Int J Aging. 2023;1:e6.
doi: 10.34172/ija.2023.e6
Review Article
Mobile Health-Based Interventions in Self-care and Treatment Adherence in Older People: A Review Study
Mohammad Hossein Kaveh 1  , Sara Kaveh 2
, Sara Kaveh 2  , Maryam Rabiey Faradonbeh 3, *
, Maryam Rabiey Faradonbeh 3, * 
Author information:
1Research Center for Health Sciences, Institute of Health, Department of Health Promotion, School of Health, Shiraz University of Medical Sciences, Shiraz, Iran
2Department of Health Management, Policy & Economics, School of Public Health, Tehran University of Medical Sciences (TUMS), Tehran, Iran
3Department of Health Promotion, School of Health, Shiraz University of Medical Sciences, Shiraz, Iran
Abstract
Objectives:
To investigate mobile health (m-health) interventions in self-care and treatment adherence in older adults.
Design:
A review study.
Participants:
People over 50 years of age with chronic diseases.
Interventions:
M-health-based interventions were used to promote self-care and treatment adherence.
Outcome measures:
Self-care and adherence.
Results:
The duration of interventions in different studies was between 8 weeks to 12 months. All participants were over 50 years old and included both male and female groups. The findings showed that m-health has a good potential for educating and empowering the target population. M-health interventions can be categorized into 5 groups such as messages, calls, applications, devices, and Internet-based interventions. They can also be used to provide care and promote health in various diseases such as diabetes, heart disease, cancer, and lung disease. In this study, self-care included practices such as self-care behaviors, self-efficacy, and self-monitoring/management. Similarly, adherence included practices such as treatment/ medication adherence, and healthy behaviors adherence.
Conclusions:
The results indicated the positive effects of m-health on improving self-care and treatment adherence. Considering the increasing population of elderly people in the world, and the increase of various problems and challenges affecting their health, using novel technologies to provide health and care services while reducing the adverse effect caused by the lack of resources can bring positive social and economic effects. It seems that the planned use of this technology can help increase the healthcare system’s efficiency and reduce health costs.
Keywords: Aged, Self-care, Medication adherence, M-health, Interventions
Introduction
The elderly include a large and growing population in the world whose cost of medical treatments and the usage of healthcare services are high because most of them suffer from chronic conditions such as hypertension, diabetes, cardiovascular diseases, respiratory problems, and cancer.1,2 Comorbidity and its subsequent medical treatments reduce people’s quality of life and self-efficacy, thus leading to psychological problems such as depression.3,4 Hence, the maintenance of the quality of life for the elderly and the increasing cost of financial and human resources required to take care of them have become major issues.5
In this regard, one of the useful approaches is to employ mobile health (m-health) capabilities. M-health is a medical and public health activity supported by mobile devices, laptops, tablets, and computers.2,6 It is defined as “a hand-held (or sometimes wearable) transmitter with multifunctional capabilities used to store, transmit, and receive health information”.6 Advances in m-health services in medicine and healthcare can increase self-management and treatment adherence in the elderly, leading to a wider and more appropriate relationship between patients, their caregivers, and service providers, as well as a reduction in complications and mortality.1,5,7
Elderly people are more at risk of medication non-adherence than youth mainly due to a condition referred to as comorbidity (i.e., a condition in which the elderly suffers from several diseases at the same time and, subsequently, uses different drugs).8 This may lead to disease aggravation, a need for a doctor visit or hospitalization, due to complications resulting from not taking or taking too much medicine.8,9 Taking advantage of the capabilities of m-health, including sending reminders to take drugs, improving patient-caregiver relationships, and constantly receiving vital information about the patients through various sensors can reduce complications and mortality. Moreover, m-health can improve self-care. Promoting self-care and treatment adherence increases the quality of life while reducing complications and costs.10
Today, smartphones are increasingly used by different groups of people, even the elderly. Therefore, taking advantage of mobile phone capabilities and their applications could be a promising and sustainable strategy to improve medication adherence and health outcomes for patients with chronic diseases. Monitoring symptoms, receiving patient information about side effects of treatments, sending reminders to the patient to take medication, providing education as well as self-care and self-management devices for the patient, communicating with the health providers, and providing social support are the capabilities of m-health intervention.11-13 So far, the effectiveness of these interventions has been shown in various diseases such as diabetes, hypertension, cardiovascular disease, and cancer.14-17 The results of the study by Soriano Marcolino et al demonstrated that numerous m-health-based interventions had positive effects in cases such as managing chronic diseases, improving disease symptoms, and reducing mortality and hospitalization rates.18 In critical situations such as the COVID-19 pandemic, providing care during m-health interventions can be an effective and efficient method when the elderly have limited access to healthcare services. Given the above-mentioned explanations, this study examined various m-health interventions in the elderly and their impact on promoting self-care and adherence. Considering that the focus of this study is on the consequences of self-care and adherence in the elderly, the findings of this study can be effective for related programs, researchers, and designers.
Methods
The present review study aimed to investigate whether m-health technology interventions can be effective in improving self-care and treatment adherence in the elderly. For this purpose, advanced search in reputable scientific resources such as PubMed, Science Direct, Scopus, Web of Science, Magiran, SID, and Iran Medex was performed from January 1, 2015 to December 31, 2022. To perform the search process, several keywords and their MeSH terms were searched and their Persian equivalents were used, including “patient compliance”, “adherence”, “elder”, “older adult”, “aged”, “frail elderly”, “telemedicine”, “mobile health”, “medication”, and self-care”.
Self-care includes activities that the elderly can use to manage and monitor their diseases with a positive attitude to their health status, as well as perform healthy behaviors, including practices such as self-care behaviors, self-efficacy, and self-monitoring/management, to improve their self-care ability.19,20 Treatment adherence also includes activities that the elderly do to implement medical orders to cure their diseases that include treatment/medication adherence and healthy behavior adherence.21 M-health is an innovative and enabling technology area for healthcare and encompasses services provided by mobile phones such as messages, calls, applications, web, and devices that can be connected to cell phones.22,23 It is related to other information and communication technologies for the healthcare domains of telemedicine, telehealth, and e-health.5,16
In this study, the following five groups of articles met the eligibility criteria, including intervention studies with m-health applications, articles that had been conducted with patients who were over 50 years old and had chronic diseases, and articles in which the study design included randomized clinical trials (RCTs). The other two groups were articles with outcomes such as improving self-care or adherence and articles written in English or Persian. Articles other than RCTs that did not include m-health interventions or had not been conducted in patients younger than 50 years old were excluded from the review.
Some data were extracted in an excel spreadsheet, including bibliographic information (first author, publication year, and country), demographic information of patients, intervention, outcomes, and results.
Articles were selected and data were extracted by two researchers independently, and any discrepancies were resolved through discussion with the third reviewer.
Results
Initially, 562 articles were found for review, and 123 articles remained after removing duplicates and checking the titles and abstracts of articles. Then, the researchers read the full text of the remaining articles and, eventually, 22 articles met our inclusion criteria (Figure 1).
