Int J Aging. 2024;2:e21.
doi: 10.34172/ija.2024.e21
Original Article
Challenges and Solutions to Improve the Provision of Oral and Dental Health Services for the Iranian Older people: A Qualitative Study
Saber Azami-Aghdash 1  , Mahdieh Asghari 2, Shahin Karami 3, Mehdi Rostampour 4, Elahe Safari 2, Shima Rastkar-Gharamaleki 5, *
, Mahdieh Asghari 2, Shahin Karami 3, Mehdi Rostampour 4, Elahe Safari 2, Shima Rastkar-Gharamaleki 5, * 
Author information:
1Tabriz Health Services Management Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
2Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran
3FH Wien der WKW, Vienna, Austria
4Medical Philosophy and History Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
5School of Management and Medical Informatics, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Objectives:
To examine the challenges of providing oral and dental health services for the Iranian older people and strategies to improve them.
Design:
A qualitative study.
Setting(s):
Iran’s health system consisting of units that provide oral and dental health services to aging people.
Participants:
Opinion-holders and service providers were selected using a purposive sampling method. Semi-structured interviews were used to collect information, and the content-analysis method was utilized for data analysis.
Outcome measures:
challenges of providing oral and dental health services for the Iranian older people and strategies to improve them.
Results:
Three main topics were identified, including problems in the health system and service delivery system, problems related to older people, and socio-economic problems, along with 16 sub-topics. The solutions included the existence of a written program, guidelines, and instructions for providing services and training, empowering health system employees regarding oral and dental hygiene and training specialists, appropriate insurance coverage for the services received, monitoring and evaluation of the services provided, and regular follow-ups of older people. The other solutions were strengthening the referral system, providing suitable service packages for different levels of service provision, and involving various organizations to provide oral and dental health services to aging people.
Conclusions:
The most important challenges in providing oral and dental health services to the aging population of Iran were identified in this study, and solutions were presented to improve them accordingly. It is anticipated that the officials and guardians in this area will focus on necessary plans and measures to enhance the oral and dental health of older people.
Keywords: Older people, Oral and dental health, Program
Copyright and License Information
© 2024 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
The research protocol was approved & supported by School of Management and Medical Informatics; Tabriz University of Medical Sciences: [Grant number:63307].
Please cite this article as follows: Azami-Aghdash S, Asghari M, Karami S, Rostampour M, Safari E, Rastkar-Gharamaleki S. Challenges and solutions to improve the provision of oral and dental health services for the Iranian older people: a qualitative study. Int J Aging. 2024;2: e21. doi: 10.34172/ija.2024.e21
Introduction
One of the most significant phenomena of the 20th century is the rapid aging of the world’s population.1,2 Low- and middle-income countries will have 80% of the world’s older population by 2050.3 As one gets older, the human body undergoes significant changes, resulting in a gradual decrease in physical and mental health, increasing the chance of contracting various diseases.4 In the meantime, oral and dental health problems are a concern for older people. Overall, oral and dental hygiene is a multifaceted phenomenon that is known as a crucial factor in enhancing the quality of life.5 Issues such as difficulty in swallowing and chewing, loss of appetite, decreased self-confidence, social isolation, and overall quality of life can all be affected by oral health. Accordingly, it is vital to deal with these oral and dental health concerns.4-7 It has been demonstrated that oral and dental diseases affect three and a half billion people worldwide.8 Tooth decay and periodontal disease are the most common oral problems among older people. More than half of older people population has moderate or severe periodontal disease.7,8 In Iran, according to forecasts, the population of older people will reach 12% of the total population by 2025.4 According to reports, the oral and dental hygiene of older Iranians is generally poor, with about 84.8% of the population experiencing complete or partial tooth loss.6 A study in Tabriz has shown that 51% of older people population have a lower-than-average quality of life regarding oral and dental health.9 According to evidence, the percentage of toothlessness is high among aging people in Torbat Heydarieh, and education and care can help reduce it.10
Prevention of oral and dental diseases in older people in Iran has received less attention,11 even health insurance in countries such as Iran does not pay much for dental services, and there is no special screening program for older people.12 The provision of oral and dental health services requires a trustee to be specified, along with defining its position and duties following their provision.13 In addition, according to the information obtained from the program of integrated healthcare for older people, oral and dental health has not been considered along with other mentioned chronic diseases. This issue should be taken into consideration along with people-associated diseases as people age. The risk factors and clinical symptoms of oral and dental diseases should be included in this program for quick diagnosis, and the necessary training should be given to health service providers and non-physicians in this regard.14
Despite the widespread problems of oral and dental health among older people population, in recent years, most of the focus on providing oral and dental health services has been directed to a specific population other than older people, namely, pregnant women and children.12 The prevention of oral and dental diseases in aging people has not received enough attention. Considering the lack of comprehensive services in the field of oral and dental healthcare for older people, there is a need to comprehensively examine the challenges and obstacles in providing oral and dental health services to aging people from the perspective of experts, officials, service providers, and older people themselves. Further, solutions to solve these challenges and obstacles, as well as improving service delivery, can play a significant role in improving the oral and dental health status of aging people. Based on the results of the initial literature review and the researchers’ experiences, no comprehensive study has so far scientifically presented these challenges and solutions. On the other hand, the presence of this information is highly vital for planning and making the right decision. Therefore, this study aims to investigate the challenges of providing oral and dental health services for the Iranian older people and methods to improve them.
Methods
This qualitative study was conducted in Tabriz in 2022. Considering that the current study aimed to describe the existing conditions (challenges) and provide solutions to improve them in the field of providing oral and dental health services to older people, a qualitative descriptive approach was used. This approach, by using the systematic collection of data to reach a stage of recognition and description of the subject under study, enables the researcher to create a clear picture of the phenomenon under study, and for this reason, it is a suitable approach for research where there is insufficient information and knowledge in similar and field studies.15
Study Participants
The participants of this study are experts and specialists in the field of dentistry, experts and specialists in the field of primary healthcare (especially oral and dental health groups and population and family health groups), and other professors who work in the field of aging. Moreover, researchers in the field of geriatrics and dental sciences established related research centers.
