body mass index, childhood asthma, occupational dust exposure, and nutrition are the most notable.3 In addition to the typical complaints of dyspnea, wheezing, chest tightness, exhaustion, activity limitation, and coughing with or without sputum production, patients with COPD may also experience acute events, known as exacerbations, which are marked by increased respiratory symptoms, severely impacting their prognosis and health status. These exacerbations call for particular therapeutic and preventive measures.4 Furthermore, mental health issues such as anxiety and depression are frequently associated with COPD and can lead to a reduced quality of life, lower activity levels, more frequent exacerbations, and a higher risk of death.5
According to reports, there were 212.3 million cases of COPD in 2019,6 accounting for one in every ten adults worldwide. This disease is also among the top three causes of death among the elderly worldwide.6-8 While the global age-standardized point prevalence of COPD has declined, the burden in the MENA region has increased.8,9 The increasing numbers of COPD patients can be attributed to growing and aging populations, as well as longer life expectancies.8,9 The global disability-adjusted life year (DALY) rate for COPD rises with age in both sexes, nonetheless, it remains consistently higher in men across all age groups.8
The economic burden of COPD is substantial. In 2017, the macroeconomic impact in the MENA region and Iran estimated at 103 billion and 14.45 billion dollars, respectively.10 Projections indicate that COPD will cost the global economy 4.326 trillion dollars between 2020 and 2050.10 The economic burden is primarily attributed to hospitalization and medication costs, which are significantly affected by the disease’s progression, the severity of acute exacerbations, and their frequency.11,12
The burden of COPD is expected to increase in the coming years due to ongoing exposure to risk factors, advancements in neonatal and pediatric care, and an aging population.13 In the MENA region, COPD-related deaths and DALY rates are steadily rising with age in both sexes. However, public awareness of this serious health issue remains limited, and health services have not prioritized this disease adequately enough.9,14 To effectively develop strategies for improving elderly health, optimizing resource allocation, and prioritizing interventions, it is essential to understand the patterns of disease burden within this age group.15 Previous research has documented the mortality and DALYs associated with COPD using data obtained from Global Burden of Disease (GBD) 2019.8 Another study examined the burden of COPD in the MENA region from 1990 to 2019.9 Additionally, research on the regional prevalence of COPD symptoms and healthcare utilization by COPD patients was conducted in 11 countries, 10 of which were in the MENA region.16 In Iran, the COPD-related burden has been estimated in a small number of studies.7,17-19 However, to the best of our knowledge, no prior study has employed modeling methods to assess the COPD burden in Iran’s elderly population. Consequently, the current study aimed to report the prevalence, deaths, and DALYs of COPD among Iranians aged 70 and older by age, sex, and province from 1990 to 2021.
Methods
Overview
GBD 2021 evaluated 371 diseases and injuries in 204 territories and countries from 1990 to 2021.20 This research provides data on the prevalence, mortality, and DALYs associated with COPD in Iran and its provinces over the same period. Details on the GBD 2021 methodology and advancements made since GBD 2019 have been previously described.20 Fatal and non-fatal estimates can be accessed using GBD Compare (https://vizhub.healthdata.org/gbd-compare/) and the GBD Results Tool (http://ghdx.healthdata.org/gbd-results-tool).
Case Definition and Data Sources
COPD is characterized as a chronic inflammatory lung condition that leads to airflow obstruction and breathing problems. It includes emphysema and chronic bronchitis. The Global Initiative for chronic obstructive lung disease (GOLD) classification defines this disease by a spirometry measurement showing a forced expiratory volume in one second/ the forced vital capacity (FEV1/FVC) ratio of less than 0.7 following bronchodilation. The severity of COPD is graded according to the GOLD classification as I: Mild [FEV1 score > 80% of normal], II: Moderate [FEV1 score 50–79% of normal], and III: Severe [FEV1 score < 50% of normal]. The International Classification of Diseases codes for COPD include ICD-10 codes J41, J42, J43, J44, and J47, as well as ICD-9 codes 491–492, and 496. In GBD 2017, J40 and 490 (unspecified bronchitis), as well as J47 and 494 (bronchiectasis), were removed from COPD mapping. Alternative case definitions for COPD, which differ from the GOLD post-bronchodilation standard, include GOLD pre-bronchodilation, the lower limit of normal post-bronchodilation, the lower limit of normal pre-bronchodilation, and European Respiratory Society guidelines. Each of these methods offers a different approach to assessing whether an individual has COPD.
Prevalence, incidence, and remission data from hospital claims data, the literature, proportion data of GOLD class severities, and Burden of Obstructive Lung Disease Study data were all gathered for the study. Data on the prevalence, incidence, and remission of COPD were obtained from the literature supplied by collaborators or found through a systematic review. All data included spirometry-based measures. Other data were collected from hospital claims data for non-fatal estimation and vital registrations for cause of death. When available, GOLD class proportions were sourced from the literature that provided information on disease severity. Our models estimated three distinct severities (mild, moderate, or severe), which were used to categorize COPD by severity in the modelling process. While a systematic literature review was not conducted for GBD 2021, additional data were incorporated from key survey series, GBD collaborators, and an opportunistic search in PubMed using a previous systematic review search string.
Data for estimating COPD mortality were drawn from vital registration and surveillance data within the Cause of Death (COD) database. Verbal autopsy data were excluded and instead mapped to a broader chronic respiratory disease model. Our outlier criteria excluded data points that (1) were implausibly high or low, (2) substantially conflicted with established age or temporal patterns, or (3) substantially conflicted with other data sources from the same or similar locations (e.g., those with a comparable socio-demographic index).
Data Processing and Disease Models
Non-fatal Modelling Strategy
In some cases, data were reported by only age or sex, but not both. For example, a study may have included the prevalence of males and females with COPD and then separately reported the prevalence for both sexes in smaller age bins (e.g., age groups of 70–74, 75–79, and the like). In such cases, an age-sex split was performed by using proportions within the study to disaggregate the data. When data could not be disaggregated into male and female categories for a given data source, instead a sex-split on the data was performed by applying sex proportions from other studies, including male- and female-specific data.
To improve guidance for disease model-Bayesian meta-regression on the expected pattern of electronic medical records, data from the previous round were used as inputs for modeling in meta-regression-Bayesian, regularized, trimmed. This modeling incorporated age, sex, healthcare access, and quality index as covariates. Meta-regression-Bayesian, regularized, trimmed results were predicted for each location by year, sex, and for ages 0, 10, 20, up to 100.
Fatal Modelling Strategy
The modelling approach in GBD 2021 remained largely unchanged. The standard COD ensemble modelling methodology was employed to calculate COPD-related deaths. Separate models were developed for male and female mortality, covering an age range from 15 to 95 + years.
Unadjusted death estimates from COPD were combined with those of other chronic respiratory diseases (asthma, interstitial lung disease, pulmonary sarcoidosis, and pneumoconiosis) and fitted to the distribution of deaths within an overall chronic respiratory disease envelope model as part of the CoDCorrect adjustment process. This approach allowed deaths recorded using non-specific coding systems, such as verbal autopsy, to be included in the parent model and proportionately redistributed to the child models.
Compilation of Results
For each estimate of prevalence, death, or DALY, 1000 draws were sampled, and the draws were summed across age, cause, and location for all intermediate calculations.20 This approach enabled us to capture and convey uncertainty throughout all computations. The 95% uncertainty intervals (UIs) were derived from the 2.5th and 97.5th percentiles of the sorted draws. Age was divided into several ranges (70–74, 75–79, 80–84, 85–89, 90–94, and 95 and above). R program (version 3.5.2) was used to generate plots for age-standardized point prevalence, mortality, and DALY rates.
Results
National Level
In 2021, COPD accounted for 592,442 cases (95% UI: 497 to 695 thousand) in the population aged ≥ 70 in Iran, with an age-standardized rate (ASR) of approximately 16 000 per 100 000 individuals (95% UI: 14 to 19 thousand per 100 000). The age-standardized prevalence rate (ASPR) rose by a statistically significant 65.2% (95% UI: 55.2 % to 75.9%) between 1990 and 2021 (Tables 1 and S1).