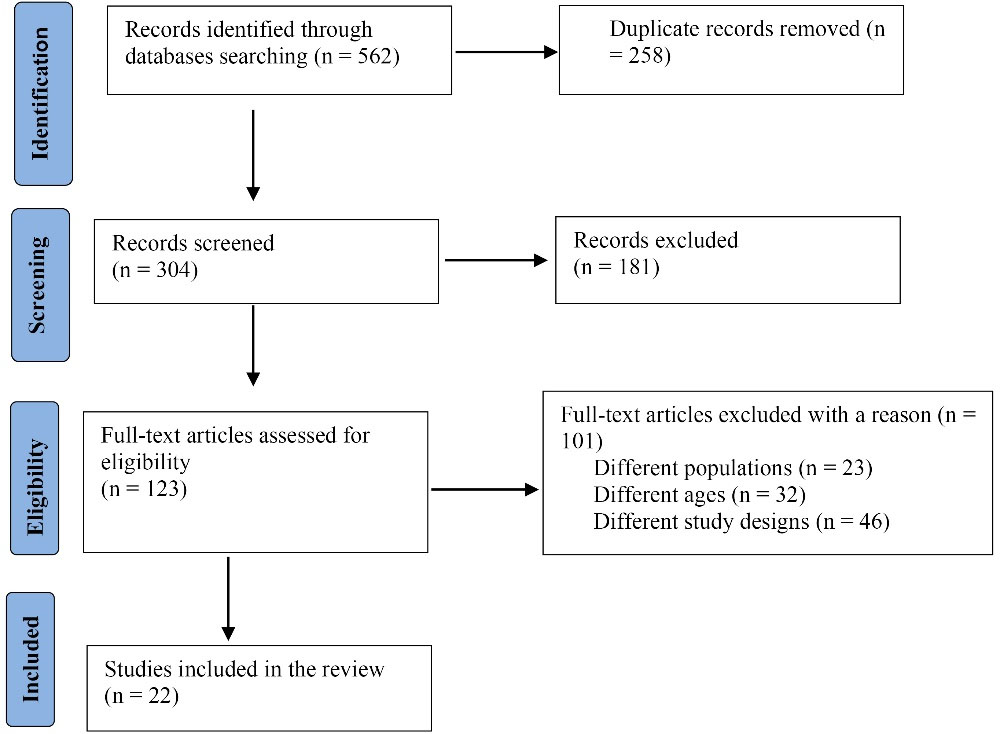
Figure 1.
Study flow diagram
.
Study flow diagram
Overall, 22 RCTs evaluating the impact of various M-health interventions on self-care and adherence in the last 8 years were reviewed in this study. All studies were in English, and the duration of interventions in different studies was between 8 weeks to 12 months. The number of participants in both control and intervention groups varied from 5 to 440 people. A total of 4,331 people (2262 and 2069 in the intervention and control groups, respectively) participated in the study. Of these, 2291 (1195 and 1096 in the intervention and control groups, respectively) and 2040 (1067 and 973 in the intervention and control groups, respectively) were males and females, respectively. All participants were over 50 years old. Of these 22 studies, four, even, and two studies were about heart diseases,14,24-26 type 2 diabetes (T2D),16,27-32 and hypertension,15,33 respectively, and one study was about pre-diabetes.34 In addition, one study was about breast cancer.17 Moreover, two, one, and four studies were about cancer screening (breast35 and colorectal36), chronic obstructive pulmonary disease (COPD),37 and a combination of two diseases, respectively (Table 1).38-41
Table 1.
Baseline Characteristics of Included Studies
|
Author(s) (Reference)
|
Country
|
RCT Code
|
Disease
|
Duration
|
Sample Size (N)
|
Age (y)
|
Gender Distribution (N) (Male)
|
|
Intervention
|
Control
|
Intervention
Mean (SD)
|
Control
Mean (SD)
|
Intervention
|
Control
|
| Abaza and Marschollek38 |
Egypt |
NCT02868320 |
Type 1 and 2 diabetes |
12 weeks |
34 |
39 |
51.24 (8.66) |
51.77 (9.68) |
16 |
16 |
| Anderson et al35 |
UK (Scotland) |
ISRCTN11057518 |
Breast cancer screening |
12 months |
276 |
276 |
- |
- |
0 |
0 |
| Bae et al25 |
Korea |
KCT0005087 |
CHD |
6 months |
440 |
439 |
60.1 (10.6) |
60.7 (10.4) |
368 |
364 |
| Becker et al27 |
Brazil |
NCT 01972412 |
Type 2 diabetes |
4 months |
36 |
27 |
63 (7.85) |
63 (11.38) |
16 |
10 |
| Van den Berg et al17 |
Netherlands |
NTR2935 |
Breast cancer |
4 months |
70 |
80 |
51.44 (8.30) |
50.18 (9.15) |
0 |
0 |
| Coultas et al37 |
USA |
NCT01108991 |
COPD |
20 weeks |
149 |
156 |
70.8 (9.5) |
69.8 (9.5) |
74 |
77 |
| Crowley et al28 |
USA-Carolina |
NCT01778751 |
Type 2 diabetes |
6 months |
25 |
25 |
60 (8.4) |
60 (9.2) |
25 |
23 |
| Pfaefli Dale et al14 |
New Zealand |
A C T R N 1 2 6 1 3 0 0 0 9 0 1 7 0 7 |
CHD |
24 weeks |
61 |
62 |
59.0 (10.5) |
59.9 (11.8) |
48 |
52 |
| Ding et al26 |
Australia |
ACTRN12614000916640 |
CHF |
6 months |
91 |
93 |
69.5 (12.3) |
70.8 (12.4) |
66 |
75 |
| Dugas et al29 |
USA |
NCT02127216 |
Type 2 diabetes |
13 weeks |
T1 (App only): 5
T2 (App with clinician Engagement): 5
T3 (App with peer engagement features): 6
T4 (App with both clinician engagement and peer engagement): 6 |
5 |
T1: 65.40 (4.72)
T2: 72.00 (9.30)
T3: 66.00 (5.18)
T4: 68.17 (3.66) |
66.40 (4.93) |
T1: 5
T2: 5
3: 6
T4: 6 |
5 |
| Fors et al39 |
France |
SRCTN55562827 |
COPDand/or CHF |
6 months |
103 |
118 |
78.3 (9.5) |
76.9 (8.3) |
52 |
49 |
| Frias et al40 |
USA |
NCT02827630 |
Hypertension and type 2 diabetes |
12 weeks |
4 weeks: 40
12 weeks: 40 |
29 |
4 weeks: 58.8 (1.4)
12 weeks: 56.7 (1.8) |
61.6 (1.7) |
4 weeks: 19
12 weeks: 11 |
19 |
| Griauzde et al34 |
USA |
NCT03025607 |
Prediabetes |
12 weeks |
App-only:24
app and Fitbit devices:22 |
23 |
App-only: 52.1 (12.0)
app and Fitbit devices: 51.6 (11.1) |
51.3 (11.0) |
App-only: 9
app and Fitbit devices: 8 |
8 |
| Kim et al33 |
Korea |
NCT01975428 |
Hypertension |
6 months |
52 |
43 |
57.5 (8.6) |
57.7 (8.7) |
14 |
16 |
| Kim15 |
Korea |
─ |
Hypertension |
8 weeks |
LMS: 32
Phone-based HC: 30
LMS + HC: 31 |
31 |
LMS: 77.21 (6.69)
HC: 77.50 (6.38)
LMS and HC: 78.25 (6.61) |
77.70 (6.92) |
LMS: 12
HC: 19
LMS and HC: 17 |
20 |
| Miller et al36 |
USA |
NCT02088333 |
Colorectal cancer screening |
24 weeks |
223 |
227 |
58 (median) |
57 (median) |
99 |
109 |
| Peimani et al30 |
Iran |
─ |
Type 2 diabetes |
12 weeks |
Tailored SMS group: 50
non-tailored SMS group: 50 |
50 |
Tailored SMS group: 49.78 (9.76)
Non-tailored SMS group: 53.26 (10.49) |
54.56 (9.88) |
Tailored SMS group: 27
Non-tailored SMS group: 28 |
26 |
| Piette et al24 |
USA |
NCT00555360 |
HF |
12 months |
166 |
165 |
67.6 (10.3) |
68.1 (10.1) |
166 |
163 |
| Piette et al41 |
USA |
HUM00081734 |
Diabetes and hypertension |
4 months |
45 |
27 |
62.2 |
63 |
32 |
15 |
| Sarayani et al31 |
Iran |
IRCT201212108612N1 |
Type 2 diabetes |
3 months |
50 |
50 |
53.4 (10.3) |
56.7 (11.5) |
28 |
31 |
| Sun et al16 |
China |
1800015214 |
Type 2 diabetes |
6 months |
44 |
47 |
68.04 (median) |
67.9 (median) |
19 |
18 |
| Tan et al32 |
Singapore |
─ |
Type 2 diabetes |
8 weeks |
56 |
57 |
61.50 (6.78) |
62.75 (7.20) |
0 |
0 |
Abbreviations: CHD, coronary heart disease; COPD, chronic obstructive pulmonary disease; CHF, chronic heart failure; HF, heart failure; SMS, short message services; RCT, randomized clinical trial; SD, standard deviation; HC, Health Coaching
Types of m-health interventions and the number of studies in any type are presented in Table 2. M-health interventions can be divided into 5 general groups, including messages, calls, applications, devices, and internet-based interventions. In message-based interventions, educational or reminder messages are sent in the form of short message services (SMS), long message services (LMS), or emails to patients or their caregivers. In telephone call interventions, training, follow-ups, and communication with service providers such as nurses are provided by a telephone call. Some educational interventions are provided through designed online or offline applications. Devices that are used include a glucometer for self-assessment of blood sugar or a pedometer for self-assessment of physical activity, and an electronic weight scale for weight monitoring, as well as a device for monitoring the heart rate and controlling blood pressure with the ability to connect to a mobile phone. Web-based interventions are training through wireless tools and websites. Research studies have used a combination of several interventions. Educational information about T2D was presented to participants in the control group in the study by Griauzde.34 Similarly, a standard program of disease management was provided in the study of Kim.33 Furthermore, telephone calls were presented in studies by Piette24 and Piette.41 Eventually, routine care was provided in the other studies (Table 2).