The inclusion criteria for experts and specialists in the field of dentistry:
-
Having at least 2 years of work experience
-
Having an interest and sufficient knowledge in the studied subject
-
Having the desire and ability to participate in the study
The inclusion criteria for experts in the field of primary healthcare
-
Having at least 2 years of work experience and activities related to older people
-
Working in primary healthcare
-
Having an interest in the subject being studied
-
Having the desire and ability to participate in the study
The inclusion criteria for expert professors in the field of geriatrics and dental sciences
-
Having at least 5 years of work experience
-
Having at least 2 articles or books published in the field of study
-
Having an interest in the subject being studied
-
Having the desire and ability to participate in the study
Sample Size and Sampling Method
The current study began with the selection of participants using the purposive sampling method, which aimed to select the interviewees who could provide the most information. A group of participants was chosen that was as diverse as possible, with participants representing different specializations, fields of study, levels of education, and work experience. The theoretical sampling method was employed to select the next participants in other specialized fields based on ideas gained from the initial interviewees’ opinions. Sampling was continued until reaching information saturation. In the present study, the researchers reached relative saturation after conducting 9 interviews, but for sure, the interviews were continued until the 11th participant.
Data Collection Method
The required data were collected using semi-structured interviews with people participating in the study. With the consent of the participants, their views were recorded and transcribed word by word immediately after the completion of each interview. In addition, notes were taken during the interviews, and the interviews were conducted using the interview guide form (Supplementary file 1). This form was developed based on the opinions of experts and the initial literature review regarding the subject. There are only a few questions in this guide that range from general to specific and ask for open-ended and interpretive answers. The interviews started on January 20, 2021 and continued until April 19, 2021. Face-to-face interviews were used to collect data from the eight available participants, and the interviewers attended the interviewees’ workplaces with prior coordination. Three interviews were also conducted online. The languages of the interviews were Azari and Persian, and it took approximately three months to conduct interviews with the experts.
Data Extraction and Analysis Method
Content analysis was employed to analyze the data, a method that involves identifying, analyzing, and reporting themes in the text. Two researchers were responsible for data coding. First, the texts were merged and read several times, and the primary codes were extracted from the text itself. In addition, themes were formed according to the codes. Further, the codes and themes were classified, and then two coders were used to ensure the reliability of the codes.
Four criteria suggested by Guba and Lincoln were used to increase the rigor and accuracy of the study results. Credibility and confirmability were utilized in this case through long-term engagement, reviews by colleagues and participants, and the use of expert opinions. In this way, after finishing the meetings and summarizing people’s opinions, a summary of the people’s statements was provided to the people from the notes made during the meetings to correct and eliminate the wrong and ambiguous content. As regards verifiability, two people were used for coding, and the reliability of the information was measured. In terms of transferability, the opinions of experts and purpose-based sampling were utilized, and the amount of use of this information at other times and places underwent evaluation.
Results
Most of the interviewees were male and had general doctorates and specialized doctorates (Table 1).
Table 1.
Demographic Characteristics of the Participants in the Interviews to Examine the Existing Conditions (Challenges) and Provide Solutions to Improve the Provision of Oral and Dental Health Services for Older People in Iran
|
Variables
|
Variable Levels
|
Frequency
|
| Gender |
Male |
8 |
| Female |
3 |
| Occupational group |
Oral health expert |
2 |
| Responsible for specialized training |
1 |
| Director of Oral Health Department |
1 |
| Specialist assistant in the Department of Mouth, Jaw, and Face Diseases |
1 |
| General dentist |
1 |
| Oral and dental health officer of the city |
1 |
| Assistant Professor of Health Management and Policy Department |
1 |
| Associate Professor of Health Education and Health Promotion Department |
1 |
| Ph.D. student in geriatric health |
1 |
| Specialist doctorate in dentistry |
1 |
| Education level |
General Ph.D. |
4 |
| Ph.D. |
4 |
| Bachelors and Masters |
3 |
Interviews with experts in different specialties yielded information that was categorized into challenges and solutions to enhance service delivery (Figure 1).
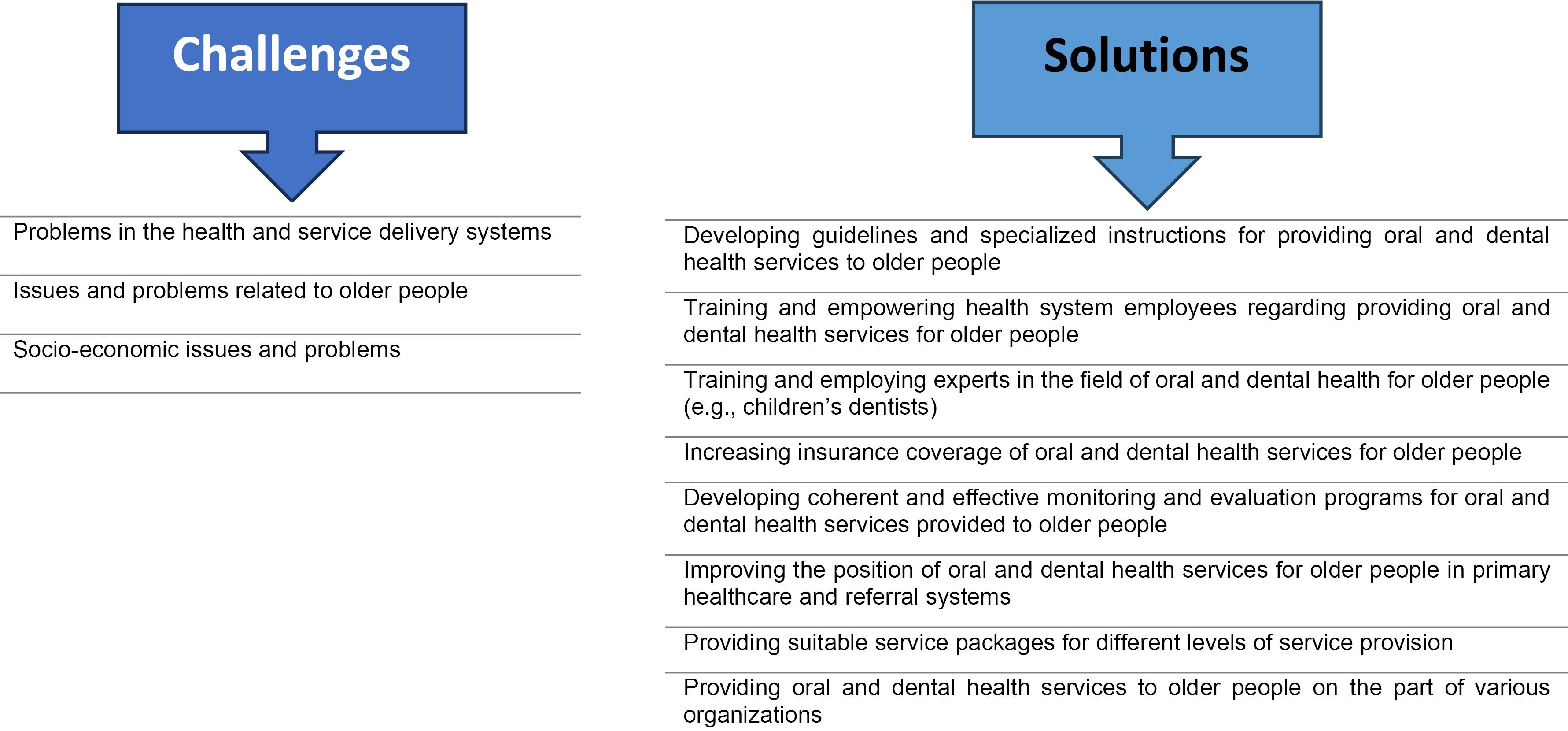
Figure 1.