Table 1.
Prevalence, Deaths, and DALYs for COPD in Adults 70 Years and Older in Iran for Both Sexes in 2021 and the Percentage Change in the Age-Standardized Rates in 1990-2021
|
|
Prevalence (95% UI)
|
Deaths (95% UI)
|
DALYs (95% UI)
|
Counts
(2021)
|
Rate
(2021)
|
Pcs in Rate
1990-2021
|
Counts
(2021)
|
Rate
(2021)
|
Pcs in Rate
1990-2021
|
Counts
(2021)
|
Rate
(2021)
|
Pcs in Rate
1990-2021
|
| Iran |
592442
(497588, 695729) |
16223.9
(13626.4, 19052.4) |
65.2
(55.2, 75.9) |
8084
(6850, 8960) |
221.4
(187.6, 245.4) |
8.2
(-8.7, 39.5) |
140030
(122556, 153396) |
3834.7
(3356.2, 4200.7) |
6.4
(-8.3, 31.3) |
| Alborz |
16060
(13291, 18940) |
15335.9
(12691.9, 18086) |
61.4
(45.9, 79.1) |
204
(163, 245) |
194.8
(156.1, 234.4) |
-3.3
(-34.5, 30.2) |
3754
(3137, 4362) |
3584.5
(2995.2, 4165.7) |
-4
(-32, 24.8) |
| Ardebil |
9062
(7476, 10724) |
15471.2
(12763.5, 18308.1) |
72.2
(55.8, 89.9) |
91
(75, 107) |
155.2
(127.8, 183.1) |
36.2
(-0.8, 122.6) |
1735
(1492, 1989) |
2962.1
(2547.4, 3395.9) |
35.5
(4.2, 96.2) |
| Bushehr |
6032
(5010, 7138) |
15434.7
(12820, 18264.8) |
59.8
(43, 76.9) |
54
(43, 65) |
138.2
(111, 165.6) |
17.2
(-12.9, 71.1) |
1099
(948, 1255) |
2811.3
(2426.8, 3212.5) |
24
(-2.8, 63.9) |
| Chahar Mahaal and Bakhtiari |
6400
(5264, 7554) |
15614.8
(12842.8, 18430.2) |
48.7
(33.3, 63.6) |
54
(43, 67) |
130.6
(105.2, 163.9) |
-23.2
(-42.3, 19.3) |
1068
(915, 1271) |
2606.7
(2231.9, 3101.1) |
-16.5
(-33.6, 15.3) |
| East Azerbaijan |
32304
(26201, 38031) |
17543.5
(14229.3, 20653.8) |
69.6
(51.8, 93) |
685
(532, 819) |
371.8
(288.7, 445) |
10.2
(-16.4, 53.4) |
10853
(8858, 12716) |
5894.1
(4810.5, 6906) |
14.1
(-9.2, 53.5) |
| Fars |
34485
(28622, 40696) |
15577.9
(12929.2, 18383.4) |
68.5
(51.8, 85.2) |
404
(321, 499) |
182.6
(144.8, 225.6) |
38
(1.1, 99.7) |
7327
(6096, 8571) |
3309.8
(2753.5, 3871.9) |
31.8
(3.1, 75.7) |
| Gilan |
23968
(19643, 28159) |
15619.3
(12801, 18350.5) |
59.9
(44.2, 75.5) |
260
(220, 304) |
169.3
(143.1, 198.4) |
24.3
(-4.7, 67.7) |
4857
(4213, 5475) |
3165.2
(2745.7, 3567.9) |
23.6
(-0.4, 55.7) |
| Golestan |
10594
(8679, 12493) |
15491.8
(12691.7, 18268.7) |
79.8
(61.6, 98.5) |
132
(105, 160) |
193.7
(153.6, 233.3) |
94.1
(37.4, 205.9) |
2458
(2038, 2867) |
3594.8
(2979.6, 4192.3) |
72.7
(28.8, 142.1) |
| Hamadan |
16408
(13433, 19425) |
16956.3
(13881.9, 20074.6) |
79.1
(58.8, 101.9) |
180
(144, 215) |
185.8
(149.2, 222.7) |
17.4
(-14.6, 69.1) |
3305
(2823, 3817) |
3415.2
(2917.2, 3945) |
14
(-12.2, 52.3) |
| Hormozgan |
7119
(5833, 8514) |
13494.2
(11057.7, 16138.6) |
50.3
(37.3, 65.4) |
65
(53, 77) |
122.6
(101.2, 146.2) |
-3.9
(-27.3, 43.6) |
1253
(1074, 1438) |
2374.4
(2035.5, 2726.2) |
-3.3
(-22.9, 31) |
| Ilam |
3427
(2820, 4021) |
14984.2
(12329.8, 17583.9) |
48.7
(36.2, 62.8) |
31
(25, 38) |
134
(109.1, 165.9) |
11.3
(-16.2, 66.5) |
603
(512, 704) |
2639
(2238.4, 3078.7) |
14.4
(-8, 52.3) |
| Isfahan |
43896
(36357, 52044) |
17145.9
(14201.3, 20328.7) |
71.5
(56.2, 88.6) |
533
(425, 650) |
208.1
(166, 254.1) |
15.6
(-14.6, 63.8) |
9495
(7950, 11197) |
3708.8
(3105.4, 4373.8) |
14.1
(-11.4, 52.3) |
| Kerman |
20574
(16968, 24075) |
18287.3
(15082.4, 21399.7) |
80.6
(62.1, 101.8) |
586
(430, 694) |
521.2
(382.5, 617) |
53.8
(16.5, 108.8) |
8868
(6827, 10444) |
7882.6
(6068.2, 9283.4) |
33
(1.8, 75.6) |
| Kermanshah |
16065
(13244, 19208) |
16417.1
(13534, 19628.3) |
60.6
(44.5, 79.9) |
235
(192, 286) |
240.5
(196.1, 292) |
-16
(-37.6, 17.7) |
4066
(3438, 4806) |
4155.2
(3513.6, 4910.8) |
-16.2
(-34.5, 13.2) |
| Khorasan-e-Razavi |
47331
(39015, 55466) |
17748.5
(14630.1, 20799.1) |
84.3
(63.5, 109.9) |
881
(664, 1035) |
330.5
(249, 388) |
47.5
(11.5, 109.7) |
14392
(11749, 16345) |
5396.8
(4405.6, 6129.2) |
32.9
(3.8, 80) |
| Khuzestan |
26252
(21653, 31333) |
15944
(13151, 19030.2) |
47.2
(35.8, 60) |
255
(204, 298) |
155.1
(123.8, 181) |
-25.3
(-41.1, 0.6) |
4950
(4186, 5650) |
3006.5
(2542.3, 3431.5) |
-17.1
(-31.8, 6.3) |
| Kohgiluyeh and Boyer-Ahmad |
4093
(3393, 4838) |
14823.9
(12288.4, 17522.4) |
45.8
(33.5, 59.4) |
27
(21, 34) |
96.3
(74.9, 123.9) |
-12
(-39.2, 54.1) |
573
(478, 692) |
2075.6
(1731.7, 2505.3) |
-4.6
(-27.9, 37.1) |
| Kurdistan |
12368
(10207, 14508) |
15883.2
(13107.9, 18630.3) |
63.6
(45.2, 85.6) |
145
(117, 182) |
186.3
(150.4, 233.4) |
-9.3
(-37.1, 38.3) |
2641
(2237, 3120) |
3391.4
(2872.7, 4006.3) |
-7
(-31.2, 32) |
| Lorestan |
10937
(8946, 13044) |
15254.6