Table 2.
Description of Interventions in Included Studies
|
Author(s) (Reference)
|
Intervention
|
Results
|
P
Valuea
|
| Abaza et al38 |
Educational and reminder SMS |
Self-efficacy |
< 0.0001 |
| Treatment and medication adherence |
< 0.0001 |
| Anderson et al35 |
Telephone calls
Device: Pedometer for self-assessment of physical activity |
Self-monitoring |
NA |
| Bae et al5 |
Supporting website and SMS
Device: Electronic devices for monitoring blood
pressure and heart rate |
Medication adherence |
< 0.001 |
| Becker et al27 |
Group 1: Educational telephone Group 2: Contacts educational mailed |
Self-care behaviors |
NA |
| Van den Berg et al17 |
Web-based self-management |
Self-efficacy |
< 0.05 |
| Coultas et al37 |
Telephone-delivered, home-based health coaching
Device: Pedometer for self-monitoring of physical activity |
Self-monitoring |
NA |
| Crowley et al28 |
Telemedicine intervention by a nurse for self-monitoring of blood glucose and telephone calls |
Medication adherence |
< 0.050 |
| Self-care |
< 0.047 |
Pfaeffli
Dale et al14 |
SMS and a supporting website |
Self-efficacy |
0.73 |
| Medication adherence |
0.004 |
| Ding et al26 |
Telephone calls
Devices: Electronic weight scale
and a computer tablet for weight monitoring |
Self-care |
0.26 |
| Medication adherence |
0.05 |
| Dugas et al29 |
Gamified M-Health App (DiaSocial) |
Medication adherence |
< 0.001 |
| Fors et al39 |
Telephone calls by a registered nurse |
Self-efficacy |
< 0.001 |
| Frias et al40 |
DMO (including digital medicines, the wearable sensor patch, and the mobile device app) |
Medication adherence |
NA |
| Griauzde et al34 |
Group 1: M-health App (App-only)
Group 2: App plus a physical activity tracker and wireless enabled digital scale for self-monitoring (app-plus) |
Healthy behavior adherence |
NA |
| Kim et al33 |
Wireless self-monitoring, reminders for self-monitoring
Web-based disease management
program
Device: Blood pressure monitoring device |
Medication adherence |
0.79 |
| Kim et al15 |
LMS
Telephone call |
Medication adherence
Self-efficacy
Self-management |
< 0.001 |
| Miller et al36 |
iPad App and sending emails for supporting patients |
Self-monitoring |
NA |
| Peimani et al30 |
Group 1: Tailored SMS
Group 2: Non-tailored SMS |
Self-care
Self-efficacy |
< 0.001 |
| Piette et al24 |
IVR calls with automated emails sent to the patient’s caregiver |
Self-care
Treatment adherence |
< 0.01 |
| Piette et al41 |
IVR calls with automated emails sent to the patient’s caregiver |
Self-care |
< 0.03 |
| Sarayani et al31 |
Telephone calls
Device: Blood glucose self-monitoring device |
Self-care |
< 0.05 |
| Medication adherence |
< 0.01 |
| Sun et al16 |
M-health management app
Telephoning for medical advice and reminding the patients
Device: Glucometer for self-assessment of blood sugar |
Self-management |
NA |
| Tan et al32 |
Telephone calls |
Self-efficacy
Self-care |
< 0.001 |
Abbreviations: SMS, short message services; NA, not applicable; LMS, long message service; IVR, interactive voice response.
a Statistically significant (P < 0.05).
In this study, self-care and adherence were the two main outcomes. Different studies in different forms (Table 3) evaluated these two factors and the impact of m-health on them. All studies demonstrated that m-health interventions are effective in self-care and have been able to improve self-care behaviors (including healthy lifestyles such as appropriate diet and adequate physical activity), self-management, and self-efficacy. These interventions have also promoted treatment, medication adherence, or healthy behavior adherence such as proper nutrition and adequate physical activity (Table 3).
Table 3.
Description of Outcomes in Included Studies
|
Study
|
Self-care Behaviors
|
Self-efficacy
|
Self-monitoring/ Management
|
Treatment/ Medication Adherence
|
Healthy Behavior Adherence
|
Key Findings
|
| Abaza et al38 |
|
● |
|
● |
|
Intervention patients at the endpoint showed considerable improvements in treatment and medication adherence and self-efficacy. |
| Anderson et al35 |
|
|
● |
|
|
The intervention could improve healthy behaviors (eating habits, alcohol intake, and physical activity) and self-monitoring. |
| Bae et al25 |
|
|
● |
● |
● |
The intervention could improve healthy behavior adherence (diet, smoking, and psychosocial variables), medication adherence, and self-management of lifestyle. |
| Becker et al27 |
● |
|
|
|
|
The intervention could improve self-care skills. |
| van den Berg et al17 |
|
● |
|
|
● |
The intervention promoted healthy behavior adherence, self-management, and self-efficacy; however, there was no significant difference between the two groups. |
| Coultas et al37 |
|
|
● |
|
● |
The intervention group improved self-management and physical activity compared to the control group. |
| Crowley et al28 |
● |
|
|
● |
|
Intervention participants’ diabetes self-care and healthy behavior adherence were improved versus the usual care group. |
| Pfaeffli Dale et al14 |
|
● |
|
● |
● |
The intervention group reported significantly greater medication and healthy behavior adherence and self-efficacy score. |
| Ding et al26 |
● |
|
● |
● |
|
Using the ITEC-CHF intervention (App, nurse-led care, and telephone support) improved self-management, self-care, medication adherence, and self-care behavior (exercise, diet, and smoking). |
| Dugas et al29 |
|
|
● |
● |
|
Using the application improved self-management, treatment, and healthy behavior (exercise and diet) adherence. |
| Fors et al39 |
● |
● |
|
|
|
Person-centered support via telephone mitigates worsening self-efficacy without increasing the risk of clinical events in chronically ill patients with CHF and/or COPD. |
| Frias et al40 |
● |
|
|
● |
● |
The use of DMO promoted medication adherence and self-care. |
| Griauzde et al34 |
● |
|
|
|
● |
Among individuals with prediabetes, this m-health intervention could improve self-care and healthy behavior adherence. |
| Kim et al33 |
● |
|
● |
● |
|
The self-monitoring intervention improved medication adherence and self-care skill. |
| Kim15 |
● |
● |
|
● |
|
There were improvements in medication adherence, hypertension-related knowledge, self-efficacy, and self-management behavior in the intervention group as compared to the control group. |
| Miller et al36 |
|
|
● |
|
|
The intervention affected self-surveys and self-ordered. |
| Peimani et al30 |
● |
● |
|
|
● |
Sending short text messages as a method of education can improve self-care behaviors, self-efficacy, and healthy behavior adherence. |
| Piette et al24 |
● |
|
● |
● |
|
Patients’ medication adherence and self-care monitoring improved by intervention |
| Piette et al41 |
● |
|
|
● |
|
M-health + CP (CarePartner) is a scalable strategy that could increase self-management and medication adherence. |
| Sarayani et al31 |
● |
|
|
● |
|
Medication adherence and self-care significantly improved in the telephone-based intervention group |
| Sun et al16 |
|
|
● |
|
● |
Satisfactory results of self-monitoring, self-management skills, and healthy behaviors (diet and exercise) adherence were demonstrated. |
| Tan et al32 |
● |
● |
|
● |
|
Compared with participants in the control group, those who received Diabetes Self-Efficacy
Enhancing Program had a significantly higher increase in self-efficacy, diabetes self-care activities, and healthy medication adherence. |
Abbreviations:DMO, Digital medicine offering; ITEC-CHF, Innovative telemonitoring enhanced care program for chronic heart failure; CHF, Chronic heart failure; COPD, Chronic obstructive pulmonary disease.