Challenges and Solutions for Providing Oral and Dental Health Services for Iranian Aging People
.
Challenges and Solutions for Providing Oral and Dental Health Services for Iranian Aging People
Challenges of Providing Oral Health Services to Older People
Examining the opinions of experts regarding the current situation of providing oral and dental health services for older people revealed many challenges in the country’s health system and the lifestyle of older people, which were divided into three main themes and 16 sub-themes (Table 2).
Table 2.
Experts’ Opinions on the Challenges of Providing Oral and Dental Health Services for Older People in Iran
|
Theme
|
Sub-theme
|
Frequency of Repetition in Interviews
|
| Problems in health and service delivery systems |
High costs of dental services |
3 |
| Lack of proper insurance coverage |
1 |
| The lack of an integrated structure and specific trustee to provide oral and dental health services to older individuals |
1 |
| Provision of more dental services by the private sector |
3 |
| Providers are willing to offer clinical services instead of preventive services |
2 |
| Weakness in providing basic services at primary levels (lack of specific and clear programs or services for older people) |
5 |
| The lack of experts and specialists who are knowledgeable about oral and dental health issues for older people |
3 |
| A shortage of dentists |
1 |
| Issues related to dental schools, such as the absence of special courses for oral health problems in older people |
3 |
| Failure to provide the specialized and advanced services needed for older people (providing completely simple and beginner services) |
3 |
| Issues and problems related to older people |
Poor oral health status (high use of dentures, high toothlessness, caries, gum infection, high decayed, missing, and filled teeth, and the like) |
3 |
| Increasing demand due to the aging of the population |
1 |
| The lack of adequate knowledge and information among older people and a lack of proper culture |
2 |
| Socio-economic issues and problems |
Low financial ability and poor income status of older people |
2 |
| Failure by the government to allocate sufficient funds for service providers |
1 |
| Changes in the lifestyle of older people |
2 |
In line with the problems and challenges in the health and service delivery systems, the high costs of treatment and oral healthcare for older people, the lack of adequate insurance coverage, and the lack of an integrated structure and a clear trustee for providing oral health services for older people have been reported by most experts. Participant 9 mentioned the exorbitant costs of the dental department, stating that the majority of dental services are provided in offices, increasing costs for older individuals. Participant 12, referring to the high cost of dental equipment and raw materials for the treatment of oral and dental diseases, indicated that “Dental services are relatively expensive in the country, which is partly due to the high cost of the equipment and essentials of these services. Perhaps, in the field of health, no service is as dependent on materials, supplies, and equipment as dental services, and unfortunately, at the end of 2019, the prices of consumables required for conventional dental services increased several times. Moreover, in our country, statistically, the rate of out-of-pocket payments for dental services is usually high, and it accounts for an important share. Therefore, the development of any kind of dental services, especially at the standard level, is a matter of gratitude”. Additionally, regarding the lack of proper insurance coverage, he mentioned, “Regarding the lack of adequate insurance coverage for dental services, unfortunately, people do not come early and rarely come to receive these services. In addition, per capita visits to the dentist are extremely low, and we are far away from the global standard”. Regarding the structure of the health system, participant 9 admitted, “In the field of oral and dental health for older people, there is no proper and integrated structure for providing services, and most service-providing centers work according to taste, and the services are not integrated. There is no specific trustee to provide services to older people, and in general, we are facing many challenges in this regard”. However, due to the lack of strength, structural weakness, and lack of sufficient support, this group is not given such importance, especially their mouth and teeth. Several participants stated that the private sector is the main provider of dental services, and providers generally concentrate on clinical rather than preventive services. For example, participant 5 declared that “Dental services are mostly provided by the private sector. In addition, in this regard, participant 9 noted that “Since most dental services are provided in private offices, dentists care more about the patient’s clinical issues than prevention and education issues. Participant 1 also stated that “Older people visit private clinics if they are aware of their oral health status”.