(12478.3, 18194.8) |
57.3
(42.9, 71.7) |
98
(80, 122) |
136.9
(111.7, 169.9) |
-10.4
(-35.5, 40.5) |
1995
(1674, 2381) |
2782.3
(2334.9, 3320.7) |
-3.1
(-27.3, 38.5) |
| Markazi |
14777
(12339, 17286) |
17472.7
(14589.1, 20438.6) |
77.9
(62.8, 94.5) |
179
(140, 217) |
211.7
(165.6, 257.1) |
3
(-23.5, 47.7) |
3078
(2560, 3601) |
3639.9
(3027.3, 4257.7) |
3.3
(-20.7, 40.1) |
| Mazandaran |
28691
(23658, 34123) |
15667.5
(12918.9, 18633.6) |
62.9
(48, 78.5) |
242
(194, 295) |
132.1
(106, 160.9) |
2.6
(-23, 47) |
4832
(4090, 5694) |
2638.4
(2233.4, 3109.2) |
8.5
(-13.4, 41) |
| North Khorasan |
5791
(4729, 6872) |
16360.5
(13360.7, 19415.5) |
80.1
(61.2, 104.8) |
84
(67, 100) |
238.1
(189.4, 281.2) |
29.5
(-8.2, 92.4) |
1486
(1227, 1714) |
4197.2
(3468.1, 4843) |
22.3
(-9.8, 70.9) |
| Qazvin |
8836
(7246, 10392) |
16233.3
(13312.4, 19092) |
73.3
(56.7, 92.6) |
114
(94, 135) |
209.9
(173, 248.1) |
25.2
(-5.3, 79.5) |
2043
(1751, 2339) |
3754.1
(3216.8, 4297) |
21.7
(-4.9, 65.5) |
| Qom |
8212
(6892, 9626) |
16406.6
(13768.9, 19231.2) |
59.5
(44.5, 75.1) |
129
(106, 155) |
258.2
(211.4, 310) |
-15.4
(-35.3, 24.9) |
2164
(1851, 2559) |
4323.1
(3698.1, 5112.9) |
-14.3
(-32.9, 22.2) |
| Semnan |
5797
(4806, 6848) |
16668.2
(13817.3, 19689.9) |
72
(54.1, 87.1) |
74
(59, 89) |
213.3
(170.7, 254.9) |
6
(-19.8, 47.7) |
1325
(1117, 1535) |
3808.5
(3210.7, 4413.9) |
4.6
(-17.9, 39.3) |
| Sistan and Baluchistan |
11659
(9553, 13672) |
16865.6
(13819.7, 19777.9) |
60.7
(43.9, 81.1) |
224
(162, 276) |
324.7
(233.9, 399.1) |
-17.8
(-38.5, 16.3) |
3720
(2872, 4457) |
5381.5
(4155, 6446.8) |
-22.6
(-41.6, 4.4) |
| South Khorasan |
7596
(6276, 8828) |
18433.3
(15231.6, 21424.9) |
78.5
(58.4, 104) |
118
(89, 141) |
286.7
(216, 342.1) |
24.5
(-8, 93.9) |
1949
(1593, 2273) |
4729.4
(3865.1, 5516.2) |
17
(-10.6, 70.1) |
| Tehran |
116701
(97488, 140196) |
15311.8
(12791, 18394.6) |
59.1
(45.7, 75.4) |
1397
(1109, 1735) |
183.3
(145.5, 227.6) |
-4.9
(-32.2, 34.8) |
24062
(20224, 28415) |
3157.1
(2653.5, 3728.2) |
-4.5
(-29.4, 27.7) |
| West Azerbaijan |
19649
(16358, 23116) |
16430.3
(13678.7, 19329.6) |
59.7
(42.6, 77.7) |
333
(269, 395) |
278.7
(225.2, 330) |
-5.1
(-26.5, 28.4) |
5561
(4606, 6425) |
4650.3
(3852, 5372.9) |
-3.1
(-23.3, 27.3) |
| Yazd |
8444
(7009, 9938) |
18048.5
(14980.5, 21240.4) |
71.7
(54, 88.5) |
138
(109, 165) |
295
(232.4, 353.2) |
10.5
(-18.3, 48) |
2270
(1883, 2661) |
4852
(4025.6, 5687.6) |
4.8
(-19.9, 35.2) |
| Zanjan |
8914
(7457, 10399) |
16992.9
(14215, 19822) |
69.8
(51.4, 92.2) |
131
(106, 152) |
249.2
(201.5, 290.5) |
9.5
(-15.8, 44.1) |
2248
(1908, 2562) |
4284.7
(3637.7, 4884.4) |
6.1
(-17, 34.9) |
Note. DALY: Disability-adjusted life years; COPD: Chronic obstructive pulmonary disease; UI: Uncertainty interval; PCs: Percentage changes.
Source. Generated from data available from http://ghdx.healthdata.org/gbd-results-tool.
The COPD-related death toll reached 8084 cases (95% UI: 6850 to 8960), with an age-standardized death rate (ASDR) of 221.4 per 100 000 (95% UI: 187.6 to 245.4). There was an 8.2% increase in the ASDR from 1990 to 2021 (95% UI: -8.7 to 39.5), but this change was not statistically significant (Tables 1 and S2).
In 2021, the population aged 70 and older in Iran experienced approximately 140,000 DALYs (95% UI: 122 to 153 thousand), with an ASR of 3834.7 per 100 000 (95% UI: 3356.2 to 4200.7). Over the specified timespan, the ASR of DALYs increased by 6.4% (95% UI: -8.3 to 31.3), which was not statistically significant (Tables 1 and S3).
Provincial Level
At the provincial level, Tehran had the highest prevalence of COPD in 2021 [116 thousand (95% UI: 97 to 140 thousand)], followed by Khorasan-e-Razavi [47 thousand (95% UI: 39 to 55 thousand)], and Isfahan [43 thousand (95% UI: 36 to 52 thousand)]. The smallest number of prevalent cases were reported in Ilam [3.4 thousand (95% UI: 2.8 to 4.0 thousand)], Kohgiluyeh and Boyer-Ahmad [4.0 thousand (95% UI: 3.3 to 4.8 thousand)], and North Khorasan [4.7 thousand (95% UI: 4.7 to 6.8 thousand)].
The ASPRs were the highest in South Khorasan [18433.3 (95% UI: 15231.6 to 21424.9)], Kerman [18287.3 (95% UI: 15082.4 to 21399.7)], and Yazd [18048.5 (95% UI: 14980.5 to 21240.4)], while the lowest rates were in Hormozgan [13494.2 (95% UI: 11057.7 to 16138.6)], Kohgiluyeh and Boyer-Ahmad [14823.9 (95% UI: 12288.4 to 17522.4)], and Ilam [14984.2 (95% UI: 12329.8 to 17583.9)] (Figure 1A and Table S1).