In the studies included in this review, different interventions had been used to promote adherence and self-care in different diseases.
Diabetes
Diabetes is a metabolic disease that causes irreversible complications such as blindness, renal failure, heart attack, and lower limb amputation, especially in the elderly.42 The use of m-health technology for self-care in this disease leads to blood sugar control, helping in regulating medications and lifestyle modification, as well as the effectiveness of communication between the health provider and the patient.43,44 Research studies included in this study, with a focus on diabetes, had employed some interventions such as sending a text message to the patient, providing advice by a person such as a nurse or a pharmacist through making phone calls, sending reminder texts, using glucometers to upgrade blood sugar self-assessment, using smartphone Apps (DiaSocial and Fitbit), sending emails to caregivers, and holding workshops and telephone follow-ups in order to improve self-care and adherence.
In a study conducted by Sun et al, training related to medication, diet, and physical activity was provided for three months through an m-health App that improved blood sugar levels, self-assessment, and healthy behavior adherence. In this study, there were 44 elderlies over 65 years old in the intervention group who were given a glucometer to assess their blood sugar and a pedometer to assess their physical activity. These devices were connected to people’s smartphones via Bluetooth. The medical team transmitted educational and reminder recommendations to people by either sending messages through the application or making phone calls. However, as the information about the diet was not as exact as that of the blood sugar level, and the impact of guidance related to diet and exercise on controlling the blood sugar level was not reliable. This study suggests that an exact approach be used in order to collect data about the amount of received and used calories.16
In a study by Peimani et al, 150 adults were randomized into three groups of 50 participants. Then, text messages were sent to two of the groups (tailored and non-tailored SMS), while the control group received no text messages. Phone calls were also made to individuals in both intervention groups once a week. Based on the aim of the study, the content of the educational message was about blood sugar control, diet, and physical activity, which ultimately led to optimal control of blood sugar levels and the promotion of diabetes self-care and self-efficacy. Considering that the education level of patients had an impact on the effectiveness of educational text messages, it is recommended that this intervention be performed in larger groups and similar education levels.30
Pre-diabetes
People with fasting blood sugar between 100 and 125 are at risk for diabetes; one of the effective ways to deal with diabetes is the prevention of infection, especially in high-risk populations.45 Improving healthy lifestyle adherence behaviors, including weight loss, adequate physical activity, a balanced diet, and blood sugar control by m-health technology, reduces the risk of developing diabetes in high-risk individuals. In this study, self-assessment Apps and devices were used to provide education and self-assessment of blood sugar for pre-diabetic people. The results revealed that the interventions could improve self-care and healthy lifestyle adherence behaviors in this group of people.34
Hypertension
Hypertension, which is the poor control of blood pressure, is an important cause of mortality and disease burden worldwide.15 The use of m-health technology in promoting self-management has led to proper control of blood pressure, reducing the risk of stroke, heart attack, heart failure, and cardiovascular diseases.15,33 In the studies included in this review, the use of applications, self-assessment of blood pressure by some devices (Fitbit), and trainings through both websites and text messages were among the approaches employed in m-health.
In 2019, Kim conducted an 8-week study on people over the age of 65 with high blood pressure. In this study, 124 participants were divided into 4 groups. In the control groups, 31 people were provided with routine care. In addition, 30, 32, and 31 people received telephone health coaching, educational long text messages, and telephone health coaching with educational long text messages, respectively. The educational content was about diet and weight control, physical activity, and blood pressure control. The group which simultaneously received long messages and phone calls indicated favorable results in self-efficacy and hypertension-related knowledge, self-management, and medication adherence, as well as reduced blood pressure levels in comparison with other groups. In this group in which participants received long messages, self-efficacy and hypertension-related knowledge, self-management, and medication adherence were improved compared to the control group, and there was a further decrease in blood pressure levels. However, it must be noted that the short duration of the intervention and the small sample size make it difficult to generalize the finding of this study to the total population.15
Heart Disease
Heart disease is one of the most common causes of death in the world, which has a complication such as arrhythmia.14 Continuous heart rate monitoring can be effective in reducing deaths from heart disease. The M-health system is a potential solution to help heart patients improve self-care skills regardless of time and place.46 As mentioned earlier, research studies investigating people with heart diseases were examined in this review. In addition, m-health interventions had been performed by telephone calls, texting, training through a support website, and feedback emails to patients’ caregivers in order to improve self-management and adherence.
Piette et al examined the effect of voice call intervention along with sending feedback emails to patients’ caregivers over 12 months. This intervention could improve communication between patients and their caregivers and lead to improved medication adherence and better self-management of the disease. This study was performed on the population of the Veterans Health Department, thus all members were males; therefore, it seems useful to perform this intervention on a population with a more balanced gender distribution of both males and females so that the results will be more favorably generalizable.24
Chronic Obstructive Pulmonary Disease
COPD is a chronic lung problem that leads to increased referral to emergency departments and hospitalization at high cost and is associated with an increased risk of mortality.47 M-health technology can improve adaptation to disease and self-control and create new and integrated interactions between physicians and patients.48,49 Providing training through telephone calls and the use of pedometers for self-assessment of physical activity were the strategies used to improve self-care and adherence in patients with COPD in this study.37
Cancer and Cancer Screening
Using m-health technology to promote self-care behaviors, including weight and diet control, optimal physical activity, and clinical signs such as blood sugar and lipids, promotes self-management and is effective in preventing cancer. In two cancer screening studies in this review, providing telephone training, using a pedometer for self-assessment of physical activity, using the mPATH-CRC application, and sending e-mail were among the interventions applied to promote self-management.35,36 Weight management program for postmenopausal women was one of the preventive measures for breast cancer. Providing training on lifestyle modification with a focus on diet and physical activity habits using health technology is an effective and affordable way to control weight and improve behavioral habits in people.35 Educating people about colorectal cancer and its prevention and decision-making assistance during a mobile App led patients to express the importance and priority of screening, discuss screening with their provider, and request a screening test.36 In a study of women with breast cancer, web-based education could improve self-efficacy and healthy lifestyle behavior adherence. In this study, using web-based self-management intervention to reduce distress and empower, women’s positive adjustment increased, and factors such as self-efficacy, quality of life, and fulfillment represented an improvement. A general self-efficacy scale was used to measure self-efficacy in the form of self-report.17
Discussion
The increase in the elderly population in the world, their incidence of various diseases, and consequently, the simultaneous use of multiple drugs have affected healthcare systems.16 Factors such as the distribution of the elderly population, health system capacity constraints and access problems, increased cost and burden of healthcare, growing tendencies of people to use mobile phones, and the use of care services based on information and communication technologies, especially mobile phones, have made mobile phones important and innovative alternatives.50,51 Improving the ability of this population in self-care and treatment adherence is an important issue that can not only improve self-efficacy, quality of life, and psychological well-being but also reduce patients’ sense of isolation and hospitalization.11,19 Recent reports indicate an increase in the use of this technology in the provision of care services and more in the form of health education and counseling. However, insufficient information is available on the extent to which these types of services have been successful and effective due to demographic and socio-economic differences, types of available services, and the type of diseases.52
As mentioned before, the current study ought to investigate the effect of m-health interventions on self-care and adherence in people over 50 years of age. In the 22 studies included in this review article, there were a total of 4331 people over the age of 50 with diseases such as heart disease, T1D and T2D, hypertension, and COPD, as well as people at risk for diabetes, breast cancer, and colorectal cancers. Interventions included various types of mobile phone-based interventions that were used alone or in combination. These interventions were in the form of messages, calls, web-based interventions, and applications such as Fitbit and DiaSocial. Further, in some cases, devices such as a pedometer, a glucometer, and a device (Withings Blood Pressure Monitor) with the ability to connect to participants’ mobile phones were employed to control blood pressure.