Most experts pointed out the weakness in providing basic services at the primary levels, the lack of experts and specialists who are aware of oral and dental health issues for older people, the lack of dentists, problems related to dental schools (the lack of curriculum or a community-oriented perspective), and the lack of specialized and advanced service provision for older people. For example, participant 10 mentioned, “There is no concrete and defined program to provide services for older people, and oral and dental training courses for health workers and caregivers to perform oral and dental examinations of older people are not conducted effectively”. Participant 3 added, “Most of the investment in the health sector is for children, particularly for providing them with preventive services such as fissure sealant and fluoride therapy, rather than investing in the real needs of older people. Further, participant 1 indicated, “There is no specific and clear program or service for older people at different levels, especially low levels, in health centers such as geriatric dentistry, and there is no clear guideline or instruction for how to provide special services for older people”. Participant 9 added, “There is no specific and defined structure for the oral and dental health of older people, and in terms of health and clinical issues, the condition of the oral and dental health of this group of people has shown a decline”.
Regarding the lack of providing proper services to older people, participant 1 asserted that “Oral and dental health services are only provided in the area of little knowledge of the dentist and caregiver. While the medications and medical conditions of older people are different from each other, these things should be taken into account in providing the service, which is not unfortunately the case. Furthermore, in the centers, the necessary recommendations should be provided regarding the drugs used and the relationship these drugs have with the oral and dental conditions of older people to prevent more advanced oral, dental, and other problems, which unfortunately rarely receive attention. For example, blood pressure medicine, which has a direct relationship with the reduction of saliva secretion, which makes a person susceptible to tooth decay”. In line with the lack of experts and specialists aware of oral and dental health issues, as well as the lack of manpower, participant 8 declared, “There are no experts in the health centers who are knowledgeable about the issues of older people or experts in the field of oral and dental health for older people”. Moreover, Participant 10 pointed out that “There is no dentist force to be stationed in all the health centers, and we are facing a lack of manpower”. Additionally, participant 8 mentioned that “There are no experts in the health centers who are aware of the issues of older people or experts and knowledgeable in the field of oral and dental health of older people”. Participant 10 added, “There are no oral and dental training courses for healthcare workers to perform examinations and provide the services needed by older people”.
The information obtained from the interviews indicated that there is no separate curriculum and a community-oriented approach to providing oral and dental health services to older people, and for this reason, specialized services are not provided to these people. Participant 1 mentioned that “There is no separate course unit for geriatric dentistry in dental schools”. Participant 9 also declared that “There is no special course for geriatric dentistry in medical schools, and education about geriatrics is not provided for the students”. Many participants claimed that there are no specialized dental services for older people in Iran. For example, participant 4 indicated that “Specialized dental services for older people that are fully suited to the conditions of this group of people do not exist in Iran...” In this regard, participant 3 mentioned that “In urban and rural health centers, quite simple and beginner services for older people, including simple repairs, tooth extraction, and basic consultations such as doing the necessary things to stop the blood after tooth extraction, are provided for them, even when the dentist is present at the center. Participant 4 also added, “Specialized dental services for older people that are fully suited to the conditions of this group do not exist in Iran, and the dental services for older people are summarized at two levels”.
In addition to these cases, a series of problems and issues related to the aging period and socio-economic issues and problems were extracted from the interviews. Most of the interviewees believed that oral and dental diseases of older people have a higher prevalence, indicating incorrect lifestyle, lack of sufficient information and knowledge, increasing age and need, and lack of budget allocation for this group. In this regard, participant 2 pointed out that “there are deplorable conditions in the oral and dental health of older people, and toothlessness, decay, and gum infection are rampant among older people”. Participant 1 also admitted, “The high percentage of tooth loss among adults is very high, so that 70% or 80% of adults report decayed, missing, and filled teeth above 20%. Additionally, the use of dentures is very high during this period, and most seniors use full dentures”.
Further, participant 12 said: “In our country, due to the late referral and the exorbitant costs of these services, unfortunately, the number of tooth extractions instead of restorative services is much higher than the world standard, and more than 50% of Iranian aging people are toothless, and the index of tooth decay has gone beyond the world standard among the Iranians”.
In line with the lack of allocation of sufficient funds by the health system, participant 5 declared, “Currently, sufficient funds are not allocated by the government to provide oral and dental health services to the organizations”. Participant 9 also admitted, “The demand for health services has increased with the increase in the number of aging people and the increase in related health issues and the change in people’s lifestyles and eating habits”.
Regarding the lack of awareness and lack of priority to address the condition of the mouth and teeth, participant 2 added, “Due to the increase of chronic diseases in old age and their dissatisfaction with the quality of life, and despite the expensive conditions, the priority of aging people is to pay attention to food, clothing, and the like rather than paying attention to oral and dental health”. Participant 4 also mentioned, “Since there is not enough information about dentistry for older people, most of the aging people think that they will receive a prosthesis after losing a tooth and do not need any other care”.
Solutions for Providing Oral and Dental Health Services for Older People
Developing Guidelines and Specialized Instructions for Providing Oral and Dental Health Services for Older People
The majority of the participants agreed that there is no need to have a new structure or process at different levels. As mentioned by participant 2, the health system does not have a special plan for the oral and dental health of older people; hence, a comprehensive program for the care of older people should be developed from the very beginning, a part of which is specially adapted to the oral and dental health of older people and at different levels, and trainings and the way to provide services and the like should be included in it. To implement this program, the necessary policies must be made and the necessary budget must be considered by the Ministry of Health, and the implementation guarantee must be taken and communicated to all levels. According to these instructions, which are compiled for different levels of service provision, services are presented from the beginning of entering the health center or home, in addition to focusing on the way of examination, screening, receiving advice, providing education according to the underlying diseases of older people. The free package includes a toothbrush, dental floss, and toothpaste containing fluoride, and in general, providing all the oral and dental services needed by older people and compiling and providing sufficient information on how to refer to comprehensive rural health service centers and city health centers/hospitals. Specialized clinics and hospitals should be provided as well.
Training and Empowering Health System Employees Regarding Providing Oral and Dental Health Services for Older People
According to the review of the experts’ opinions about human resources providing oral and dental health services to older people and considering the lack of staff training and experts and specialists who are aware of oral and dental health issues for older people and the lack of manpower, it is better to empower the existing forces to provide these services by using training. The majority believed that the existence of a person called a technician or dental hygienist or a person called a dental hygienist at the initial levels of service provision, especially level one, including health houses and comprehensive urban and rural health service centers, is essential. For example, in this regard, participant 2 indicated that “Oral and dental hygiene can perform specialized tasks and tasks such as tooth extraction, caries treatment, medicine prescription, and the like. The level of education of these people can be improved to provide specialized services. In addition, forces such as health workers at the lower levels of services can provide services for training and referrals; even with the necessary training in the field of dentistry, they can prescribe painkillers for toothaches and the like”.