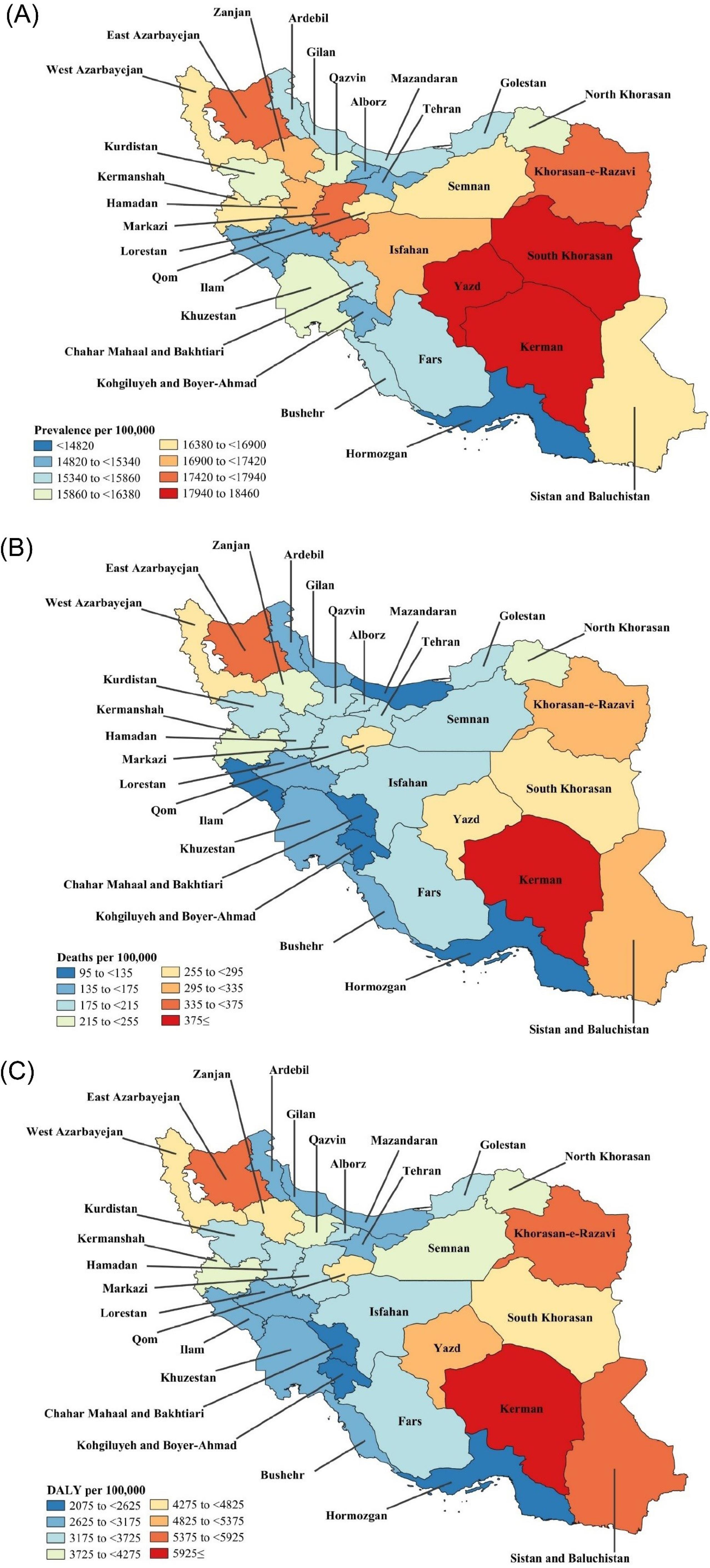
Figure 1.
(A) Point Prevalence, (B) Deaths, and (C) DALY Rates for COPD (per 100 000 Population) for Adults 70 Years and Older in Iran in 2021 by Province. Note. DALY: Disability-adjusted life years; COPD: Chronic obstructive pulmonary disease. Source. Generated from data available from http://ghdx.healthdata.org/gbd-results-tool.
.
(A) Point Prevalence, (B) Deaths, and (C) DALY Rates for COPD (per 100 000 Population) for Adults 70 Years and Older in Iran in 2021 by Province. Note. DALY: Disability-adjusted life years; COPD: Chronic obstructive pulmonary disease. Source. Generated from data available from http://ghdx.healthdata.org/gbd-results-tool.
Furthermore, all provinces experienced a statistically significant increase in ASPRs over the 1990-2021 timespan, of which Khorasan-e-Razavi [84.3% (95% UI: 63.5 % to 109.9%)], Kerman [80.6% (95% UI: 62.1% to 101.8%)], and North Khorasan [80.1% (95% UI: 61.2% to 104.8%)] had the largest increases. The ASPR per 100,000 population did not exhibit any significant sex differences over the evaluated timespan (Figure S1).
In 2021, among the population aged 70 and older in Iran’s provinces, the highest COPD-related death rates were observed in Tehran [1397 (95% UI: 1109 to 1735)], Khorasan-e-Razavi [881 (95% UI: 664 to 1035)], and East Azarbayejan [685 (95% UI: 532 to 819)]. Conversely, the lowest rates were found in Kohgiluyeh and Boyer-Ahmad [27 (95% UI: 21 to 34)], Ilam [31 (95% UI: 25 to 38)], and Bushehr [54 (95% UI: 43 to 65)].
Additionally, the ASDR per 100 000 was highest in Kerman [521.2 (95% UI: 382.5 to 617)], East Azarbayejan [371.8 (95% UI: 288.7 to 445)], and Khorasan-e-Razavi [330.5 (95% UI: 249 to 388)], while this rate was lowest in Kohgiluyeh and Boyer-Ahmad [96.3 (95% UI: 74.9 to 123.9)], Hormozgan [122.6 (95% UI: 101.2 to 146.2)], and Chahar Mahaal and Bakhtiari [130.6 (95% UI: 105.2 to 163.9)] (Figure 1B and Table S2).
From 1990 to 2021, the ASDR showed statistically significant changes in five provinces: Golestan [94.1% (95% UI: 37.4 % to 205.9%)], Zanjan [68.7% (95% UI: 1.6% to 127.8%)], Kerman [53.8% (95% UI: 16.5% to 108.8%)], Khorasan-e-Razavi [47.5% (95% UI: 11.5% to 109.7%)], and Fars [38% (95% UI: 1.1 % to 99.7%)]. On the other hand, in 2021 no significant differences were observed between the sexes across the provinces (Figure S2).
In 2021, the highest rates of COPD-induced DALYs were recorded in Tehran [24062 (95% UI: 20224 to 28415)], Khorasan-e-Razavi [14392 (95% UI: 11749 to 16345)], and East Azarbayejan [10853 (95% UI: 8858 to 12716)]. Conversely, the lowest numbers were observed in Kohgiluyeh and Boyer-Ahmad [573 (95% UI: 478 to 692)], Ilam [603 (95% UI: 512 to 704)], and Chahar Mahaal and Bakhtiari [1068 (95% UI: 915 to 1271)]. The ASR of DALYs due to COPD were highest in Kerman [7882.6 (95% UI: 6068.2 to 9283.4)], East Azarbayejan [5894.1 (95% UI: 4810.5 to 6906)], and Khorasan-e-Razavi [5396.8 (95% UI: 4405.6 to 6129.2)]. The lowest ASR was found in Kohgiluyeh and Boyer-Ahmad [2075.6 (95% UI: 1731.7 to 2505.3)], Hormozgan [2374.4 (95% UI: 2035.5 to 2726.2)], and Chahar Mahaal and Bakhtiari [2606.7 (95% UI: 2231.9 to 3101.1)] (Figure 1C and Table S3).
From 1990 to 2021, there were statistically significant increases in the ASRs of COPD-induced DALYs Golestan [72.7% (95% UI: 28.8 % to 142.1%)], Ardebil [35.5% (95% UI: 4.2 % to 96.2%)], Kerman [33% (95% UI: 1.8 % to 75.6%)], Khorasan-e-Razavi [32.9% (95% UI: 3.8 % to 80%)], and Fars [31.8% (95% UI: 3.1 % to 75.7%)] provinces. Similar to prevalence and deaths, no significant differences were noted between sexes in the ASR of DALYs across Iran’s provinces (Figure S3).
Age and Sex Patterns
In 2021, the highest number of prevalent cases occurred in the 70-74 age group, with a gradual decline in cases observed with an increase in age. The ASPR per 100 000 population increased linearly as the population aged, peaking at the population age ≥ 95 (Figure 2A). Overall, women had a greater prevalence of cases compared to men, while men only had a larger prevalence in the ≥ 90 age range, but these differences were not statistically significant. Furthermore, from 1990 to 2021, there were no significant changes in COPD prevalence rates for either sex across the Iranian provinces (Figure S4).