Advances in m-health services in medicine and healthcare can be effective in improving the self-management of the elderly, controlling diseases more efficiently, and establishing wider and more appropriate communication between patients and service providers.5,7 However, due to the lack of review and systematic review studies based on the types of diseases (or different diseases) and demographic differences, there is not enough available evidence about the effectiveness of these interventions.
The various applications used in diabetes have improved self-care capabilities while reducing the burden of diabetes.53 They could also help improve patients’ self-efficacy by improving blood sugar self-assessment.54 The self-assessment of blood pressure in hypertensive people has been effective in controlling the disease and self-management.12,55 In addition, the message-based intervention has led to improved self-care behaviors in heart patients.56 Self-management training provided by this technology has been efficient in managing patients’ conditions with various diseases.2,3 Hartz et al evaluated the impact of m-health technology on the prevention and management of diabetes. Their findings, consistent with the results of the present study, revealed that this technology is effective in promoting self-management and self-efficacy. However, unlike the present study which considers various chronic diseases, Hartz et al only examined diabetes without evaluating the impact of this technology on adherence.57 The role of m-health applications in facilitating self-care was evaluated and self-care, as in the present study, was evaluated in a review study. In this study, the applications were divided into several groups, including diabetes management, cardiac arrhythmia management, elderly monitoring, drug monitoring, smoking cessation, obesity control and management, asthma control and management, and stroke control and management. The results of the study demonstrated that mobile applications have the necessary potential for patient education, disease management, easy follow-up of the treatment process, motivation boosting, and medication adherence improvement.46 In this review, only the existing applications in this field were examined while the present study investigated m-health-based interventions in improving self-care and adherence.
A report study from the World Health Organization about health commitment has pointed out that the amount of adherence to health that is being observed in developed countries is 50%; however, this percentage is extremely lower in developing countries. In this report, patients’ poor health outcomes and increased healthcare costs were the two main consequences of treatment non-adherence.21 The complexity of the medication regimen, patients’ concerns about side effects, and lack of knowledge of patients about the importance of treatment adherence can be mentioned among the reasons for the treatment of non-adherence.58 Adherence to treatment and healthy lifestyle behaviors (including appropriate diet and adequate physical activity) is an important and effective option in controlling chronic diseases.59 The benefits of prescribed medical treatment adherence and lifestyle modification should be trained since they are key components in controlling chronic conditions.10 M-health technology is a promising approach to dealing with poor treatment adherence.10,60 Some studies have confirmed the positive effect of m-health interventions in improving treatment and adherence to healthy lifestyle behaviors. In patients with hypertension and those receiving liver transplants, the use of smartphone applications has improved medication adherence.60,61
One of the advantages of m-health technology, which is an appropriate approach for treatment adherence, is that it can act as a reminder.22 An RCT study represented that the use of reminder SMS in people taking multiple drugs has a significant role in medication self-management.23 In a review study by Dupuis et al, it was emphasized that the use of m-health can reduce the care burden of health systems and have a significant impact on better disease control, treatment adherence, and reduction of drug side effects. The above-mentioned study, in contrast to our study which considered a variety of m-health interventions, considered and examined application-based interventions and stated that the design of applications that are appropriate to the elderly population can be effective in empowering and attracting their interest in the use of smartphones and available applications.5
In their review study, Safdari et al concluded that m-health technology could be effective in controlling the health of older patients. They examined the benefits of using this technology in various aspects of health services and the overall health of the elderly, focusing on the challenges of using this technology. Although the aim of this study was to evaluate m-health in the elderly, the exact age range in the study was not mentioned, and the studies included in their research were not limited to a specific design. However, the present study specifically evaluated the impact of m-health technology on self-care and adherence, included only RCT studies that had stronger evidence, and considered a specific age range (above 50 years). In addition, the keywords and timespan for search in these two studies were different.62
An umbrella review was conducted by Marcolino et al. In this study, systematic reviews covering the effectiveness of m-health interventions were investigated, and the results demonstrated the positive impact of various types of interventions such as SMS, sensors, voicemails, and phone counseling by some devices, including mobile phones, smartphones, personal digital assistants, and the like, on chronic and non-communicable diseases. In this study, no specific age range was considered for patients, while the target of the current study was the elderly. In addition, the purpose of this study was to support the management of chronic diseases, change health behavior, and the like, while the main purpose of the present study was to examine m-health self-care and adherence.18
Elderly people use m-health technology less for some reasons such as a lack of interest in mobile technology, poor digital skills and knowledge, insufficient confidence in learning new skills, and disabilities due to aging such as visual or cognitive impairments.6,63 Attempts need to be made so that age-related physical and cognitive changes would not hinder the use of m-health technology.64 Some mobile manufacturers are attempting to make this device a simple and accessible tool for the elderly.6 Proper design and training can make the desired interaction of people with this technology possible.64 M-health interventions can reduce patients’ sense of isolation, improve self-efficacy and quality of life, and lead to better communication between the elderly and their caregivers.11,65 Therefore, due to the growing trend of the elderly population in the world and Iran, focusing on m-health technology has several benefits for these people and can have positive social and economic effects in communities by creating new job opportunities and reducing the cost and burden of healthcare. The low cost of mobile-based applications and the possibility of customizing the interventions for various patient groups are the potentials of these interventions. M-health has the potential to improve the quality and efficiency of care in low- and middle-income countries.66 The improvement of health information systems and medical technologies should be on the agenda of the government and be financed to provide services in the context of m-health in these countries.66,67
Adverse health situations increased during the COVID-19 pandemic. However, M-health has been used as a solution and has become a suitable strategy for accessing health services.68 The use of m-health technologies for the elderly population is a basic principle in planning and providing health-related services to this vulnerable age group, considering their specific physical, economic, and social characteristics.69 There are several benefits to using companion health in the elderly, the most important of which are saving money, improving interaction with the provision of service providers, reducing the stress of receiving care, and improving health status.68,69 It seems that the use of this technology in the conditions of such epidemics can be an efficient way to provide services to the elderly and be effective in improving their health.
One of the limitations of this study is the specific timespan of the search. Although it provides newer and more up-to-date information, it failed to investigate similar studies that were outside the timespan. Finally, including various diseases may increase heterogeneity, and providing firm conclusions is challenging. On the other hand, considering a specific age range was one of the strengths of the present study. Although the number of obtained studies was limited, it led to more coherent and specific conclusions.