Training and Employing Experts in the Field of Oral and Dental Health for Older People (e.g., Children’s Dentists)
In addition to the cases mentioned about the staff providing services in the previous section, according to the opinions of several experts in the field of geriatrics and management, it is necessary to use dental specialists for older people to provide oral and dental services to this group, especially at higher levels. It has been stated that general dentists who are at the second level or higher should also attend dental courses for older adults. In this regard, participant 4 declared, “People who have a dental fellowship for older people and people who are psychologically familiar with the states and behaviors of older people should work at higher levels to provide oral and dental services to older people”. In addition, participant 9 added, “In addition to general and specialized dentists, there should be dentists with a specialized course for older people to provide services for older people”. Further, participant 11 mentioned that “It is better for people specializing in geriatrics to enter the work”.
Increasing Insurance Coverage of Oral and Dental Health Services for Older People
Due to the high costs of dental services, lack of adequate insurance coverage, many economic and social problems for this group, low financial ability, inadequate income status, and increasing need for dental services with age, the insurance system should be strengthened and reformed. Further, a separate budget should be considered by the health system for providing services, and oral and dental services should be covered through basic insurance. Furthermore, the supplementary part of services and the costs should be supported and covered by supplementary insurance. According to the opinion of participant 2, “The provision of basic services in health centers should be covered by insurance, and an insurance allowance should be considered for aging people’s artificial teeth.” Furthermore, according to the opinion of participant 4: “Subsidies should be provided by the government through supplementary insurance for older people, or a separate fund or budget should be considered for this age group”.
Developing Coherent and Effective Monitoring and Evaluation Programs for Oral and Dental Health Services Provided to Older People
According to the opinion of most participants, it is possible to evaluate the quality and quantity of providing oral and dental health services at different levels using appropriate indicators that have been compiled in this regard and provided to different centers. It is important to develop indicators that measure both system performance and individual performance of people at different levels of service delivery. Depending on the interviewees’ opinions, there are several methods for checking the quality and quantity of services provided, including checklists during the initial examination and indicators for verification. Participant 2 stated, “There must be a special checklist for the initial assessment of older people upon entering the center. In addition to quantitative indicators (process, output, and impact indicators) to check the quality and quantity of services, it is possible to use qualitative indicators such as quality of life related to mouth and teeth and indicators that are measured by questionnaires, such as oral and dental hygiene behaviors in older people”. According to participant 4, “A monitoring protocol should be developed for each service delivery unit, and people who are at different levels of service delivery should perform the control and evaluation process; for example, at the levels of a service provision, checklists should be provided for teaching how to use a toothbrush and dental floss and how to care for teeth”.
Improving the Position of Oral and Dental Health Services for Older People in Primary Health Care and Referral System
According to the items extracted from the interviews, the people involved in providing dental services believed that the health system does not have a special program or guideline for the oral and dental care of older people. Moreover, they indicated that there is not even a separate curriculum for dentistry for older people, and services are provided only in the small area of the dentist’s information for older people, while the pharmaceutical and medical conditions of older people are different. The referral system needs to be reinforced, and the dental referral system for older individuals needs to be activated on all levels. There should be a specific plan for referring older individuals. According to interviewee 2, “A comprehensive healthcare plan for older people should be written, with a section dedicated to mouth and teeth, and the necessary policies should be explained, the referral system should be strengthened, and after the initial examination and training, referrals should be made if necessary”.
Providing Suitable Service Packages for Different Levels of Service Provision
According to the analysis of the opinions of the participants, the majority agreed with the provision of educational and preventive services as well as the provision of simple and routine dental services needed for older people at level one. Routine dental services such as simple and advanced restorations, denervation, provision of simple prostheses, dental radiography, tooth extraction, scaling, provision of preventive measures, and necessary health recommendations should be followed at levels one and two. Other routine dental services included the diagnosis of simple caries, written education for older people, regular follow-ups of older people, referral to a dentist, provision of painkillers for toothache, screening, visit and examination, and provision of nutrition advice for older people. However, according to one of the participants, the specialized services for older people, which are the services that should be provided according to their physical and mental conditions at level three, do not exist in Iran, and the services provided at this level are limited to the provision of specialized dental services such as prosthetics, implants, and specialized prosthetic care. According to interviewee 9, “The service package should be defined for different levels of service provision and users”.
Providing Oral and Dental Health Services to Older People on the Part of Various Organizations
The health system alone is unable to provide oral and dental services to older people, and there should be organizations to participate in providing services to this group. Organizations such as charitable organizations, non-governmental welfare organizations, and retirement centers should play a role in providing services to older people, and organizations such as insurance organizations, relief committees, and non-governmental organizations should play a role in financial support. The dental schools of the country should play a significant role in training dentists regarding the oral and dental health of older people, streamlining the process of providing services, and creating a culture to create community-oriented dentistry. Additionally, according to participant 9, “Dental associations should be involved in providing training courses to providers regarding geriatric dentistry and supporting this vulnerable group”.