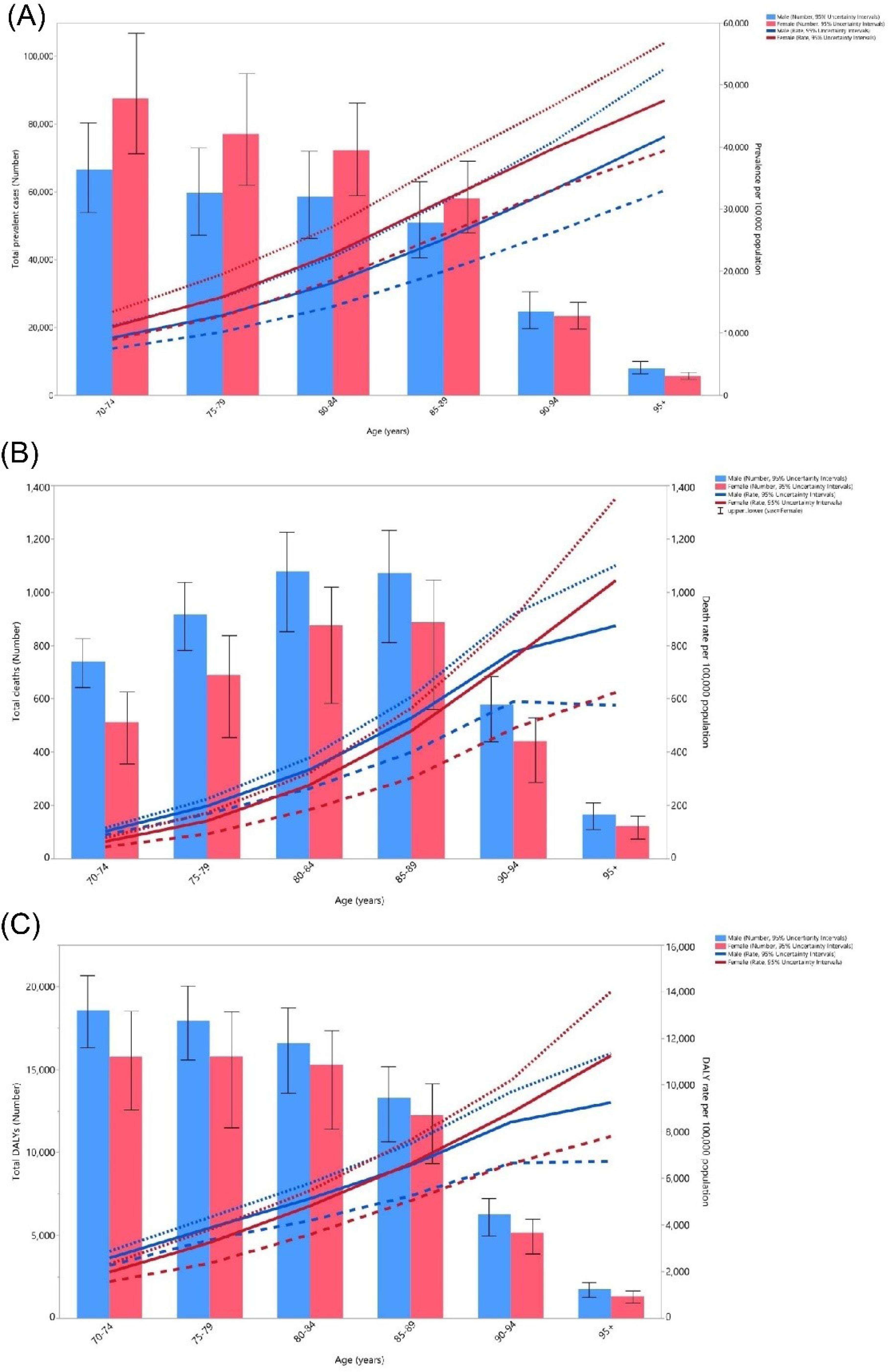
Figure 2.
(A) Number of Prevalent Cases and Prevalence, (B) Number of Deaths and Death Rate, and (C) Number of DALYs and DALY Rate for COPD (per 100 000 Population) in Iran in 2021 by Age and Sex. Note. UI: Uncertainty interval; DALY: Disability-adjusted life years; COPD: Chronic obstructive pulmonary disease. Dotted and dashed lines indicate 95% upper and lower UIs, respectively. Source. Generated from data available from http://ghdx.healthdata.org/gbd-results-tool.
.
(A) Number of Prevalent Cases and Prevalence, (B) Number of Deaths and Death Rate, and (C) Number of DALYs and DALY Rate for COPD (per 100 000 Population) in Iran in 2021 by Age and Sex. Note. UI: Uncertainty interval; DALY: Disability-adjusted life years; COPD: Chronic obstructive pulmonary disease. Dotted and dashed lines indicate 95% upper and lower UIs, respectively. Source. Generated from data available from http://ghdx.healthdata.org/gbd-results-tool.
In 2021, COPD-related deaths in the ≥ 70 Iranian population increased with the advancement of age, peaked at 85–89, and then began to drop in the ≥ 90 age range, with men showing greater mortality rates in all the groups. The ASDR per 100 000 increased as the advancing age and peaked in the ≥ 95 age group. Notably, the ASDR for females began to pass that of males starting in the ≥ 90 age group (Figure 2B).
With the exception of the 70–74 age group, where men had significantly higher death numbers, no statistically significant differences in death numbers and rates were observed between sexes across other age groups (Figure 2B). At the province level, there were no significant sex disparities in changes in mortality rates from 1990 to 2021 (Figure S5).
In 2021, the COPD-related DALYs peaked in the 70–74 age group for both sexes, followed by a gradual decline with aging. Although there was a general pattern of higher DALYs among males across all the age groups, the ASR DALYs for women surpassed that of men in the 85–89 age group. Furthermore, the overall ASR of DALYs rose with age, peaking in the ≥ 95 age group (Figure 2C). Moreover, from 1990 to 2021, there were no significant sex differences in DALY rates due to COPD at the provincial level in Iran, mirroring the trends observed in prevalence and mortality rates (Figure S6).
Comparison to the MENA Region
Figure 3 depicts the Iran/MENA ratio of COPD-related DALY rates per 100 000 population, indicating that Iran had lower DALY rates for both men and women compared to the MENA region, with women’s rates being closer to the MENA average than men’s rates. For men, the ratios were similar across most age groups in 1990 and 2021, with the exception of the 80–84 age group, which exhibited higher rates in 2021 compared to 1990. In women, the ratios were higher in 2021 in the 70–74, 75–79, and 80–84 age groups, while other age groups maintained the same ratio in both 1990 and 2021.