Conclusions
Due to the lack of a review study on the impact of m-health on self-care and adherence in the elderly, the present study was conducted with a wide range of considerations. Since self-care and adherence skills and behaviors should be improved as a result of the use of m-health technology, using this technology to help patients and their caregivers and reducing the care burden of healthcare systems are recommended in this regard. It is also suggested that applications be designed based on sociocultural and economical differences of the communities. The findings of this study can also help in designing more specific and detailed studies according to different factors such as disease, type of intervention, healthoutcome, or population of specific patients. Future studies can shed light on the reasons behind populations with low engagement and provide solutions on how to motivate people to use these applications. Eventually, policymakers could provide sustainable financing to facilitate access to m-health for various groups of people.
Acknowledgments
The authors would like to express their gratitude to Dr. Bahareh Malmir, Ph.D. in Applied Linguistics, who edited the language issues of the present article.
Funding
None.
Data availability statement
Not applicable.
Ethical approval
Not applicable.
Consent for publication
Not applicable.
Conflict of interests
The authors declare that there is no conflict of interests.
References
- Borrero AF, Vasques J, Vargas R. Implementation of a mobile application to promote self-care in elder diabetic patients. In: Braidot A, Hadad A, eds. VI Latin American Congress on Biomedical Engineering CLAIB 2014, Paraná, Argentina 29, 30 & 31 October 2014. Cham Springer; 2015. p. 797-800. 10.1007/978-3-319-13117-7_203.
- Thomas-Purcell KB, Jacobs RJ, Seidman TL, Acevedo A, Waldrop-Valverde D, Ownby RL. A mixed analysis approach to elucidate the multiple chronic condition experience of English- and Spanish-speaking older adults. Clin Interv Aging 2019; 14:407-18. doi: 10.2147/cia.s193215 [Crossref] [ Google Scholar]
- Dallosso H, Yates T, Mani H, Gray LJ, Dhalwani N, Baldry E. Movement through Active Personalised engagement (MAP) - a self-management programme designed to promote physical activity in people with multimorbidity: study protocol for a randomised controlled trial. Trials 2018; 19(1):576. doi: 10.1186/s13063-018-2939-2 [Crossref] [ Google Scholar]
- Guo Y, Chen Y, Lane DA, Liu L, Wang Y, Lip GYH. Mobile health technology for atrial fibrillation management integrating decision support, education, and patient involvement: mAF app trial. Am J Med 2017;130(12):1388-96.e6. 10.1016/j.amjmed.2017.07.003.
- Dupuis K, Tsotsos LE. Technology for remote health monitoring in an older population: a role for mobile devices. Multimodal Technol Interact 2018; 2(3):43. doi: 10.3390/mti2030043 [Crossref] [ Google Scholar]
- Kuerbis A, Mulliken A, Muench F, Moore AA, Gardner D. Older adults and mobile technology: factors that enhance and inhibit utilization in the context of behavioral health. Int J Ment Health Addict 2017; 2(2):1-11. doi: 10.15761/mhar.1000136 [Crossref] [ Google Scholar]
- Chouvarda IG, Goulis DG, Lambrinoudaki I, Maglaveras N. Connected health and integrated care: toward new models for chronic disease management. Maturitas 2015; 82(1):22-7. doi: 10.1016/j.maturitas.2015.03.015 [Crossref] [ Google Scholar]
- Toh MR, Teo V, Kwan YH, Raaj S, Tan SY, Tan JZ. Association between number of doses per day, number of medications and patient’s non-compliance, and frequency of readmissions in a multi-ethnic Asian population. Prev Med Rep 2014; 1:43-7. doi: 10.1016/j.pmedr.2014.10.001 [Crossref] [ Google Scholar]
- Yap AF, Thirumoorthy T, Kwan YH. Medication adherence in the elderly. J Clin Gerontol Geriatr 2016; 7(2):64-7. doi: 10.1016/j.jcgg.2015.05.001 [Crossref] [ Google Scholar]
- Johnston N, Bodegard J, Jerström S, Åkesson J, Brorsson H, Alfredsson J. Effects of interactive patient smartphone support app on drug adherence and lifestyle changes in myocardial infarction patients: a randomized study. Am Heart J 2016; 178:85-94. doi: 10.1016/j.ahj.2016.05.005 [Crossref] [ Google Scholar]
- Hardinge M, Rutter H, Velardo C, Shah SA, Williams V, Tarassenko L. Using a mobile health application to support self-management in chronic obstructive pulmonary disease: a six-month cohort study. BMC Med Inform Decis Mak 2015; 15:46. doi: 10.1186/s12911-015-0171-5 [Crossref] [ Google Scholar]
- Lakshminarayan K, Westberg S, Northuis C, Fuller CC, Ikramuddin F, Ezzeddine M. A mHealth-based care model for improving hypertension control in stroke survivors: pilot RCT. Contemp Clin Trials 2018; 70:24-34. doi: 10.1016/j.cct.2018.05.005 [Crossref] [ Google Scholar]
- Levine M, Reid M. Primary care providers’ perspectives on telemedicine in the pharmacologic management of older adults with chronic pain (CP). J Am Geriatr Soc 2012; 60:S202. [ Google Scholar]
- Pfaeffli Dale L, Whittaker R, Jiang Y, Stewart R, Rolleston A, Maddison R. Text message and internet support for coronary heart disease self-management: results from the Text4Heart randomized controlled trial. J Med Internet Res 2015; 17(10):e237. doi: 10.2196/jmir.4944 [Crossref] [ Google Scholar]
- Kim M. Effects of customized long-message service and phone-based health-coaching on elderly people with hypertension. Iran J Public Health 2019; 48(4):655-63. [ Google Scholar]
- Sun C, Sun L, Xi S, Zhang H, Wang H, Feng Y. Mobile phone-based telemedicine practice in older Chinese patients with type 2 diabetes mellitus: randomized controlled trial. JMIR Mhealth Uhealth 2019; 7(1):e10664. doi: 10.2196/10664 [Crossref] [ Google Scholar]
- van den Berg SW, Gielissen MF, Custers JA, van der Graaf WT, Ottevanger PB, Prins JB. BREATH: web-based self-management for psychological adjustment after primary breast cancer--results of a multicenter randomized controlled trial. J Clin Oncol 2015; 33(25):2763-71. doi: 10.1200/jco.2013.54.9386 [Crossref] [ Google Scholar]
- Marcolino MS, Oliveira JAQ, D’Agostino M, Ribeiro AL, Alkmim MBM, Novillo-Ortiz D. The impact of mHealth interventions: systematic review of systematic reviews. JMIR Mhealth Uhealth 2018; 6(1):e23. doi: 10.2196/mhealth.8873 [Crossref] [ Google Scholar]
- Shade M, Boron J, Manley N, Kupzyk K, Pullen C. Ease of use and usefulness of medication reminder apps among rural aging adults. J Community Health Nurs 2019; 36(3):105-14. doi: 10.1080/07370016.2019.1630960 [Crossref] [ Google Scholar]
- Woodman J, Ballard K, Hewitt C, MacPherson H. Self-efficacy and self-care-related outcomes following Alexander Technique lessons for people with chronic neck pain in the ATLAS randomised, controlled trial. Eur J Integr Med 2018; 17:64-71. doi: 10.1016/j.eujim.2017.11.006 [Crossref] [ Google Scholar]
- Mikaili N, Ghasemi MA, Salari S, Sakeni Z. Theoretical and practical dimensions of adherence to treatment in patients: a review study. Med J Mashhad Univ Med Sci 2019; 62(2):1403-19. doi: 10.22038/mjms.2019.14116.[Persian] [Crossref] [ Google Scholar]