Discussion
Challenges of Providing Oral Health Services to Older People
The high rate of the use of artificial teeth with very high costs, the provision of dental services mostly by the private sector and in the office, the lack of proper insurance coverage, and the lack of an integrated structure to provide services to older people are the challenges of the health system and older people in providing and receiving oral and dental services. According to studies performed by Jones and Webb et al, most of the treatments are provided in the private sector and private dentists’ offices and are paid out of pocket, and the remaining treatments are provided in clinics and public hospitals.16,17 Based on the results of a study conducted by Ástvaldsdóttir et al, it has been observed that dental providers and other healthcare professionals need to have more knowledge about the oral health of older adults. Oral hygiene is not always included in undergraduate education programs for healthcare professionals or nursing and healthcare assistants.18
Older people are confronted with problems such as a high percentage of tooth loss, poor health conditions and decay, and issues with oral and dental health. According to a study performed by Helgeson and Glassman, it was revealed that aging people suffer proportionally from active and untreated oral infections, tooth loss, old age, and inappropriate dentures, and there are disorders in oral saliva, especially in those living in long-term care centers.19 Based on the findings of a study conducted by Griffin et al, it is clear that aging people may have more problems achieving effective interventions for the prevention and control of oral and dental disease than other people. The lack of insurance is a major obstacle that needs to be overcome, causing adults to pay more of their dental expenses out of pocket as they get older.20
Solutions for Providing Oral and Dental Health Services for Older People
Presenting Guidelines and Specialized Instructions for Providing Oral and Dental Health Services for Older People
There must be a written program, guidelines, and instructions for providing services and training at all levels, and all oral and dental disease prevention services should be provided at the centers where older people go to receive oral and dental care services. In a study conducted by Griffin et al, it was stated that every person in a nursing home should have a daily oral and dental care plan based on the level of oral and dental disease they have, and their ability to implement such a Framework should be independently regulated. In addition, the necessary care should be provided by the caregiver in the nursing home, or the necessary training should be provided to older people to do so.20 According to a study performed by Ghezzi et al, new integrated care models must include oral health expertise in a comprehensive set of services with different specialties, especially because people who report poor health are significantly more likely to have multiple chronic diseases.21
Training and Empowering Health System Employees Regarding Providing Oral and Dental Health Services for Older People and Training and Employing Experts in the Field of Oral and Dental Health for Older People (e.g., Children’s Dental Specialists)
Examining the experts’ opinions about the manpower to provide oral and dental health services to older people showed the lack of staff training and the lack of experts and specialists who are aware of the oral and dental health issues of older people and the lack of manpower and the absence of geriatric dental specialists. According to a report conducted by Moffett, when treating older people, dentists should take into account that this population usually has physical problems and may have received long-term care in a facility. Therefore, it is important to pay attention to and know about the physical condition of the person to treat oral and dental problems of older people. In addition, the findings of this study revealed that the correct treatment of patients is teamwork, which requires a dentist, dental hygienist, dental assistant, and center staff.22 Further, based on the findings of Shigli et al, training of staff (non-dentists) in dental care for older people should be provided so that they can help in oral health education, tooth decay prevention, oral cancer screening, and the like.23 The results of a study performed by John et al demonstrated that healthcare providers and caregivers should be trained at all levels.24 The government should provide the necessary support for dental teaching and research for older people, and geriatrics and geriatric care specialists should be trained and created to provide better services.25,26
Increasing the Insurance Coverage of Oral and Dental Health Services for Older People
Due to the high costs of dental services and the lack of adequate insurance coverage to provide these services for older people, the insurance system should be strengthened and improved. In most countries, such as Denmark, Sweden, Norway, England, and Germany, the private sector and private insurance are responsible for funding for oral and dental services rather than a combination of national medical insurance and private insurance. However, the coverage of services by national and government medical insurance is limited and leads to preventive and simple repair services, and other specialized services are covered by private insurance, imposing extensive costs on low-income and middle-income people.27 However, it is suggested that most preventive and routine dental services that are at the initial levels of service provision be covered by insurance or refer people to receive services at centers that are covered by insurance, and the government should pay most of the costs of prevention and routine oral and dental services for older people.
Developing Coherent and Effective Monitoring and Evaluation Programs for Oral and Dental Health Services Provided to Older people
According to the results of the studies, it is expected that a series of guidelines should be set for oral and dental health experts and dentists to control and monitor the services provided to older people, and these people should perform their duties based on these guidelines. The existence of the surveillance system varies depending on the factors of different countries, and most countries are moving toward reducing surveillance (e.g., in Arizona, in 2004, an agreement for the practice of dental hygienists and dental hygienists established specific regulations). In this agreement, the steps of treatment and provision of services, referrals, and follow-up care protocols have been specified, and permanent instructions have been prepared that the dentist must follow.28 The findings of a study conducted by De Visschere et al revealed that indicators of structure, process, and impact should be used to monitor the implementation of oral health guidelines for older people in nursing homes in the healthcare process. Structural indicators demonstrate whether oral healthcare is well integrated into the healthcare process. Process indicators are related to oral healthcare programs for older people. Impact indicators provide information about the outcome of the oral health protocol (e.g., the amount of oral plaque in older people).29
Improving the Position of Oral and Dental Health Services for Older people in Primary Healthcare and Referral System
According to the cases extracted from the interviews, the health system for the mouth and teeth of older people does not have a special program or guideline, and services are provided only in the small area of the dentist’s information for older people. There is not even a specific referral system for dentistry for older people. According to the report of the World Health Organization in 2005, the appropriate oral health policy should use appropriate strategies for older people and prioritize health education for these people, and by informing other non-dentist professionals, consider them as an integral part of the health of older people. Moreover, based on a study conducted by Griffin et al, the suggested public health priorities included better integration of oral and dental hygiene in medical care, implementation of community programs to promote healthy behaviors, and access to prevention services in the form of a comprehensive strategy to meet the oral and dental health needs of older people.20 The results of a study performed by Ástvaldsdóttir et al highlighted the need to organize dentistry for older people and clarify its place in the care chain.18
Providing Suitable Service Packages for Different Levels of Service Provision
Based on the findings of the interviews conducted with experts, all oral and dental disease prevention services should be provided in centers where older people go to receive oral and dental care services. Furthermore, other specialized services, such as dental restoration services, prosthetics, which is the basic need of older people due to the high rate of tooth loss, preventive services, surgery, implants, and other specialized services needed by older people at different levels of prevention, should be provided to them. According to a report performed by Moffett, one of the important factors that plays a role in meeting the dental needs of older people is the lack of programs that support prevention and oral health education for this population. Although there have been advances in prevention education over the past years, there is still a need for them among older people.22 In this regard, a study conducted by Nihtilä et al pointed out the importance of preventive interventions and counseling regarding oral health to service recipients and providers.30 According to a report in 2015 from Australia, it is suggested that screening should be performed not only in centers where a person goes to receive oral and dental services but also in public centers and hospitals where a person goes to receive non-dental services.31
Providing Oral and Dental Health Services to Older People on the Part of Various Organizations
To impose a financial burden on low-income seniors, it is recommended that the organizations that provide dental services to older people be in contact with non-governmental organizations to start public-private partnerships. This is because the health system alone is unable to provide oral and dental services to older people, and there must be organizations to participate in providing services to this group. Services provided by dental colleges should be distributed to rural and low-income areas; even oral care services for older people can be distributed by state governments and dental colleges (according to a study by Shigli et al in India) (e.g., the Karnataka state government provides free dentures for those below the poverty line above 60 years of age). Public sector employees also identify needy senior citizens and connect them with dental schools, and the government pays a set amount to the dental school.23 Based on the preliminary results of the literature review and researchers’ experiences, the present study, to the best of our knowledge, was the first to specifically and scientifically discuss the challenges of providing oral and dental health services for older people in Iran. However, the lack of access to several experts and senior officials due to busy work despite numerous follow-ups was the most important limitation of this study.