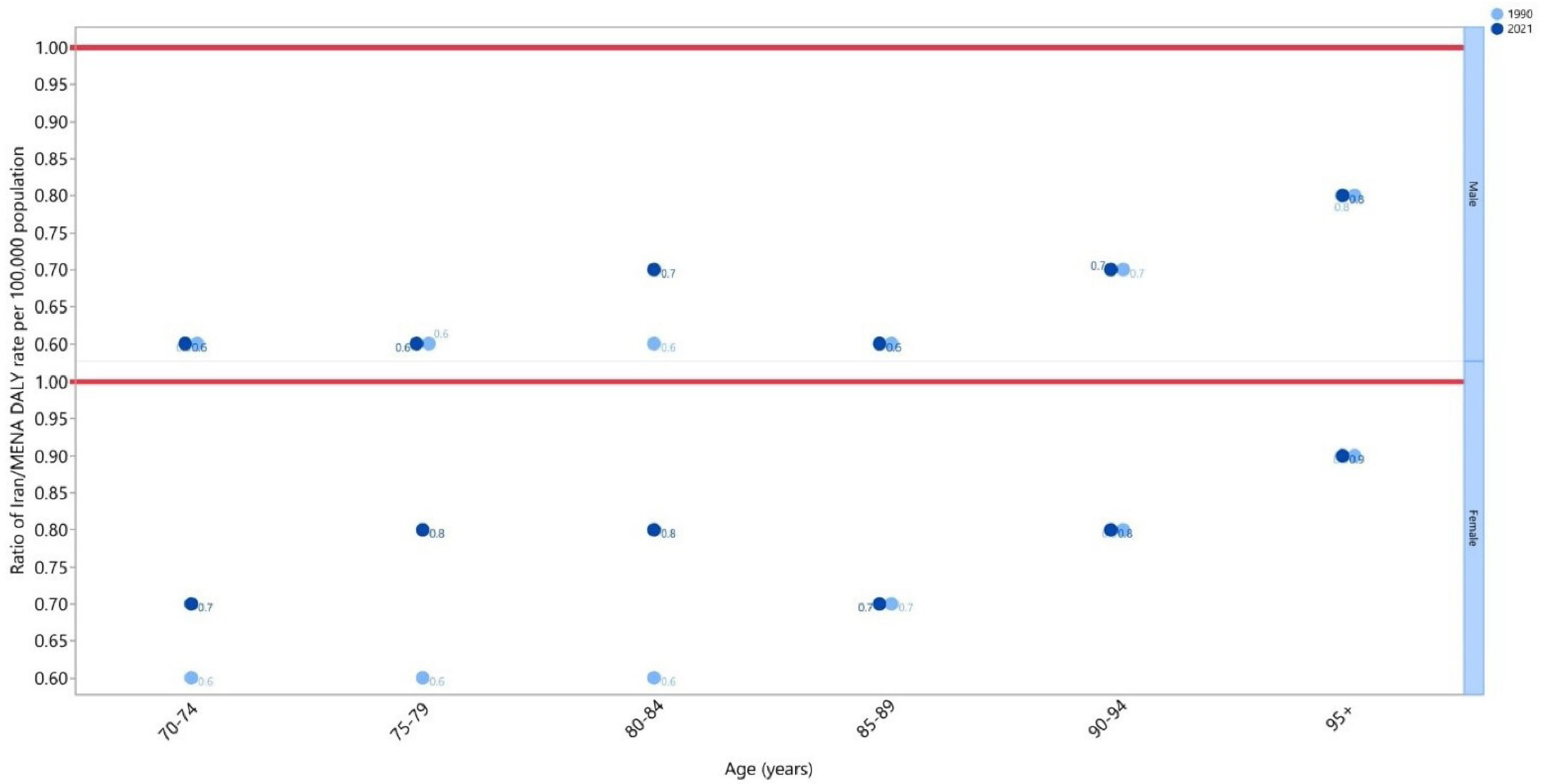
Figure 3.
Ratio of COPD’s DALY Rate of Iran’s Elderly ( ≥ 70 Years Old) to the Middle East and North Africa Region According to Age Group and Sex (1990–2021)
Note. DALY: Disability-adjusted life years; COPD: Chronic obstructive pulmonary disease. Source. Generated from data available from http://ghdx.healthdata.org/gbd-results-tool.
.
Ratio of COPD’s DALY Rate of Iran’s Elderly ( ≥ 70 Years Old) to the Middle East and North Africa Region According to Age Group and Sex (1990–2021)
Note. DALY: Disability-adjusted life years; COPD: Chronic obstructive pulmonary disease. Source. Generated from data available from http://ghdx.healthdata.org/gbd-results-tool.
Discussion
The current study assessed the incidence, prevalence, and DALYs attributable to COPD, along with their respective rates, for Iranians aged 70 and older across different provinces from 1990 to 2021, using data from the GBD 2021. In 2021, there were 592 442 prevalent cases of COPD, 8084 deaths, and 140 thousand DALYs among Iranians in this age group.
A previous study examining the impact of COPD in the MENA region from 1990 to 2019 revealed a 30.6% increase in the age-standardized point prevalence of COPD. During the same period, the age-standardized rates for mortality and DALYs declined by 18% and 11.8%, respectively. Our findings are consistent with those of the previous study regarding point prevalence but differ in terms of mortality and DALY rates. While the rise in mortality and DALY rates observed in our study may indicate future trends, it was not statistically significant overall 9. Nonetheless, the statistically significant rise in deaths and DALY rates in some provinces, such as Golestan and Fars, should be considered a serious warning.
Prior investigations in Iran have reported COPD prevalence rates ranging from 1.68% to 10%.7,17,21-24 However, our study differs from earlier research in several ways, including a larger sample size. Other factors contributing to discrepancies include the year of study, diagnostic standards used, and the sample sizes, as well as whether studies were conducted at a subnational or national level and the applied methodologies. As a result, our findings and those of other studies on the burden of COPD are not directly comparable. This is due to the use of different standards in defining COPD, interpreting spirometry data, and the inclusion or exclusion of bronchodilator inhalation.12 For instance, a 2015 systematic review reported a total COPD prevalence of 5.57% across all age groups in Iran, which is extremely lower than our findings. This discrepancy may be attributed to differences in the definitions of COPD, as the review only reported the prevalence of chronic bronchitis.17
In contrast to the prevalence rate, the estimated mortality and DALY rates linked to COPD in Iran’s elderly population were notably higher than the global and regional rates observed in the general population. In 2019, the global death and DALY rates per 100 000 were 42.5 and 926.1, respectively, while in the MENA region, they were 26.1 and 649.1. These figures are considerably lower than the estimates presented in this research.8,9 This discrepancy may be attributed to the correlation between age and COPD mortality rates, which tend to rise as the population ages.9,25 Other contributing factors include increased life expectancy and a lack of epidemiological data on the prevalence and risk factors of COPD in developing countries, particularly in Iran. Previous research indicates that COPD is underdiagnosed in Iran.22 This underestimation may result from the absence of a coherent registration system, inaccurate diagnoses, or the omission of mild cases, as patients often seek medical care only when their condition worsens.
The present investigation also revealed that the 70–74 age group had the largest number of prevalent cases, with a progressive decline noted with increasing age. This trend may be explained by the smaller population size in the older age brackets. Furthermore, this research revealed that the ASDR per 100 000 individuals rose as age grew and peaked for both sexes in the 95 and older age group. In accordance with our findings, a prior investigation demonstrated that the mortality rate of COPD increased with increasing age.25
The DALY rates in Iran are lower than the regional rates per 100 000, despite the fact that the prevalence of COPD in the geriatric population is higher than in other MENA countries. This discrepancy may be due to Iran’s higher health coverage index and/or a lower age-standardized prevalence of tobacco use compared to the rest of the MENA region, as smoking is the primary risk factor for COPD.23,26 Understanding the reasons behind this phenomenon requires controlling many confounding factors, such as the efficacy of regional healthcare systems and the presence of comorbidities.
Industrialized cities such as Tehran, Khorasan-e-Razavi, and Isfahan had a larger number of prevalent COPD cases. Nevertheless, the ASPRs were greater in South Khorasan and Kerman. The higher rate of opium use in these regions, compared to Iran’s overall population, may account for the elevated ASPRs, as opium users are more likely to have COPD and other respiratory diseases.27,28 Furthermore, East Azarbayejan, Khorasan-e-Razavi, and Tehran had greater rates of COPD-related deaths and DALYs. In contrast, provinces such as Kohgiluyeh and Boyer-Ahmad, Ilam, and Chahar Mahaal and Bakhtiari showed lower rates of COPD-related deaths, prevalence, and DALYs than other provinces. The higher rates in the more industrialized areas might be attributed to the larger populations and more polluted air compared to less urbanized areas.29,30
Consistent with our findings, data from Sharifi et al indicated that among the five cities—Tehran, Ahvaz, Mazandaran, Mashhad, and Kerman—Kerman had the highest prevalence of COPD in the general population, followed by Tehran.21 Furthermore, exposure to biomass fuels, commonly used for cooking and heating in poorly ventilated homes, is considered a risk factor for COPD in rural settings due to the high levels of particulate matter in indoor air.31-34 While air pollution is typically more severe in urban areas compared to rural ones, the prevalence of COPD may decrease with global urbanization. This trend is due to more households transitioning from traditional cooking methods in badly ventilated homes to using gas or electric cooking in better-ventilated environments.35 In addition, as developing nations modernize their air-polluting industries, outdoor air pollution is either improving or staying the same.36
Our findings revealed a higher prevalence of COPD cases among women compared to men in the geriatric population, which contrasts with prior research.8,9,21 However, the model used in the study by Feenstra et al predicted that the burden of COPD would inescapably rise in the coming years, affecting women more severely than men.37 A subsequent study supported this forecast, revealing that the prevalence of COPD among females is expected to rise from 7.8% in 2020 to 8.3% in 2050, reflecting a relative increase of 6.4%.38 This discrepancy may be attributed to women’s longer life expectancy compared to men.39 Moreover, while global and regional smoking trends are declining, the prevalence of smokers in Iran has increased, particularly among women, which is significant given that smoking is a key risk factor for COPD.23,40 An emerging body of research suggests that, given equal exposure, women might be more vulnerable to risk factors than men.37,41 In developing countries, women are also more susceptible to exposure to elevated indoor air pollution levels than men. This is evident from the fact that 80% of nonsmoker patients with COPD are women, likely due to their exposure to biomass fuels.42,43
The findings of this study confirmed that the overall burden of COPD has increased over the past 30 years. This highlights the need for performing prompt interventions such as implementing smoking cessation programs, reducing air pollution levels by controlling industrial and traffic exhaust, increasing awareness about the disease and its possible risk factors, and providing better healthcare coverage for underserved populations.