- Changizi M, Kaveh MH. Effectiveness of the mHealth technology in improvement of healthy behaviors in an elderly population-a systematic review. Mhealth 2017; 3:51. doi: 10.21037/mhealth.2017.08.06 [Crossref] [ Google Scholar]
- Huang CY, Nguyen PA, Clinciu DL, Hsu CK, Lu JR, Yang HC. A personalized medication management platform (PMMP) to improve medication adherence: a randomized control trial. Comput Methods Programs Biomed 2017; 140:275-81. doi: 10.1016/j.cmpb.2016.12.012 [Crossref] [ Google Scholar]
- Piette JD, Striplin D, Marinec N, Chen J, Trivedi RB, Aron DC. A mobile health intervention supporting heart failure patients and their informal caregivers: a randomized comparative effectiveness trial. J Med Internet Res 2015; 17(6):e142. doi: 10.2196/jmir.4550 [Crossref] [ Google Scholar]
- Bae JW, Woo SI, Lee J, Park SD, Kwon SW, Choi SH. mHealth interventions for lifestyle and risk factor modification in coronary heart disease: randomized controlled trial. JMIR Mhealth Uhealth 2021; 9(9):e29928. doi: 10.2196/29928 [Crossref] [ Google Scholar]
- Ding H, Jayasena R, Chen SH, Maiorana A, Dowling A, Layland J. The effects of telemonitoring on patient compliance with self-management recommendations and outcomes of the innovative telemonitoring enhanced care program for chronic heart failure: randomized controlled trial. J Med Internet Res 2020; 22(7):e17559. doi: 10.2196/17559 [Crossref] [ Google Scholar]
- Becker TAC, de Souza Teixeira CR, Zanetti ML, Pace AE, Almeida FA, da Costa Gonçalves Torquato MT. Effects of supportive telephone counseling in the metabolic control of elderly people with diabetes mellitus. Rev Bras Enferm 2017; 70(4):704-10. doi: 10.1590/0034-7167-2017-0089 [Crossref] [ Google Scholar]
- Crowley MJ, Edelman D, McAndrew AT, Kistler S, Danus S, Webb JA. Practical telemedicine for veterans with persistently poor diabetes control: a randomized pilot trial. Telemed J E Health 2016; 22(5):376-84. doi: 10.1089/tmj.2015.0145 [Crossref] [ Google Scholar]
- Dugas M, Crowley K, Gao GG, Xu T, Agarwal R, Kruglanski AW. Individual differences in regulatory mode moderate the effectiveness of a pilot mHealth trial for diabetes management among older veterans. PLoS One 2018; 13(3):e0192807. doi: 10.1371/journal.pone.0192807 [Crossref] [ Google Scholar]
- Peimani M, Rambod C, Omidvar M, Larijani B, Ghodssi-Ghassemabadi R, Tootee A. Effectiveness of short message service-based intervention (SMS) on self-care in type 2 diabetes: a feasibility study. Prim Care Diabetes 2016; 10(4):251-8. doi: 10.1016/j.pcd.2015.11.001 [Crossref] [ Google Scholar]
- Sarayani A, Mashayekhi M, Nosrati M, Jahangard-Rafsanjani Z, Javadi M, Saadat N. Efficacy of a telephone-based intervention among patients with type-2 diabetes; a randomized controlled trial in pharmacy practice. Int J Clin Pharm 2018; 40(2):345-53. doi: 10.1007/s11096-018-0593-0 [Crossref] [ Google Scholar]
- Tan CCL, Cheng KKF, Hwang SW, Zhang N, Holroyd E, Wang W. Effect of a diabetes self-efficacy enhancing program on older adults with type 2 diabetes: a randomized controlled trial. Clin Nurs Res 2020; 29(5):293-303. doi: 10.1177/1054773818792480 [Crossref] [ Google Scholar]
- Kim JY, Wineinger NE, Steinhubl SR. The influence of wireless self-monitoring program on the relationship between patient activation and health behaviors, medication adherence, and blood pressure levels in hypertensive patients: a substudy of a randomized controlled trial. J Med Internet Res 2016; 18(6):e116. doi: 10.2196/jmir.5429 [Crossref] [ Google Scholar]
- Griauzde D, Kullgren JT, Liestenfeltz B, Ansari T, Johnson EH, Fedewa A. A mobile phone-based program to promote healthy behaviors among adults with prediabetes who declined participation in free diabetes prevention programs: mixed-methods pilot randomized controlled trial. JMIR Mhealth Uhealth 2019; 7(1):e11267. doi: 10.2196/11267 [Crossref] [ Google Scholar]
- Anderson AS, Craigie AM, Gallant S, McAdam C, Macaskill EJ, Mutrie N. Randomised controlled trial to assess the impact of a lifestyle intervention (ActWELL) in women invited to NHS breast screening. BMJ Open 2018; 8(11):e024136. doi: 10.1136/bmjopen-2018-024136 [Crossref] [ Google Scholar]
- Miller DP Jr, Denizard-Thompson N, Weaver KE, Case LD, Troyer JL, Spangler JG. Effect of a digital health intervention on receipt of colorectal cancer screening in vulnerable patients: a randomized controlled trial. Ann Intern Med 2018; 168(8):550-7. doi: 10.7326/m17-2315 [Crossref] [ Google Scholar]
- Coultas DB, Jackson BE, Russo R, Peoples J, Singh KP, Sloan J. Home-based physical activity coaching, physical activity, and health care utilization in chronic obstructive pulmonary disease Chronic obstructive pulmonary disease self-management activation research trial secondary outcomes. Ann Am Thorac Soc 2018; 15(4):470-8. doi: 10.1513/AnnalsATS.201704-308OC [Crossref] [ Google Scholar]
- Abaza H, Marschollek M. SMS education for the promotion of diabetes self-management in low & middle income countries: a pilot randomized controlled trial in Egypt. BMC Public Health 2017; 17(1):962. doi: 10.1186/s12889-017-4973-5 [Crossref] [ Google Scholar]
- Fors A, Blanck E, Ali L, Ekberg-Jansson A, Fu M, Lindström Kjellberg I. Effects of a person-centred telephone-support in patients with chronic obstructive pulmonary disease and/or chronic heart failure - a randomized controlled trial. PLoS One 2018; 13(8):e0203031. doi: 10.1371/journal.pone.0203031 [Crossref] [ Google Scholar]
- Frias J, Virdi N, Raja P, Kim Y, Savage G, Osterberg L. Effectiveness of digital medicines to improve clinical outcomes in patients with uncontrolled hypertension and type 2 diabetes: prospective, open-label, cluster-randomized pilot clinical trial. J Med Internet Res 2017; 19(7):e246. doi: 10.2196/jmir.7833 [Crossref] [ Google Scholar]
- Piette JD, Marinec N, Janda K, Morgan E, Schantz K, Yujra AC. Structured caregiver feedback enhances engagement and impact of mobile health support: a randomized trial in a lower-middle-income country. Telemed J E Health 2016; 22(4):261-8. doi: 10.1089/tmj.2015.0099 [Crossref] [ Google Scholar]
- Aminuddin HB, Jiao N, Jiang Y, Hong J, Wang W. Effectiveness of smartphone-based self-management interventions on self-efficacy, self-care activities, health-related quality of life and clinical outcomes in patients with type 2 diabetes: a systematic review and meta-analysis. Int J Nurs Stud 2021; 116:103286. doi: 10.1016/j.ijnurstu.2019.02.003 [Crossref] [ Google Scholar]
- Harashima SI, Nishimura A, Inagaki N. Attitudes of patients and physicians to insulin therapy in Japan: an analysis of the Global Attitude of Patients and Physicians in Insulin Therapy study. Expert Opin Pharmacother 2017; 18(1):5-11. doi: 10.1080/14656566.2016.1260547 [Crossref] [ Google Scholar]
- Schnell O, Klausmann G, Gutschek B, Garcia-Verdugo RM, Hummel M. Impact on diabetes self-management and glycemic control of a new color-based SMBG meter. J Diabetes Sci Technol 2017; 11(6):1218-25. doi: 10.1177/1932296817706376 [Crossref] [ Google Scholar]
- Mohamadzadeh Larijan H, Nikravan A, Aeenparast A. The role of hospital intervention in prevention of diabetes in pre-diabetes patients. Payesh 2019;18(5):465-73. [Persian].