Conclusions
The present study collected and analyzed data on the challenges and solutions of providing healthcare services to older people through interviews. The findings could provide comprehensive and extensive information in various fields to other people and should be used by managers and policymakers to formulate a coherent program to provide oral and dental health services to older people and provide the basis for improving the oral and dental health status of older people. The results revealed that there are no effective plans and policies to provide oral health and dental services to older people. Moreover, it was found that the provision of oral and dental health services to older people is facing many challenges, and the focus should be on prevention issues, education, and the provision of optimal services to older people according to their special conditions and the employment of dental specialists for older people
Acknowledgments
We would also like to appreciate the full cooperation of the university officials. We also thank the interviewees for their participation.
Author contributions
Conceptualization: Saber Azami-Aghdash, Shima Rastkar-Gharamaleki.
Data curation: Saber Azami-Aghdash, Shima Rastkar-Gharamaleki.
Formal analysis: Saber Azami-Aghdash,Shima Rastkar-Gharamaleki, Mahdieh Asghari.
Funding acquisition: Saber Azami-Aghdash, Shima Rastkar-Gharamaleki.
Investigation: Saber Azami-Aghdash,Shima Rastkar-Gharamaleki, Mahdieh Asghari, Mehdi Rostampour.
Methodology: Saber Azami-Aghdash, Shima Rastkar-Gharamaleki, Mahdieh Asghari, Mehdi Rostampour, Elahe Safari.
Project administration: Saber Azami-Aghdash,Shima Rastkar-Gharamaleki.
Resources: Saber Azami-Aghdash, Shima Rastkar-Gharamaleki.
Supervision: Saber Azami-Aghdash.
Validation: Saber Azami-Aghdash, Shima Rastkar-Gharamaleki, Mahdieh Asghari, Mehdi Rostampour, Elahe Safari, Shahin Karami.
Visualization: Shima Rastkar-Gharamaleki, Mahdieh Asghari.
Writing–original draft: Saber Azami-Aghdash, Shima Rastkar-Gharamaleki, Mahdieh Asghari.
Writing–review & editing: Saber Azami-Aghdash, Shima Rastkar-Gharamaleki, Mahdieh Asghari, Shahin Karami.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethical approval
Informed consent was obtained from all participants. The interviews were conducted after completing the informed consent form and were analyzed anonymously. All the study procedures were conducted in accordance with the accepted ethical standards. The work was approved by the Ethics Committee of Tabriz University of Medical Sciences (Code: IR.TBZMED.REC.1398.1013).
Consent for publication
Not applicable.
Conflict of interests
The authors declare that there is no conflict of interests.
Supplementary files
Supplementary file 1. Interview Question.
(pdf)
References
- Safiri S, Motlagh Asghari K, Sullman MJ. The global burden of diseases and injuries among older adults. Int J Aging 2023; 1:e16. doi: 10.34172/ija.2023.e16 [Crossref] [ Google Scholar]
- Khodabakhshi-Koolaee A, Heidari F, Zangeneh Motlagh F. The effect of mixed prayer and positive psychology group therapy on life meaning and death anxiety among elderly women with physical-motor disabilities. J Res Relig Health 2018;4(2):16-28. [Persian].
- Aminisani N, Azimi-Nezhad M, Shamshirgaran SM, Mirhafez SR, Borji A, Poustchi H. Cohort profile: the IRanian Longitudinal Study on Ageing (IRLSA): the first comprehensive study on ageing in Iran. Int J Epidemiol 2022; 51(4):e177-88. doi: 10.1093/ije/dyab272 [Crossref] [ Google Scholar]
- Sabatini S, Wahl HW, Kaspar R, Huntley J. International evidence on predictors and outcomes of awareness of age-related change. Front Psychiatry 2023; 14:1128531. doi: 10.3389/fpsyt.2023.1128531 [Crossref] [ Google Scholar]
- Bakker MH, Vissink A, Spoorenberg SLW, Wynia K, Visser A. Self-reported oral health problems and the ability to organize dental care of community-dwelling elderly aged ≥ 75 years. BMC Oral Health 2020; 20(1):185. doi: 10.1186/s12903-020-01175-7 [Crossref] [ Google Scholar]
- Jahangiry L, Bagheri R, Darabi F, Sarbakhsh P, Naghibi Sistani MM, Ponnet K. Oral health status and associated lifestyle behaviors in a sample of Iranian adults: an exploratory household survey. BMC Oral Health 2020; 20(1):82. doi: 10.1186/s12903-020-01072-z [Crossref] [ Google Scholar]
- Bolukbasi G, Dundar N. Oral health in older adults: current insights and tips. J Gerontol Geriatr 2024; 72(2):96-107. doi: 10.36150/2499-6564-n700 [Crossref] [ Google Scholar]
- World Health Organization (WHO). Ageing and Health. Available from: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health. Accessed February 5, 2018.