Strengths and Limitations
This study has provided the most current information on the burden of COPD among Iranians aged 70 and above from 1990 to 2021. Nevertheless, this study has several limitations. First, the limited availability of COPD data in Iran, a challenge also noted in other GBD studies, may have impacted the accuracy and reliability of the data and subsequent estimates. In addition, it was impossible to look into additional significant spirometry-based questions, as the analyses presented in this paper relied on the data provided by the GBD project. Further, the burden of COPD was not broken down by the racial or ethnic group or by kind of habitation (rural vs. urban). Further research is needed to report data regarding the area of residency, which could help policymakers implement more precise and effective measures.
Conclusions
From 1990 to 2021, the age-standardized prevalence, mortality, and DALY rates of COPD have increased, making it a leading cause of mortality and morbidity among Iran’s elderly population. To lower the incidence of new COPD cases, policymakers and health systems should focus on mitigating risk factors, enhancing diagnostic accuracy, and improving care for current patients. This approach is crucial, as COPD significantly contributes to deaths and DALYs among the elderly. Further research is required to more accurately quantify the prevalence and burden of this condition.
Acknowledgments
We would like to thank the Institute for Health Metrics and Evaluation staff and its collaborators who prepared these publicly available data. This study is based on publicly available data and solely reflects the opinions of its authors and not that of the Institute for Health Metrics and Evaluation.
Author contributions
Conceptualization: Shahnam Arshi, Ali-Asghar Kolahi.
Formal analysis: Reza Aeltaha.
Funding acquisition: Ali-Asghar Kolahi.
Investigation:Ali-Asghar Kolahi.
Methodology:Ali-Asghar Kolahi.
Project administration: Shahnam Arshi.
Software: Ali Shamekh.
Supervision: Shahnam Arshi.
Validation: Ali Shamekh.
Visualization: Ali Shamekh.
Writing–original draft: Reza Aletaha, Ali Shamekh, Fatemeh Tahmasbi, Mark JM Sullman, Shahnam Arshi, Ali-Asghar Kolahi.
Writing–review & editing: Reza Aletaha, Ali Shamekh, Fatemeh Tahmasbi, Mark JM Sullman, Shahnam Arshi, Ali-Asghar Kolahi.
Data availability statement
The data used for these analyses are all publicly available at http://ghdx.healthdata.org/gbd-results-tool.
Ethical approval
The present study was reviewed and approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran (Ethics code: IR.SBMU.RETECH.REC.1401.688).
Consent for publication
Not applicable.
Conflict of interests
None declared.
Supplementary Files
Supplementary files contain Tables S1-S3 and Figures S1-S6.
(pdf)
References
- Celli BR, MacNee W. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J 2004; 23(6):932-46. doi: 10.1183/09031936.04.00014304 [Crossref] [ Google Scholar]
- Cannon D, Buys N, Sriram KB, Sharma S, Morris N, Sun J. The effects of chronic obstructive pulmonary disease self-management interventions on improvement of quality of life in COPD patients: a meta-analysis. Respir Med 2016; 121:81-90. doi: 10.1016/j.rmed.2016.11.005 [Crossref] [ Google Scholar]
- Holtjer JC, Bloemsma LD, Beijers R, Cornelissen MEB, Hilvering B, Houweling L. Identifying risk factors for COPD and adult-onset asthma: an umbrella review. Eur Respir Rev 2023; 32(168):230009. doi: 10.1183/16000617.0009-2023 [Crossref] [ Google Scholar]
- Global Initiative for Chronic Obstructive Lung Disease. 2024 GOLD Report. Global Initiative for Chronic Obstructive Lung Disease; 2024.
- Smith MC, Wrobel JP. Epidemiology and clinical impact of major comorbidities in patients with COPD. Int J Chron Obstruct Pulmon Dis 2014; 9:871-88. doi: 10.2147/copd.s49621 [Crossref] [ Google Scholar]
- Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380(9859):2095-128. doi: 10.1016/s0140-6736(12)61728-0 [Crossref] [ Google Scholar]
- Sharifi H, Ghanei M, Jamaati H, Masjedi MR, Aarabi M, Sharifpour A. Burden of obstructive lung disease in Iran: prevalence and risk factors for COPD in North of Iran. Int J Prev Med 2020; 11:78. doi: 10.4103/ijpvm.IJPVM_478_18 [Crossref] [ Google Scholar]
- Safiri S, Carson-Chahhoud K, Noori M, Nejadghaderi SA, Sullman MJ, Ahmadian Heris J. Burden of chronic obstructive pulmonary disease and its attributable risk factors in 204 countries and territories, 1990-2019: results from the Global Burden of Disease Study 2019. BMJ 2022; 378:e069679. doi: 10.1136/bmj-2021-069679 [Crossref] [ Google Scholar]
- Feizi H, Alizadeh M, Nejadghaderi SA, Noori M, Sullman MJ, Ahmadian Heris J. The burden of chronic obstructive pulmonary disease and its attributable risk factors in the Middle East and North Africa region, 1990-2019. Respir Res 2022; 23(1):319. doi: 10.1186/s12931-022-02242-z [Crossref] [ Google Scholar]
- Chen S, Kuhn M, Prettner K, Yu F, Yang T, Bärnighausen T. The global economic burden of chronic obstructive pulmonary disease for 204 countries and territories in 2020-50: a health-augmented macroeconomic modelling study. Lancet Glob Health 2023; 11(8):e1183-93. doi: 10.1016/s2214-109x(23)00217-6 [Crossref] [ Google Scholar]
- ur Rehman R, Ahmad Hassali MA, Muhammad SA, Shah S, Abbas S, Hyder Ali IA. The economic burden of chronic obstructive pulmonary disease (COPD) in the USA, Europe, and Asia: results from a systematic review of the literature. Expert Rev Pharmacoecon Outcomes Res 2020; 20(6):661-72. doi: 10.1080/14737167.2020.1678385 [Crossref] [ Google Scholar]
- López-Campos JL, Tan W, Soriano JB. Global burden of COPD. Respirology 2016; 21(1):14-23. doi: 10.1111/resp.12660 [Crossref] [ Google Scholar]
- Safiri S, Motlagh Asghari K, Sullman MJM. The global burden of diseases and injuries among older adults. Int J Aging 2023; 1:e16. doi: 10.34172/ija.2023.e16 [Crossref] [ Google Scholar]
- Halpin DM, Celli BR, Criner GJ, Frith P, López Varela MV, Salvi S. The GOLD Summit on chronic obstructive pulmonary disease in low- and middle-income countries. Int J Tuberc Lung Dis 2019; 23(11):1131-41. doi: 10.5588/ijtld.19.0397 [Crossref] [ Google Scholar]
- Michel JP, Sadana R. “Healthy aging” concepts and measures. J Am Med Dir Assoc 2017; 18(6):460-4. doi: 10.1016/j.jamda.2017.03.008 [Crossref] [ Google Scholar]