- Molaei K, Ahmadi M. The role of mobile health apps to facilitate self-care. Journal of Modern Medical Information Sciences 2017;3(1):44-55. [Persian].
- Criner GJ, Bourbeau J, Diekemper RL, Ouellette DR, Goodridge D, Hernandez P. Prevention of acute exacerbations of COPD: American College of Chest Physicians and Canadian Thoracic Society Guideline. Chest 2015; 147(4):894-942. doi: 10.1378/chest.14-1676 [Crossref] [ Google Scholar]
- Rodrigues R, Shet A, Antony J, Sidney K, Arumugam K, Krishnamurthy S. Supporting adherence to antiretroviral therapy with mobile phone reminders: results from a cohort in South India. PLoS One 2012; 7(8):e40723. doi: 10.1371/journal.pone.0040723 [Crossref] [ Google Scholar]
- Tucker JA, Simpson CA, Huang J, Roth DL, Stewart KE. Utility of an interactive voice response system to assess antiretroviral pharmacotherapy adherence among substance users living with HIV/AIDS in the rural South. AIDS Patient Care STDS 2013; 27(5):280-6. doi: 10.1089/apc.2012.0322 [Crossref] [ Google Scholar]
- van Heerden A, Tomlinson M, Swartz L. Point of care in your pocket: a research agenda for the field of m-health. Bull World Health Organ 2012; 90(5):393-4. doi: 10.2471/blt.11.099788 [Crossref] [ Google Scholar]
- Thirumurthy H, Lester RT. M-health for health behaviour change in resource-limited settings: applications to HIV care and beyond. Bull World Health Organ 2012; 90(5):390-2. doi: 10.2471/blt.11.099317 [Crossref] [ Google Scholar]
- Anderson K, Burford O, Emmerton L. Mobile health apps to facilitate self-care: a qualitative study of user experiences. PLoS One 2016; 11(5):e0156164. doi: 10.1371/journal.pone.0156164 [Crossref] [ Google Scholar]
- Chiu CJ, Yu YC, Du YF, Yang YC, Chen JY, Wong LP. Comparing a social and communication app, telephone intervention, and usual care for diabetes self-management: 3-arm quasiexperimental evaluation study. JMIR Mhealth Uhealth 2020; 8(6):e14024. doi: 10.2196/14024 [Crossref] [ Google Scholar]
- Bee YM, Batcagan-Abueg AP, Chei CL, Do YK, Haaland B, Goh SY. A smartphone application to deliver a treat-to-target insulin titration algorithm in insulin-naive patients with type 2 diabetes: a pilot randomized controlled trial. Diabetes Care 2016; 39(10):e174-6. doi: 10.2337/dc16-0419 [Crossref] [ Google Scholar]
- McManus RJ, Mant J, Franssen M, Nickless A, Schwartz C, Hodgkinson J. Efficacy of self-monitored blood pressure, with or without telemonitoring, for titration of antihypertensive medication (TASMINH4): an unmasked randomised controlled trial. Lancet 2018; 391(10124):949-59. doi: 10.1016/s0140-6736(18)30309-x [Crossref] [ Google Scholar]
- Chen C, Li X, Sun L, Cao S, Kang Y, Hong L. Post-discharge short message service improves short-term clinical outcome and self-care behaviour in chronic heart failure. ESC Heart Fail 2019; 6(1):164-73. doi: 10.1002/ehf2.12380 [Crossref] [ Google Scholar]
- Hartz J, Yingling L, Powell-Wiley TM. Use of mobile health technology in the prevention and management of diabetes mellitus. Curr Cardiol Rep 2016; 18(12):130. doi: 10.1007/s11886-016-0796-8 [Crossref] [ Google Scholar]
- Cook KA, Modena BD, Simon RA. Improvement in asthma control using a minimally burdensome and proactive smartphone application. J Allergy Clin Immunol Pract 2016;4(4):730-7.e1. 10.1016/j.jaip.2016.03.005.
- Browning RB, McGillicuddy JW, Treiber FA, Taber DJ. Kidney transplant recipients’ attitudes about using mobile health technology for managing and monitoring medication therapy. J Am Pharm Assoc (2003) 2016;56(4):450-4.e1. 10.1016/j.japh.2016.03.017.
- Mrosek R, Dehling T, Sunyaev A. Taxonomy of health IT and medication adherence. Health Policy Technol 2015; 4(3):215-24. doi: 10.1016/j.hlpt.2015.04.003 [Crossref] [ Google Scholar]
- Márquez Contreras E, Márquez Rivero S, Rodríguez García E, López-García-Ramos L, Carlos Pastoriza Vilas J, Baldonedo Suárez A. Specific hypertension smartphone application to improve medication adherence in hypertension: a cluster-randomized trial. Curr Med Res Opin 2019; 35(1):167-73. doi: 10.1080/03007995.2018.1549026 [Crossref] [ Google Scholar]
- Safdari R, Shams Abadi AR, Pahlevany Nejad S. Improve health of the elderly people with m-health and technology. Iran J Ageing 2018; 13(3):288-99. doi: 10.32598/sija.13.3.288.[Persian] [Crossref] [ Google Scholar]
- Arning K, Ziefle M. Understanding age differences in PDA acceptance and performance. Comput Human Behav 2007; 23(6):2904-27. doi: 10.1016/j.chb.2006.06.005 [Crossref] [ Google Scholar]
- Nelson LA, Wallston KA, Kripalani S, Greevy RA Jr, Elasy TA, Bergner EM. Mobile phone support for diabetes self-care among diverse adults: protocol for a three-arm randomized controlled trial. JMIR Res Protoc 2018; 7(4):e92. doi: 10.2196/resprot.9443 [Crossref] [ Google Scholar]
- Huo X, Spatz ES, Ding Q, Horak P, Zheng X, Masters C. Design and rationale of the Cardiovascular Health and Text Messaging (CHAT) Study and the CHAT-Diabetes Mellitus (CHAT-DM) Study: two randomised controlled trials of text messaging to improve secondary prevention for coronary heart disease and diabetes. BMJ Open 2017; 7(12):e018302. doi: 10.1136/bmjopen-2017-018302 [Crossref] [ Google Scholar]
- Lopéz DM, Blobel B. mHealth in low- and middle-income countries: status, requirements and strategies. Stud Health Technol Inform 2015; 211:79-87. doi: 10.3233/978-1-61499-516-6-79 [Crossref] [ Google Scholar]
- Nelson LA, Mulvaney SA, Gebretsadik T, Ho YX, Johnson KB, Osborn CY. Disparities in the use of a mHealth medication adherence promotion intervention for low-income adults with type 2 diabetes. J Am Med Inform Assoc 2016; 23(1):12-8. doi: 10.1093/jamia/ocv082 [Crossref] [ Google Scholar]
- Rostam Niakan Kalhori S, Bahaadinbeigy K, Deldar K, Gholamzadeh M, Hajesmaeel-Gohari S, Ayyoubzadeh SM. Digital health solutions to control the COVID-19 pandemic in countries with high disease prevalence: literature review. J Med Internet Res 2021; 23(3):e19473. doi: 10.2196/19473 [Crossref] [ Google Scholar]
- Astley CM, Clarke RA, Cartledge S, Beleigoli A, Du H, Gallagher C. Remote cardiac rehabilitation services and the digital divide: implications for elderly populations during the COVID19 pandemic. Eur J Cardiovasc Nurs 2021; 20(6):521-3. doi: 10.1093/eurjcn/zvab034 [Crossref] [ Google Scholar]