- Heidarpoor P, Tajary M. Evaluating oral and dental health and the related factors regarding the elderly in Aliabad city of Golestan province in 2022. The Journal of Tolooebehdasht 2024; 22(6):15-29. doi: 10.18502/tbj.v22i6.15208.[Persian] [Crossref] [ Google Scholar]
- Kosari M, Hoseini Z, Golrizi F. The investigation of oral and dental status and its related factors in the elderly in Torbat Heydariyeh in 2015. J Torbat Heydariyeh Univ Med Sci 2016;4(2):39-44. [Persian].
- Mohammadpour M, Bastani P, Brennan D, Ghanbarzadegan A, Bahmaei J. Oral health policymaking challenges in Iran: a qualitative approach. BMC Oral Health 2020; 20(1):158. doi: 10.1186/s12903-020-01148-w [Crossref] [ Google Scholar]
- Aryan Kya M, Rojhanian T, Sayar Irani F. Exploring factors shaping dental insurance utilization: insights from an investigation in Iran: dental services utilization factors in Iran. J Dent Sch 2023; 41(4):133-9. doi: 10.22037/jds.v41i4.44451.[Persian] [Crossref] [ Google Scholar]
- Henderson E, Rubin G. A model of roles and responsibilities in oral health promotion based on perspectives of a community-based initiative for pre-school children in the UK. Br Dent J 2014; 216(5):E11. doi: 10.1038/sj.bdj.2014.196 [Crossref] [ Google Scholar]
- Poudel P, Paudel G, Acharya R, George A, Borgnakke WS, Rawal LB. Oral health and healthy ageing: a scoping review. BMC Geriatr 2024; 24(1):33. doi: 10.1186/s12877-023-04613-7 [Crossref] [ Google Scholar]
- Kim H, Sefcik JS, Bradway C. Characteristics of qualitative descriptive studies: a systematic review. Res Nurs Health 2017; 40(1):23-42. doi: 10.1002/nur.21768 [Crossref] [ Google Scholar]
- Jones JA. Financing and reimbursement of elders’ oral health care: lessons from the present, opportunities for the future. J Dent Educ 2005; 69(9):1022-31. [ Google Scholar]
- Webb BC, Whittle T, Schwarz E. Provision of dental care in aged care facilities, NSW, Australia - part 1 as perceived by the directors of nursing (care providers). Gerodontology 2013; 30(3):226-31. doi: 10.1111/j.1741-2358.2012.00670.x [Crossref] [ Google Scholar]
- Ástvaldsdóttir Á, Boström AM, Davidson T, Gabre P, Gahnberg L, Sandborgh Englund G. Oral health and dental care of older persons-a systematic map of systematic reviews. Gerodontology 2018; 35(4):290-304. doi: 10.1111/ger.12368 [Crossref] [ Google Scholar]
- Helgeson M, Glassman P. Oral health delivery systems for older adults and people with disabilities. Spec Care Dentist 2013; 33(4):177-89. doi: 10.1111/scd.12038 [Crossref] [ Google Scholar]
- Griffin SO, Jones JA, Brunson D, Griffin PM, Bailey WD. Burden of oral disease among older adults and implications for public health priorities. Am J Public Health 2012; 102(3):411-8. doi: 10.2105/ajph.2011.300362 [Crossref] [ Google Scholar]
- Ghezzi EM, Kobayashi K, Park DY, Srisilapanan P. Oral healthcare systems for an ageing population: concepts and challenges. Int Dent J 2017; 67(Suppl 2):26-33. doi: 10.1111/idj.12343 [Crossref] [ Google Scholar]
- Moffett F. Taking Care How Dentists Should Prepare for Treating Aging Patients. Academy of General Dentistry; 2016. Available from: https://www.agd.org/docs/default-source/policies-and-white-papers/impact-and-gd-articles/taking-care-how-dentists-should-prepare-for-aging-patients.pdf?sfvrsn=2.
- Shigli K, Nayak SS, Nayak PP, Basavaraj A, Shivasakthy M. Innovative solutions to reform geriatric oral health in India: alliance for healthy aging. Indian J Community Health 2021; 33(1):222-5. doi: 10.47203/IJCH.2021.v33i01.033 [Crossref] [ Google Scholar]
- John J, Mani SA, Azizah Y. Oral health care in the elderly population in Malaysia--a review. Med J Malaysia 2004; 59(3):433-9. [ Google Scholar]
- Jiang CM, Chu CH, Duangthip D, Ettinger RL, Hugo FN, Kettratad-Pruksapong M. Global perspectives of oral health policies and oral healthcare schemes for older adult populations. Front Oral Health 2021; 2:703526. doi: 10.3389/froh.2021.703526 [Crossref] [ Google Scholar]
- Leung KC, Chu CH. Dental care for older adults. Int J Environ Res Public Health 2022; 20(1):214. doi: 10.3390/ijerph20010214 [Crossref] [ Google Scholar]
- World Health Organization (WHO). Global Oral Health Status Report: Towards Universal Health Coverage for Oral Health by 2030. WHO; 2022.
-
Naughton DK. Expanding oral care opportunities: direct access care provided by dental hygienists in the United States. J Evid Based Dent Pract 2014;14 Suppl:171-82.e1. doi: 10.1016/j.jebdp.2014.04.003.
- De Visschere LM, van der Putten GJ, Vanobbergen JN, Schols JM, de Baat C. An oral health care guideline for institutionalised older people. Gerodontology 2011; 28(4):307-10. doi: 10.1111/j.1741-2358.2010.00406.x [Crossref] [ Google Scholar]
- Nihtilä A, Tuuliainen E, Komulainen K, Autonen-Honkonen K, Nykänen I, Hartikainen S. Preventive oral health intervention among old home care clients. Age Ageing 2017; 46(5):846-51. doi: 10.1093/ageing/afx020 [Crossref] [ Google Scholar]
- Müller F, Shimazaki Y, Kahabuka F, Schimmel M. Oral health for an ageing population: the importance of a natural dentition in older adults. Int Dent J 2017; 67(Suppl 2):7-13. doi: 10.1111/idj.12329 [Crossref] [ Google Scholar]