- Tageldin MA, Nafti S, Khan JA, Nejjari C, Beji M, Mahboub B. Distribution of COPD-related symptoms in the Middle East and North Africa: results of the BREATHE study. Respir Med 2012; 106 Suppl 2:S25-32. doi: 10.1016/s0954-6111(12)70012-4 [Crossref] [ Google Scholar]
- Varmaghani M, Farzadfar F, Sharifi F, Rashidian A, Moin M, Moradi-Lakeh M. Prevalence of asthma, COPD, and chronic bronchitis in Iran: a systematic review and meta-analysis. Iran J Allergy Asthma Immunol 2016; 15(2):93-104. [ Google Scholar]
- Raji H, Riahi A, Borsi SH, Masoumi K, Khanjani N, AhmadiAngali K. Acute effects of air pollution on hospital admissions for asthma, COPD, and bronchiectasis in Ahvaz, Iran. Int J Chron Obstruct Pulmon Dis 2020; 15:501-14. doi: 10.2147/copd.s231317 [Crossref] [ Google Scholar]
- Raddadi Y, Adib-Hajbaghery M. Health literacy and quality of life in Iranian persons with COPD. Heart Lung 2022; 54:61-7. doi: 10.1016/j.hrtlng.2022.02.009 [Crossref] [ Google Scholar]
- GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 2024; 403(10440):2133-61. doi: 10.1016/s0140-6736(24)00757-8 [Crossref] [ Google Scholar]
- Sharifi H, Ghanei M, Jamaati H, Masjedi MR, Aarabi M, Sharifpour A. Burden of obstructive lung disease study in Iran: first report of the prevalence and risk factors of COPD in five provinces. Lung India 2019; 36(1):14-9. doi: 10.4103/lungindia.lungindia_129_18 [Crossref] [ Google Scholar]
- Sharifi H, Masjedi MR, Emami H, Ghanei M, Eslaminejad A, Radmand G. Burden of obstructive lung disease study in Tehran: prevalence and risk factors of chronic obstructive pulmonary disease. Lung India 2015; 32(6):572-7. doi: 10.4103/0970-2113.168129 [Crossref] [ Google Scholar]
- Kiani FZ, Ahmadi A, Soleymani Babadi A, Rouhi H. Profile and preliminary results of Iranian sub cohort chronic obstructive pulmonary disease (COPD) in Shahrekord PERSIAN cohort in southwest Iran. BMC Pulm Med 2021; 21(1):105. doi: 10.1186/s12890-021-01469-8 [Crossref] [ Google Scholar]
- Sharifi H, Ghanei M, Jamaati H, Masjedi MR, Najafimehr H, Fakharian A. Effect of COPD on health-related quality of life; results from the BOLD study in Iran. Tanaffos 2021; 20(1):51-8. [ Google Scholar]
- Burney PG, Patel J, Newson R, Minelli C, Naghavi M. Global and regional trends in COPD mortality, 1990-2010. Eur Respir J 2015; 45(5):1239-47. doi: 10.1183/09031936.00142414 [Crossref] [ Google Scholar]
- GBD 2019 Universal Health Coverage Collaborators. Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020; 396(10258):1250-84. doi: 10.1016/s0140-6736(20)30750-9 [Crossref] [ Google Scholar]
- Raeisy L, Masoompour SM, Rezaianzadeh A. Evaluation of the prevalence of asthma and chronic obstructive pulmonary disease among opium users, and cigarette smokers and comparison with normal population in Kharameh: a cross-sectional study. BMC Pulm Med 2023; 23(1):419. doi: 10.1186/s12890-023-02734-8 [Crossref] [ Google Scholar]
- Noorbala AA, Saljoughian A, Bagheri Yazdi SA, Faghihzadeh E, Farahzadi MH, Kamali K. Evaluation of drug and alcohol abuse in people aged 15 years and older in Iran. Iran J Public Health 2020; 49(10):1940-6. doi: 10.18502/ijph.v49i10.4697 [Crossref] [ Google Scholar]
- Taghizadeh F, Mokhtarani B, Rahmanian N. Air pollution in Iran: the current status and potential solutions. Environ Monit Assess 2023; 195(6):737. doi: 10.1007/s10661-023-11296-5 [Crossref] [ Google Scholar]
- Pilehvar AP. Spatial-geographical analysis of urbanization in Iran. Humanit Soc Sci Commun 2021; 8(1):63. doi: 10.1057/s41599-021-00741-w [Crossref] [ Google Scholar]
- Pérez-Padilla R, Regalado J, Vedal S, Paré P, Chapela R, Sansores R. Exposure to biomass smoke and chronic airway disease in Mexican women A case-control study. Am J Respir Crit Care Med 1996; 154(3 Pt 1):701-6. doi: 10.1164/ajrccm.154.3.8810608 [Crossref] [ Google Scholar]
- Zhang J, Smith KR. Hydrocarbon emissions and health risks from cookstoves in developing countries. J Expo Anal Environ Epidemiol 1996; 6(2):147-61. [ Google Scholar]
- Chen BH, Hong CJ, Pandey MR, Smith KR. Indoor air pollution in developing countries. World Health Stat Q 1990; 43(3):127-38. [ Google Scholar]
- Smith KR. National burden of disease in India from indoor air pollution. Proc Natl Acad Sci U S A 2000; 97(24):13286-93. doi: 10.1073/pnas.97.24.13286 [Crossref] [ Google Scholar]
- Tibrewal K, Venkataraman C. COVID-19 lockdown closures of emissions sources in India: lessons for air quality and climate policy. J Environ Manage 2022; 302(Pt B):114079. doi: 10.1016/j.jenvman.2021.114079 [Crossref] [ Google Scholar]
- Lin B, Zhu J. Changes in urban air quality during urbanization in China. J Clean Prod 2018; 188:312-21. doi: 10.1016/j.jclepro.2018.03.293 [Crossref] [ Google Scholar]
- Feenstra TL, van Genugten ML, Hoogenveen RT, Wouters EF, Rutten-van Mölken MP. The impact of aging and smoking on the future burden of chronic obstructive pulmonary disease: a model analysis in the Netherlands. Am J Respir Crit Care Med 2001; 164(4):590-6. doi: 10.1164/ajrccm.164.4.2003167 [Crossref] [ Google Scholar]
- Boers E, Barrett M, Su JG, Benjafield AV, Sinha S, Kaye L. Global burden of chronic obstructive pulmonary disease through 2050. JAMA Netw Open 2023; 6(12):e2346598. doi: 10.1001/jamanetworkopen.2023.46598 [Crossref] [ Google Scholar]
- GBD 2017 Mortality Collaborators. Global, regional, and national age-sex-specific mortality and life expectancy, 1950-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018; 392(10159):1684-735. doi: 10.1016/s0140-6736(18)31891-9 [Crossref] [ Google Scholar]
- Salvi S. Tobacco smoking and environmental risk factors for chronic obstructive pulmonary disease. Clin Chest Med 2014; 35(1):17-27. doi: 10.1016/j.ccm.2013.09.011 [Crossref] [ Google Scholar]
- Perez TA, Castillo EG, Ancochea J, Pastor Sanz MT, Almagro P, Martínez-Camblor P. Sex differences between women and men with COPD: a new analysis of the 3CIA study. Respir Med 2020; 171:106105. doi: 10.1016/j.rmed.2020.106105 [Crossref] [ Google Scholar]
- Varkey AB. Chronic obstructive pulmonary disease in women: exploring gender differences. Curr Opin Pulm Med 2004; 10(2):98-103. doi: 10.1097/00063198-200403000-00003 [Crossref] [ Google Scholar]
- Celli BR, Halbert RJ, Nordyke RJ, Schau B. Airway obstruction in never smokers: results from the Third National Health and Nutrition Examination Survey. Am J Med 2005; 118(12):1364-72. doi: 10.1016/j.amjmed.2005.06.041 [Crossref] [ Google Scholar]